Shilpi Padhi and Sonal Bhat*
Department Of Anaesthesiology Kasturba Medical College, Mangaluru Manipal Academy of Higher Education, Manipal
Corresponding Author E-mail : sonalbhat27@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1888
Abstract
Incidence of cough and sore throat post-extubation is known to be increased in cigarette smokers. Simple methods with minimal side-effects like application of 2% lignocaine jelly is observed to reduce such complications in the normal population. The rationale of this study is to directly compare such effects between smokers and non-smokers.It is an observational study including 60 participants aged between 20 to 60 years with ASA 1 and 2 physical status undergoing elective surgery under general anaesthesia. The patients were randomized in to two groups – smokers and non-smokers. Lignocaine 2% jelly was applied to endo-tracheal tube cuffs in both groups. Comparison was made between the two groups with regards to post operative cough and sore throat at intervals of 1 hour and 24 hours post extubation as well as hemodynamic variability at pre-induction, 3 mins, 15 mins post intubation and 3 mins post extubation. Students t-test, Fishers exact test and Mann-Whitney test was used for comparison between the two groups.1-hour sore throat was significantly lower in non-smoker group (p=0.000). However, incidence of 24-hour sore throat was comparable (p=0.104). The number and severity of cough was greater in smoker group, even after the application of 2% lignocaine jelly (p=0.003). There was no significant difference in hemodynamic variables pre and postoperatively.Noticeable difference was observed between smokers and non-smokers with regard to respiratory complications post-extubation. We must consider smoking as a public health hazard and effects of chronic smoking cannot be discounted when taking in to account benefits observed with lignocaine jelly on ET tube cuffs.
Keywords
Lignocaine; Smokers; Non-Smokers
Download this article as:| Copy the following to cite this article: Padhi S, Bhat S. An Experimental Study on Topical Application of 2% Lignocaine Jelly for Preventing Coughing and Sore Throat Post Extubation in Elective Surgeries in Smokers vs. Non-Smokers. Biomed Pharmacol J 2020;13(1). |
| Copy the following to cite this URL: Padhi S, Bhat S. An Experimental Study on Topical Application of 2% Lignocaine Jelly for Preventing Coughing and Sore Throat Post Extubation in Elective Surgeries in Smokers vs. Non-Smokers. Biomed Pharmacol J 2020;13(1). Available from: https://bit.ly/2Q73cuP |
Introduction
Endotracheal intubation causes airway mucosal inflammation and irritation. Occurrence of cough and sore throat post-extubation is known to be increased in cigarette smokers due to the loss of epithelial integrity. The aim of various anaesthetic providers is to reduce the complications of cough and increase post-operative patient comfort. Simple and easy methods with minimal side effects like application of local anaesthetics like lignocaine 2% jelly have been used for the same1. However, the impact of chronic smoking on this effect has been the topic of evaluation for years. Respiratory complications peri-operatively have been known to be trimmed down by the use of lignocaine applied topically to the airways exercising different administration techniques such as sprays, gels. During extubation as well as subsequently postextubation, for a period of 24 hours, coughing and sore throat is a crucial problem as seen in patients administered general anaesthesia.2,3 Some of the factors affecting the incidence of such sequel are endotracheal tube cuff size and design, use of lubricants, ease of intubation, age, gender and environmental factors such as cigarette smoking.4 A number of studies have analyzed the correlations of these factors with sequelae.5,6,7,8 The effectiveness of lignocaine has been studied to minimize the hemodynamic changes during extubation as well as prevention of post extubation cough and sore throat in various patients undergoing endotracheal intubation9,10. Improvement in endotracheal tube tolerance without compromising full emergence from general anaesthesia is ideal.11
Ranging from its impact on the hemodynamic parameters such as elevated blood pressure, heart rate, respiratory system such as its effect on the oxygen uptake and delivery as well as its interference with drug metabolism, smoking can cause a plethora of effects which serves as a challenge during general anaesthesia12. In this scenario, it becomes essential for studies show casing the contrast between smokers and non-smokers with regards to post-operative recovery following general anaesthesia. Many studies have analyzed topical or intravenous use of local anaesthetics and corticosteroids to reduce such complications separately for smokers and non-smokers, but not as a direct comparison. The study was conducted with the objective to compare the effectiveness of lignocaine 2% jelly in smokers vs. non-smokers to reduce post-extubation cough and sore throat, which is relevant given the widespread use and availability of lignocaine 2% jelly.
Materials and Methods
An experimental study, encompassing 60 patients scheduled for elective surgeries under general anaesthesia was conducted in hospitals of Kasturba Medical College, Mangaluru from December 2017 to August 2019 after Institutional Ethics Committee approval was taken. The study population was sub-divided in to two groups: G1 comprising of smokers and G2 comprising of non-smokers. They were aged between 20-60 years, of ASA 1 and 2 physical status who were able to comprehendand G1 group consisted of heavy smokers. Randomisation was done using computer generated randomisation. According to a study reported in the September issue of “International Journal of Environmental Researchand Public Health” 2013, heavy smoking was defined as “20 or more cigarettes per day, or 20 or more pack-years”13. A pack-year is calculated by “multiplying the number of cigarettes smoked per day by the number of years of smoking”14.
Patients at risk for difficult intubation, sore throat and chronic cough as well as those with respiratory ailments (like asthma) were excluded from the study.
A written, informed consent was obtained from all the patients after explaining the procedure. A pre-anaesthetic check up was done including detailed history and physical examination, baseline hemodynamic measurements and routine investigations.
Following administration of 1 mg midazolam and 2 microgm/kg fentanyl, patients were induced with 5mg/kg of thiopentone or propofol and 1.5 mg/kg succinylcholine or 0.5mg/kg atracurium. Intubation was undertaken using appropriately sized endotracheal tubes (ET). Anaesthesia was maintained with oxygen, nitrous oxide and inhalational agents such as sevoflurane with assisted ventilation.
A standard procedure of application of 2% lignocaine jelly on ET tube cuffs was carried out in both the groups. In both the groups, topical lignocaine was applied to attenuate airway responses during intubation. After the procedure, patients were extubated when they were fully awake and able to respond to verbal commands (eye opening or handgrip) and moved all four limbs. The pre-induction and post-induction vitals such as systolic, diastolic blood pressure and the pulse rate were noted. The observations were done at 3 and 15 mins post intubation as well as 3 mins post extubation. In the post-operative ward, episodes of coughing , sore throat and laryngospasm were noted
Severity of cough was assessed using 4-Point cough scale15 at intervals of 1 and 24 hours post extubation
0: patient did not display any cough (Nil)
1: patient exhibited short bursts of coughs with no discomfort (Mild)
2: patient exhibited cough for less then 5 seconds with discomfort (Moderate)
3: patient displayed cough for more then 5 seconds with bucking as well as acute discomfort due to irritation (Severe)
Post extubation, at intervals of 1 hour and 24 hours, sore throat was evaluated using 4- point scale15. 0: corresponding to no sore throat
1: corresponding to mild (raises concern only on asking)
2: corresponding to moderate (raises concern on their own)
3: corresponding to severe (hoarseness or voice change, associated with throat pain)
Additional side effects like vomiting and nausea were also noted.16
Statistical Analysis
SPSS (Statistical Package for the Social Sciences) version 17 was used to analyze the data. Multiple tests were used to assess the variables using students t-test, Fishers exact test and Mann-Whitney test. Statistical significance was established with p value<0.05.
Results
The mean age and weight in the patients of Group 1were 38.97±10.31 years and 70.40±10.29 kgs respectively and for Group 2 were 38.71± 9.27 years and 63.65± 10.02 kgs respectively.
The mean systolic, diastolic pressures and the mean heart rate in the pre-induction period in Group1 were 131.23±9.02 mmHg (Table 1), 81.77±4.58mmHg (Table 2) and 74.07±6.79 beats per minute (Table 3) respectively. The corresponding values in patients of Group 2 were 124.59±14.12 mmHg, (Table 1) 78.24±5.15 mmHg (Table 2) and 70.91±7.67 (Table 3) beats per minute respectively. The mean systolic, diastolic pressures and the mean heart rate at 3 minutes post intubation in Group 1 were 119.77±9.47 mmHg (Table1), 76.97±5.16mmHg (Table 2) and 68.90±5.86 beats per minute (Table 3) respectively. The corresponding values in patients of Group 2 were 114.35±13.37 mmHg (Table1), 73.71±5.35 mmHg (Table 2) and 66.09± 6.89 beats per minute (Table3) respectively. The mean systolic, diastolic pressures and the mean heart rate at 3 minutes postextubation in Group 1 were 123.93±9.01 mmHg (Table1), 80.13±5.26 mmHg (Table 2) and 70.67± 6.31 beats per minute (Table3) respectively. The corresponding values in patients of Group 2 were 118.18±13.26 mmHg (Table1), 77.41±5.05 mmHg (Table 2) and 67.21±6.50 beats per minute (Table 3) respectively.
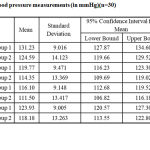 |
Table 1: Systolic blood pressure measurements (in mmHg)(n=30) |
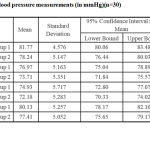 |
Table 2: Diastolic blood pressure measurements (in mmHg)(n=30) |
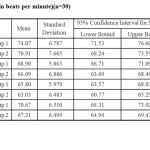 |
Table 3: Pulse Rate (in beats per minute)(n=30) |
The incidence of coughs was greater for smokers versus non-smokers (p=0.003). (Table 4) The cough was graded as mild, moderate and severe. Mild to moderate coughs were observed in 60% of smokers as compared to 61.8% in non-smokers. However, severe cough grading was observed in 33.3% of smokers as compared to 2.9% in non-smokers. The cough grading was higher in smokers versus non-smokers (p=0.001). (Figure 1) The incidence and severity of sore throat at 1 hour was higher in smokers compared to non-smokers (p=0.000) (Figure 2). Similarly, the incidence was comparable after 24 hours across both the groups (p=0.104). (Table 4) No incidence of laryngospasm, nausea and vomiting were observed.
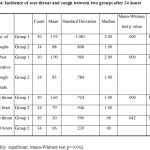 |
Table 4: Incidence of sore throat and cough between two groups after 24 hours |
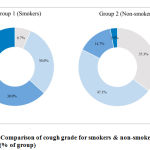 |
Figure 1: Comparison of cough grade for smokers & non-smokers groups (n = 30) (% of group) |
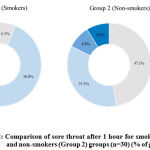 |
Figure 2: Comparison of sore throat after 1 hour for smokers (Group1) and non-smokers (Group 2) groups (n=30) (% of group) |
Discussion
Lignocaine has been used over the period of time in numerous ways to reduce the complications associated with endotracheal intubation in surgeries requiring general anaesthesia such as cough and sore throat. Some of the forms of administration of lignocaine are intravenous, aerosolized sprays, lubrication in the form of jelly or lignocaine inserted into the cuffs of endotracheal tubes. These methods have been compared in various studies but the key difference has not been established considering differences between smokers and non-smokers.
The main findings of the present study are that in smokers, respiratory complications such as cough and sore throat occur post-extubation in a greater degree vs. non-smokers. However, these complications are managed effectively by applying lignocaine jelly 2% on ET tube cuffs. As smokers are more prone to irritable airways, the prophylactic use of lignocaine jelly on ET tube cuffs before intubation is shown to have a greater influence in cutting down the incidence of complications in nonsmokers who are not exposed to the ill effects of smoking. We have delineated two separate groups G1including smokers and G2 including non-smokers in the study.
In our study, in group G2, 35.3% of the population had no cough post-extubation where as only 6.7% in group G1 were extubated without the incidence of cough. On the other hand, 33.4% of group G1 had severe cough. This is in accordance with a study conducted by Jawad et al1 which also compared the incidence of cough post extubation between smokers and non-smokers. The method used by Jawad et al1 was 0.5% lignocaine which was dropped into the tube continuously through out the procedure. 86% of smokers without intervention had cough whereas 30% in non-smokers. Within the smoker group, the incidence of cough was reduced to 35.2% with intervention of lignocaine thus implying that lignocaine installation has a positive effect on post-extubation sequalae. The Jawad et al study took into account only severe cough defined as more than 3 efforts and also included bucking as criteria. In contrast, our study outlines the implications on various grades of coughing. Lignocaine jelly is observed to reduce the severity as well as occurrence of cough in the normal population, however as we see it with regard to two specific groups, it doesn’t prove to be a significant tool to determine the effects of chronic smoking on airway complications during extubation.
In another study by Narimani et al28, the use of lignocaine gel applied over ET tube cuff was shown to have no role in moderating the incidence of cough and sore throat immediately after surgery. Our study demonstrates a clear benefit of 2% lignocaine jelly across both the groups, however the benefit was observed more in non smokers.
In another study (Ji won Lee et al29), no incidence of sore throat was observed in 42% of the sample population treated with lignocaine jelly. In our study, 47.1% of non-smokers had no sore throat after 1 hour with lignocaine jelly applied on ET tube cuffs. They however took into account the shape of the ET tube cuff which was tapered. In our study, the significance of the shape of the cuff was not established. Their sampling method did not account for the harmful impact of smoking which was done in our study.
The theory behind constant use of local anesthetic in order to block the tracheal nociceptive receptors has been helpful in diminishing incidence of sore throat. In our study, incidence of sore throat of moderate to severe degree was seen in 46.4% smokers and 17.6% nonsmokers 1 hour postsurgery. In a recent study by Navarro et al30, intra cuff lignocaine 4% showed unexpected results in preventing postextubation sore throat, where in no patients treated with lignocaine had evidence of sore throat as compared to intracuff normal saline in the control group. This study however, took into account ET tube cuff pressure as a higher pressure can increase morbidity. Intracuff lignocaine might be a superior technique to reduce postoperative respiratory
complications as outlined by their study in the general population. Their role with regard to smokers specifically remains to be studied and there is further scope of comparison with 2% lignocaine jelly.
In study by Soltani et al31, the number of coughs has been projected to be 3.6±0.1 after pre-treatment with 2% lignocaine jelly. Our study shows a marginal reduction of the number of coughs to 1.93±1.08 including the deleterious effects of smoking. On the other hand, significant improvement is observed in terms of reduction in number of coughs for non-smokers to 0.88±0.808.
In study by Basaranoglu et al32, use of 5% lignocaine jelly on ET tubes led to incidence of severe sore throat at 1 hour after surgery to be 12%. In our study, using 2% lignocaine jelly, shows the observed incidence to be 13.3% amongst smokers which was comparable to the previous study where in no specific differentiation within the study sample regarding smoking. In our study,in the non-smoker group, a clear benefit is observed with incidence of severe coughing being 8.8%. This reinstates the fact that 2% lignocaine jelly has a beneficial effect in reducing cough and sore throat postextubation drastically in nonsmokers.
It is advised to stop smoking eight weeks before surgery in optimum conditions. However, abstinence from smoking for 24 hours before surgery also has some impact in preventing cardio-vascular and respiratory complications of general anaesthesia in smokers. Smoking impairs the integrity of laryngeal epithelium causing inflammation and dysplasia thus leading to increased airway reactivity to mechanical and chemical stimulation. Hence, smokers are at a higher risk of exacerbated airway reflexes in the postextubation period. Higher incidence of laryngospasm and peri-operarative desaturation is observed in smokers leading to higher requirements for oxygen and analgesia as compared to non-smokers, post-operatively. To prevent these complications, 2% lignocaine jelly applied on ET tube cuffs is a standardized procedure in our institution.
Lignocaine targets the mucosa in contact with the endo-tracheal cuff and reduces tracheal stimuli. It induces anaesthetic action and increases tube tolerance in the patients.
We must consider smoking as a public health hazard and the effects of chronic smoking cannot be discounted when taking into account the benefits observed with lignocaine jelly on ET tube cuffs.
There is additional scope in exploring the comparative impact of other forms of lignocaine application in reducing postoperative complications for smokers and nonsmokers.
Conclusion
Our study has compared and shown a marked benefit in non-smokers with regard to post-extubation sore throat and cough as compared to smokers with application of 2% lignocaine jelly on endotracheal tube cuffs.
Acknowledgments
We would like to thank Kasturba Medical College, Mangaluru and Manipal Academy of Higher Education, Manipal, Karnataka, India for their support in conducting this study.
Conflicts of Interest
Nil
Funding Source
Nil
References
- Jawad M, Alsaady MA. Effect of Endotracheal Tube Lidocaine Instillation in Prevention of Smokers Emergence Coughing: Sample of Iraqi Patients Undergoing Emergency Appendectomy. J Intensive &Crit Care 2016;2(2):31-5.
- Stone DJ, Gal TJ. Airway management. In: Miller RD (ed): Anesthesia, 5th ed. Philadelphia: Churchill Livingstone Company;2000.1414-51.
- Endotracheal Anesthesia: II. Technical considerations. In: Collins VJ (ed): Principles of Anesthesiology. Philadelphia: Lea & Febiger;1993.518-59.
- Loeser EA, Kaminsky A, Diaz A, Stanley TH, Pace NL. The influence of endotracheal tube cuff design and cuff lubrication on post operative sore throat. Anesthesiology 1983;58(4):376-9.
- El Hakim M. Beclomethasone prevents postoperative sore throat. Acta Anaesthesiol Scand. 1993 Apr;37(3):250-2.
- Honarmand A, Safavi M. Bethamethazone inhaler versus intravenous lidocaine in the prevention of postoperative airway and throat complaints: a randomized, controlled trial. Ann Saudi Med. 2008 Jan-Feb;28(1):6-11.
- Canbay O, Celebi N, Sahin A, Celiker V, Ozgen, Aypar U. Ketamine gargle for attenuating postoperative sore throat. Br J Anaesth. 2008 Apr;100(4):490-3.
- Biro P, Seifert B, Pasch T. Complaints of sore throat after tracheal intubation: A prospective evaluation. Eur J Anaesthesiol. 2005 Apr;22(4):307-11.
- Mraovic B, Simurina T, Mikulandra, S, Seric, J, Sonicki, Z. Effects of IV lidocaine administered prior to extubation on early and late recovery after breast surgery; European Journal of Anaesthesiology. June 12 2010;27(47):4-8.
- Sitzman BT, Rich GF, Rockwell JJ, Leisure GS, Durieux ME, DiFazio CA. Local anesthetic administration for awake direct laryngoscopy. Anesthesiology 1997;86(1): 34-40.
- Navarro RM, Baughman VL. Lidocaine in the endotracheal tube cuff reduces post operative sore throat. J Clin Anesth. 1997 Aug;9(5):394-7.
- Rodrigo C. The effects of cigarette smoking on anesthesia. Anaesthesia Program 2000;47(4):143-150.
- Neumann T, Rasmussen M, Heitmann BL, Tønnesen H. Gold standard program for heavy smokers in a real-life setting. Int J Environ Res Public Health 2013 Sep 9;10(9):4186-99.
- Gillison ML, Zhang Q, Jordan R, Xiao W, Westra WH, Trotti A, Spencer S, Harris J, Chung CH, Ang KK. Tobacco smoking and increased risk of death and progression for patients with p16-positive and p16-negative oropharyngeal cancer. J Clin Oncol. 2012 Jun 10;30(17):2102-11.
- Fagan C, Frizelle HP, Laffey J, Hannon V, Carey M. The effect of intracuff lidocaine on endotracheal tube induced emergence phenomena after general anesthesia. AnesthAnalg. 2000 Jul;91(1):201-5.
- Estebe JP, Gentilli M, Le Corre P, Dollo G, Chevanne F, Ecoffey C. Alkalinization of intracuff lidocaine : efficacy and safety. AnesthAnalg 2005 Nov;101(5):1536-41.
- Budania LS, Chamala V, Rao M, Virmani S, Goyal KA, Nanda K. Effect of air, anesthetic gas mixture, saline, or 2% lignocaine used for tracheal tube cuff inflation on coughing and laryngotracheal morbidity after tracheal extubation. J Anaesthesiol Clin Pharmacol. 2018 Jul-Sep;34(3):386-391.
- Khan MA, Siddiqi KJ, Aqeel M. Lidocaine 4% spray is better than intracuff lidocaine 2% for reducing the incidence of post-extubation cough in patients undergoing total abdominal hysterectomy. Anaesth Pain & Intensive Care 2014;18(2):162-66
- Sumathi PA, Shenoy T, Ambareesha M, Krishna HM. Controlled comparison between betamethasone gel and lidocaine jelly applied over tracheal tube to reduce postoperative sore throat, cough, and hoarseness of voice. Br J Anaesth. 2008 Feb;100(2):215-8.
- Lam F, Lin YC, Tsai HC, Chen TL, Tam TW, Chen CY: effect of intracuff lidocaine on post operative sore throat and the emergence phenomena. PLoS One. 2015 Aug 19;10(8):e0136184.
- Snigdha RM, Alai T, Kumar V. Instillation of 4% lidocaine versus air in the endotracheal tube (ETT) cuff to evaluate post intubation morbidity-a randomized double blind study. J Anaesthesiol Clin Sci 2013;2:19-23.
- Wetzel LE, Ancona AL, Cooper AS, Kortman AJ, Loniewski GB, Lebeck LL. The effectiveness of 4% intracuff lidocaine in reducing coughing during emergence from general anesthesia in procedures lasting less than 1.5 hours. AANA J 2008 Apr; 76(2): 105-8.
- Zamora Lozano J, Cruz Villaseñor JA, Rodríguez Reyes J, Sánchez Rodríguez JP, Briones Corona G, Gallardo Alonso LA. Comparison of topical, intravenous and intracuff lidocaine for reducing coughing after extubation during emergence from general anaesthesia. Rev EspAnestesiolReanim. 2007 Dec;54(10):596-601. Spanish.
- Bousselmi R, Lebbi MA, Bargaoui A, Ben Romdhane M, Messaoudi A, Ben Gabsia A, Ferjani M. Lidocaine reduces endotracheal tube associated side effects when instilled over the glottis but not when used to inflate the cuff: A double blind, placebo-controlled, randomized trial. Tunis Med. 2014 Jan;92(1):29-33.
- D’Aragon F, Beaudet N, Gagnon V, Martin R, Sansoucy Y. The effects of lidocaine spray and intracuff alkalinized lidocaine on the occurrence of cough at extubation: a double-blind randomized controlled trial. Can J Anaesth. 2013 Apr;60(4):370-6.
- Singh AP, Jena SS, Meena RK, Tewari M, Rastogi V. Nebulised fentanyl for post-operative pain relief, a prospective double-blind controlled randomised clinical trial. Indian J Anaesth2013;57:583-6.
- Harding CJ, McVey FK. Interview method affects incidence of postoperative sore throat. Anaesthesia. 1987 Oct;42(10):1104-7.
- Narimani M, Mehdi SAS, Gholami F, Ansari L, Aryafar M, Shahbazi F. The Effect of Betamethasone Gel and Lidocaine Jelly Applied Over Tracheal Tube Cuff on Postoperative Sore Throat, Cough and Hoarseness. Journal of PeriAnesthesia Nursing 2016 August; 31(4):298-302.
- Lee Jiwon, Lee YC, Son JD, Lee JY, Kim HC. The effect of lidocaine jelly on a taper-shaped cuff of an endotracheal tube on the postoperative sore throat: a prospective randomized study. Medicine (Baltimore). 2017 Sep;96(37):e8094.
- Navarro L, Lima RM, Aguiar AS, Braz JR, Carness JM, Módolo NS. The effect of intracuff alkalinized 2% lidocaine on emergence coughing, sore throat, and hoarseness in smokers. Rev Assoc Med Bras (1992). 2012 Mar-Apr;58(2):248-53.
- Soltani HA, Aghadavoudi O. The effect of different lidocaine application methods on postoperative cough and sore throat. J Clin Anesth. 2002 Feb;14(1):15-8.
- Basaranoglu G, Erden V, Delatioglu H. Postoperative sore throat: effect of lidocaine jelly and pomade on endotracheal intubation. J Clin Anesth. 2004 Feb;16(1):79-80.








