Ashith M. V1, Utkarsh Mangal2, Ankita Lohia3 and Mithun. K4
1Department of Orthodontics and Dentofacial Orthopedics Manipal College of Dental Sciences, Mangalore, Manipal Academy of Higher Education Manipal, Karnataka, India
2Consultant Orthodontist, Jaipur, Rajasthan
3Consultant Orthodontist, 32 Dental Care and Orthodontic Specialty Centre Chawra Complex, Raniganj, Asansol, West Bengal
4Department of Orthodontics A.J Institute of Dental Sciences,Kuntikana,Mangalore, Karnataka, India
Corresponding Author E-mail: Utkmangal@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1821
Abstract
The main clinical and radiological defect in cleft maxilla is localised at the region of nasomaxillary complex and thereby the increased focus on maxillary interventional correction. During the period of development, the affected individual undergoes a series of periodic treatment approaches aimed towards normalisation of the function and aesthetics. However, such interventional procedures can have otherwise effects on the restriction of growth. Surgical and facial orthopaedic interventions can cause protrusion of the premaxilla. This influences the depth and height of the upper jaw and thus the total height causing clockwise rotation of the face. Similarly, the depth of the posterior maxilla is found to be reduced in CLP cases. The advancement of the anterior maxilla with callus distraction for correction of the cleft maxilla was first reported by KraKasis and Hadjipetrou in 2004. The technique has been used since then with variable success and less predictability. The present table clinic is targeted to showcase the key features of various stages critical in planning the anterior maxillary distraction in adult maxillary hypoplasia cases. The requirement of precision in planning and treatment is high in such cases to minimize the adverse effects. The novel methodology discussed here is the combination of CBCT, face bow transfer and stereolithography for surgical planning and simulation. With the use of CBCT diagnostic capacity is enhanced, enabling visualisation of the defect. It also helps to simulate surgical procedure virtually and/or with the application of stereolithography. Use of the face bow facilitates biomechanical planning. The registration of the maxillomandibular relation to the cranial base serves as a guide to position the distractor. This is a critical step, as it dictates the direction of the distraction force vectors. Precise orientation and planning enable predictable movement of the anterior maxilla and control the extent of anterior open bite opening, in most cases. This contrasts with the overbite created with counter clockwise jaw rotation, reducing the post distraction orthodontic management. This table clinic presentation also draws home the key points in identifying and mitigating the potential complications during and after the distraction. The use of the present methodology enables a predictive treatment outcome for the cases with minimal complications associated with distraction with a marked reduction in the magnitude of callus molding. Therefore, with the application of this novel clinical paradigm for AMD, a predictable result can be achieved, which helps in the reduction of the treatment time and gives a stable outcome.
Keywords
non-syndromic; radiological; stereolithography
Download this article as:| Copy the following to cite this article: Ashith M. V, Mangal U, Lohia A, Mithun K. Role of an Orthodontist in the Management of Cleft Maxilla With Anterior Maxillary Segmental Distraction (AMD)- A Clinical overview. Biomed Pharmacol J 2019;12(4). |
| Copy the following to cite this URL: Ashith M. V, Mangal U, Lohia A, Mithun K. Role of an Orthodontist in the Management of Cleft Maxilla With Anterior Maxillary Segmental Distraction (AMD)- A Clinical overview. Biomed Pharmacol J 2019;12(4). Available from: http://biomedpharmajournal.org/?p=29155 |
Introduction
Defining Cleft Maxilla
Cleft of the face can present as syndromic or a non-syndromic variant. Where the syndromic variant presents with a significant co-morbidity in multiple organs, the facial clefting presents with a varying magnitude in both types.
The cause for the occurrence of cleft lip and palate is multifactorial ranging from genetic factors to epigenetic influences. Based on the pattern of common presentation of the cleft palate has been classified as complete or incomplete, involving only palate or both palate and alveolar process.
The inevitable sequalae of the disorder is the significant retardation in the growth of the upper jaw with or without excessive growth of the mandible. The deficiency of the upper jaw in the adult individual forms a matter of serious concern having functional and aesthetic implications. This presence of a deficient maxilla is referred to as cleft maxillary hypoplasia or cleft maxilla.
Challenges associated
The main clinical and radiological defect is localised at the region of nasomaxillary complex and thereby the increased focus on the management of the defect by intervention at the maxilla. During the period of development, the affected individual undergoes a series of periodic treatment approaches aimed towards normalisation of the function and aesthetics. However, such interventional procedures can have otherwise effects on the restriction of growth1,2.
Surgical and facial orthopaedic interventions can cause protrusion and retroclination of the premaxilla. This influences the depth and height of the upper jaw and thus the total height causing clockwise rotation of the face. Similarly, the depth of the posterior maxilla is found to be reduced in CLP cases3.
Though multiple procedures are taken up to normalise the growth and development, the stigma of the cleft facies persists, in the backdrop of a hypoplastic maxilla. This demands a definitive surgical correction is restoring the near normal balance.
Defining AMD
The management of the hypoplastic defect has been a challenge to the reconstructive team. The conventional choices of maxillary osteotomy to address the craniofacial defects have had a variable rate of success, with relapse rates reported in literature 30-40%.4-7 This high percentage, with orthognathic surgery alone, can mostly be attributed to the varying magnitude of the defect and the specific problems associated, such as existing scarring from previous surgeries, the presence of pharyngeal flap and poor bone structure with reduced cortical thickness.8
The principles of distraction osteogenesis were reported as early in 1988 by Ilizarov9 and had been applied to correction of the compromised middle third of the face by several authors in the literature. 10-12
The advancement of the anterior maxilla with callus distraction was first reported by KraKasis and Hadjipetrou in 2004.13
AMD versus Lefort I Maxillary Osteotomy
Orthognathic surgery with Lefort I maxillary advancement has been the conventional standard method for addressing the hypoplastic defect.14 Other than osteotomy, Lefort I distraction osteogenesis (DO) has also been undertaken when the sagittal discrepancy is considered beyond the envelope of surgical repositioning alone. This has the limitation of the Lefort I osteotomy has been attributed to the contraction of the maxillary palatal mucosa and the associated scarring. 15,16
In Le Fort I DO, subperiosteal Le Fort I osteotomy is done followed by gradual rhythmic separation of bone using a fixed distractor device. This allows the filling of the gap created during the physiological healing and hence effectively lengthening the bone.9 However, for the patients of maxillary hypoplasia with repaired cleft palate, the bony defect may be addressed, but the functionality of the speech proves challenging. Earlier studies in the literature have reported the risk for velopharyngeal insufficiency (VPI) with same risk magnitude with Lefort I osteotomy and distraction, as the soft palate gets farther away from posterior pharyngeal wall17. This insufficiency can lead to further deterioration of the speech function of the patient.18
Anterior maxillary segmental distraction osteogenesis (AMSDO) has surfaced as the technique of choice in the literature for correction of the maxillary hypoplasia13,16,19-21The differences between AMSDO, and Le Fort I DO are mainly in the speech change and the surgical security.20
Planning for AMD
Hanson and Melugin22 described the role of an orthodontist in mandibular distraction osteogenesis divided into three temporal phases viz. (1) pre-distraction treatment planning and orthodontic preparation, (2) orthodontic therapy during distraction and consolidation, and (3) post-consolidation orthodontic management. Similar considerations are involved in preparation for the AMSDO which can be discussed here with the emphasis on diagnostic evaluation.
Diagnostic considerations and Pre-surgical orthodontic planning
The familial nature of facial clefting makes it imperative to acquire a thorough history of the presenting disorder. In addition, it is also necessary that a detailed treatment history is obtained from the patient because the various treatments undertaken throughout the period of development. Special attention is also often advised to the psychological history, which contributes to gauging patient’s expectations from the orthodontic therapy.
The diagnostic approach is essentially like orthodontic diagnostic and treatment planning protocol. A complete extra oral and intra oral assessment with suitable photographic records with the impressions is made.
Functional diagnosis is of special significance and emphasis should be placed on obtaining centric relation with a facebow transfer. This provides the dual benefit of firstly, a total overview of the occlusion in the patient’s craniomandibular relation and secondly, assists in planning the positioning of the distractor during appliance design and fabrication.
Imaging both 2D and 3D are necessary in the precise planning of the case.(Fig. 1 )
 |
Figure 1: A-F: 3D reconstructive view of the cleft maxilla case showing severe arch constriction and misalignment of the dentoalveolar units. |
Cone Beam CT (CBCT) forms an essential diagnostic aid in such cases. The use of 3D imaging equips the orthodontist and the oral surgeon with comprehensive structural anatomy. This is facilitated by the use of stereolithography and rapid prototyping to conduct a simulation of osteotomy and appliance placement.
CBCT assists orthodontically by giving the 3D orientation of the dental units, including impacted teeth and altered root anatomy such as dilacerations. It also helps to assess the bone density and the possibility of an alveolar bone graft following expansion. Care should be given in prescribing the type of scan, with a high definition full field of view (FOV) scan fulfilling the as low as diagnostically acceptable (ALADA) criteria. If a low dose scan is taken, 3D printing of the models becomes questionable due to high noise density in such scans.
Digital Lateral cephalogram and panoramic radiographs are also obtained pre treatment. While Lateral cephalometric analysis can be made from reconstructed cephalogram from the CBCT, a separate OPG is required. This forms the base line for reliable comparison of mid treatment changes and treatment progress, eliminating the need to repeat a high exposure CBCT scan.
Presurgical orthodontics
The requisite prior to surgery is a well aligned arch with well-established width and form. Therefore, its imperative to assess the transverse relations between the arches and within the arch. With the presence of multiple misaligned and ectopically placed teeth, the alignment to overcome interferences becomes a critical step. Severely crowded or impacted teeth should be carefully evaluated, and the decision to extract should be deferred until the establishment of form and width.
Maxillary arch expansion is a crucial step, especially in cases of cleft lip and palate as the foci of defect lie in the palate. The need for expansion is based on the arch structure and inter arch relationship in present occlusion and the predictive post-surgical occlusion. This should be observed and planned with the help of plaster models and CBCT scans with or without treatment simulations.
A contoured and stable arch form provides improved post surgically stability, hence is always methodically planned. The expansion in cleft lip and palate is met with certain challenged in the selection and design of expansion appliance. This occurs mostly due to the skewed and asymmetric arch forms. Commonly recommended appliances for transverse palatal expansion include NiTi Palatal Expander, V-shape expander and Quad helix with or without modifications. (Fig 2a-i)
 |
Figure 2: a-d: pre-treatment intra oral records e-g: initial alignment stage with HANT wire, 3h; use of NiTi expander for arch expansion3l, Nasomaxillary fistula formation seen following expansion |
A sequalae of the arch expansion can be the opening of the alveolar cleft defect or palatal nasomaxillary fistula. (Fig 2i) Based on the severity and magnitude of the defect and presence or absence of impacted canine, the need for an alveolar bone graft is established. The mucosal fistula is also addressed at this stage. (Fig 3 a-d) The advantage with achieving arch expansion is the increment in arch length, which now can be potentially used to align the severely crowded teeth and bring previously impacted teeth into alignment.
The goal at this stage is to achieve a stable occlusal table with well-established arch form. (Fig3e-h)
Surgical Preparation
To facilitate the surgery, based on the osteotomy cuts planned, the root orientation of the teeth adjacent to the surgical site is changed. The positioning of the roots in a divergent pattern is done to avoid any inadvertent damage due to surgical cut. This can be achieved by bracket reorientation or v-bend in the arch wire creating a symmetric geometry.
It is important to note that the lower arch alignment and plane should be addressed to simultaneously. To best orient, the post-surgical maxilla, the curve of spee should be levelled.
Distractor placement
An important step in this stage is to achieve a craniomaxillary correlation, as mentioned earlier, with the use of face-bow and articulator. This will best orient the maxilla and assist in positioning of the distractor device parallel to it. The distractor used is the HYRAX design with the screw oriented anterioposteriorly.(Fig3i)
 |
Figure 3: a-d, surgical correction of the nasomaxillary fistula e-h, complete alignment of the arch prior to surgery i-k, consolidation of the dentoalveolar units |
l, distraction appliance in place
The position of the device is critical in deciding the force vectors from the active distraction force.
For an ideal distraction setting, the line of force must pass through the centre of resistance (Cres) of the jaw. However, as the distractor is placed intraorally, the distance between the Cres and the line of force creates a counterclockwise rotational movement23. (Fig 4) Therefore, the orientation of the distractor device must be done parallel to prevent the same. Simulation of the distraction model, digital or on the models provides improved precision by mimicking the immediate impact of the force magnitude and direction.
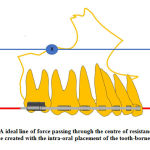 |
Figure 4 : A ideal line of force passing through the centre of resistance (X) B, a line of force created with the intra-oral placement of the tooth-borne distractor |
Prior to surgery, the consolidation of the dental units of the two, planned osteotomized segments must be done. This preserves the alignment of the teeth during the courses of distraction under the increased tensile forces.(Fig3i-l)
Following a consolidation period of six weeks, the distractor device is activated with a rate of 0.5mm/turn for a rhythm of twice a day.
Post-surgical management
Settling the occlusion
Postsurgical orthodontic treatment should be aimed at acceptable overbite and overjet with tight intercuspation of teeth. The phenomenon of postsurgical accelerated orthodontic tooth movement could be caused by the improvement in dental and muscular function postoperatively or the changes in bone physiology and metabolism induced by orthognathic surgery as proposed by Liou et al25.
The orthognathic surgery triggers 3 to 4 months of higher osteoclastic activity and metabolic changes in the dentoalveolar complex postoperatively, which may accelerate postoperative orthodontic tooth movement.
 |
Figure 5: a-c, placement of the distractor device in antero-posterior orientation on the face bow transferred and articulation. d-f, simulation of the distraction to assess the parallelism |
 |
Figure 6: a-d, Post-distraction intra-oral photographs |
The newly formed soft bone after distraction could be molded by using inter arch elastics to achieve better interdigitation of teeth26.
Attending to the AOB
Anterior open bite is a complication which can be controlled using intermaxillary elastic bands on the anterior dental arch to prevent the cranial dislocation of the distracted segment. This might be due to the high friction at the site of horizontal osteotomy at the maxilla, and the rigid distractor is required for preventing the rotation. Another possible prevention method would be the use of bone-borne distractor instead of the tooth-borne distractor.
Finishing and retention
Distraction osteogenesis gradually lengthens both the bones and the soft tissues, then greatly lowers the soft tissue restriction around the distracted segment and lowers the relapse rate by 5.56%–10%27. Relapse after anterior maxillary distraction can still occur in patients with cleft lip and palate if a retention appliance in the form of tooth replacement is not performed28. A modified nance palatal bar can be used to retain the amount of distraction (Fig7)
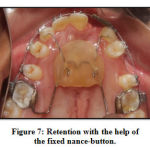 |
Figure 7: Retention with the help of the fixed nance-button. |
Timing
Timing and the rate of distraction are important for new bone formation in DO. Distraction rate that is too quick can lead to non union. On the other hand, if the bone is distracted too slowly, it might lead to early fusion. After a latency period of one week, the appliance was activated at a rate of 1 mm per day, using five rhythms, three in the morning and two in the evening. Activation was carried out until the desired clinical results were achieved.
Conclusion
In AMD precision diagnosis, careful, methodical planning and stringent observant follow up protocols are essential. An amalgam of sound basics with careful technical execution will help achieve good post-treatment outcome with no to minimal complications.
Acknowledgement
None
Conflict of Interest
None
Funding Source
None
References
- Liao Y-F, Mars M. Long-Term Effects of Clefts on Craniofacial Morphology in Patients With Unilateral Cleft Lip and Palate. Cleft Palate-Craniofacial J. 2005;42(6):601-609.
- Naqvi Z, Ravi S, Shivalinga B, Munawwar S. Effect of cleft lip palate repair on craniofacial growth. J Orthod Sci. 2015;4(3):59.
- Smahel Z. Craniofacial morphology in adults with bilateral complete cleft lip and palate. Cleft Palate J. 1984;21(3):159-169
- Hochban W, Gans C, Austermann KH. Long-term results after maxillary advancement in patients with cleft. Cleft Palate CraniofacJ 1993;30:237-243.
- Cheung LK, Sammam N, Hiu E, Tiderman H. The 3-dimensional stability of maxillary osteotomies in cleft patients with residual alveolar clefts. Br J Oral Maxillofac Surg 1994;32:6-12.
- Posnick JC, Dagys AP. Skeletal stability and relapse patterns after Lefort I maxillary osteotomy fixed with miniplates: The unilateral cleft lip and palate deformity. Plast Reconstr Surg l994;94:924-932.
- Erbe M, Stoelinga PJ, Leenen RJ. Long-term results of segmental repositioning of the maxilla in cleft palate patients without previously grafted alveolo-palatal clefts. J Craniomaxillofac Surg 1996;24:109-117.
- Figueroa AA, Polley JW, Ko EW. Maxillary distraction for the management of cleft maxillary hypoplasia with a rigid external distraction system. InSeminars in orthodontics 1999 Mar 1 (Vol. 5, No. 1, pp. 46-51).
- Ilizarov GA: The principles of the Ilizarov method. Bull Hosp Joint Dis Orthop Inst 48:1–11, 1988
- Kessler P, WiltfangJ, Schultze-Mosgau S, Hirschfelder U, Neukam W: Distraction osteogenesis of the maxilla and midface usinga subcutaneous device: report of four cases. Br J Oral Maxillofac Surg39:13–21, 2001
- Meyer U, Wiesmann HP, Kruse-Losler B, Handschel J, Stratmann U, Joos J: Strain-related bone remodelingin distraction osteogenesis of the mandible. Plast Reconstr Surg 103:800–807, 1999
- Polley JW, Figueroa AA: Management of severe maxillary deficiency in childhood and adolescence through distraction osteogenesis with an external, adjustable, rigid distraction device. J Craniofac Surg8:181–185, 1997
- Karakasis D, Hadjipetrou L. Advancement of the anterior maxilla by distraction (case report). Journal of Cranio-Maxillofacial Surgery. 2004 Jun 1;32(3):150-4.
- Baek SH, Lee JK, Lee JH, et al. Comparison of treatment outcome and stability between distraction osteogenesis and LeFort I osteotomy in cleft patients with maxillary hypoplasia. J Craniofac Surg 2007;18:1209–1215
- Wagner S, Reyneke JP. The Le Fort I downsliding osteotomy: a study of long-term hard tissue stability. Int J Adult Orthodon Orthognath Surg 2000;15:37–49 6.
- Alkan A, Bas B, Ozer M, et al. Maxillary anterior segmental advancement of hypoplastic maxilla in cleft patients by distraction osteogenesis: report of 2 cases. J Oral Maxillofac Surg 2008;66:126–132
- Guyette TW, Polley JW, Figueroa A, et al. Changes in speech following maxillary distraction osteogenesis. Cleft Palate Craniofac J 2001;38:199
- Nohara K, Tachimura T, Wada T. Prediction of deterioration of velopharyngeal function associated with maxillary advancement using electromyography of levator veli palatini muscle. Cleft Palate Craniofac J 2006;43:174–178
- Markose E, Paulose J, Paul ET. Soft tissue changes in cleft lip and palate patients: anterior maxillary distraction versus conventional Le-Fort I osteotomy. J Maxillofac Oral Surg 2013;12:429
- Lin X, Zhou N, Huang X, Song S, Li H. Anterior Maxillary Segmental Distraction Osteogenesis for Treatment of Maxillary Hypoplasia in Patients With Repaired Cleft Palate. Journal of Craniofacial Surgery. 2018 Jul 1;29(5):e480-4.
- Sunitha C, Gunaseelan R, Anusha V, et al. Maxillary movement in cleft patients treated with internal tooth borne distractor. J Maxillofac Oral Surg 2013;12:266–272
- Hanson PR, Melugin MB. Orthodontic management of the patientundergoing mandibular distraction osteogenesis. InSeminars in orthodontics 1999 Mar 1 (Vol. 5, No. 1, pp. 25-34). Elsevier.
- Liou EJW, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. Surgery first accelerated orthognathic surgery: postoperative rapid orthodontic tooth movement. J Oral Maxillofac Surg 2011;69(3): 781–785
- Verna C, DalstraM, Melsen B. The rate and the type of orthodontic tooth movement is influenced by bone turnover in a rat model. Eur J Orthod 2000;22(4):343–352
- Liou EJW, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. Surgery first accelerated orthognathic surgery: postoperative rapid orthodontic tooth movement. J Oral Maxillofac Surg 2011;69(3): 781–785
- Verna C, DalstraM, Melsen B. The rate and the type of orthodontic tooth movement is influenced by bone turnover in a rat model. Eur J Orthod 2000;22(4):343–352
- Sudhir R, Ramnathan M. Distraction osteogenesis in the maxilla for a patient with a repaired cleft lip and palate: A case report. Spec Care Dentist 2011;31:182‑7.
- Richardson S, Agni NA, Selvaraj D. Anterior maxillary distraction using a tooth-borne device for hypoplastic cleft maxillas-a pilot study. J Oral Maxillofac Surg. 2011 Dec;69(12):e542-8.







