Chandra Shekar B R1  , Ramesh Nagarajappa2, Richa Jain3, S Suma4, K Mruthunjaya5 and Rupesh Thakur6
, Ramesh Nagarajappa2, Richa Jain3, S Suma4, K Mruthunjaya5 and Rupesh Thakur6
1Department of Public Health Dentistry, JSS Dental College and Hospital, JSS Academy of Higher Education and Research, Mysore
2Department of Public Health Dentistry, Institute of Dental Sciences, Siksha “O” Anusandhan (Deemed to be University), Bhubaneshwar, Odisha, India
3Center for Scientific Research and Development, People’s University, Bhanpur, Bhopal, Madhya Pradesh
4Department of Orthodontics and Dentofacial Orthopedics, JSS Dental College and Hospital, JSS Academy of Higher Education and Research, Mysuru
5Department of Pharmacognosy, JSS College of Pharmacy, JSS Academy of Higher Education and Research, Mysuru
6Center for Scientific Research and Development, People’s University, Bhanpur, Bhopal, Madhya Pradesh
Corresponding Author E-mail: drchandrashekarbr_dch@jssuni.edu.in
DOI : https://dx.doi.org/10.13005/bpj/1794
Abstract
To develop a novel, innovative herbal formulation that can prevent both dental caries and periodontal diseases simultaneously. This clinical research involved in vitro studies to determine Minimum Inhibitory Concentration (MIC) of combinations of Acacia nilotica, Murraya koenigii Linn Sprengel, Eucalyptus hybrid, and Psidium Guajava on dental caries and plaque bacteria followed by evaluation of phytochemical constituents in these plant extracts. MIC was determined using broth dilution method. Then, an animal experimentation was carried out to determine median lethal dose and adverse drug reactions following single oral administration of polyherbal extract which was followed by human experimentation. A short term double blind randomized double blind study on 34 adult human volunteers was undertaken to assess antiplaque efficacy of a novel polyherbal mouth rinse using 0.2% chlorhexidine as positive control.MIC of the polyherbal combinations on S. mutans, S. sanguis, S. salivarius, L. acidophilus, F. nucleatum and P. gingivalis was found to be 0.25%, 0.05% , 0.05%, 0.1%, 0.25% and 0.25% respectively. Median lethal dose (LD50) for herbal formulation was found to be more than 2000mg/kg body weight. In vivo study found that the polyherbal mouth rinse group had lesser plaque buildup, S mutans and total viable count in comparison with saline group with no significant difference in plaque build-up and total viable count between polyherbal rinse group and 0.2% chlorhexidine. Polyherbal mouth rinse containing Acacia nilotica, Murraya koenigii L.sprengel, Eucalyptus hybrid and Psidium guajava was effective against dental caries and plaque induced dental diseases.
Keywords
Antiplaque Efficacy; Dental Caries; Median Lethal Dose; Minimum Inhibitory Concentration; Periodontal Diseases
Download this article as:| Copy the following to cite this article: Shekar B. R. C, Nagarajappa R, Jain R, Suma S, Mruthunjaya K, Thakur R. Evaluating the Antimicrobial Efficacy of an Innovative, Novel Herbal Formulation on Dental Caries and Plaque Microorganisms - A Clinical Research. Biomed Pharmacol J 2019;12(4) |
| Copy the following to cite this URL: Shekar B. R. C, Nagarajappa R, Jain R, Suma S, Mruthunjaya K, Thakur R. Evaluating the Antimicrobial Efficacy of an Innovative, Novel Herbal Formulation on Dental Caries and Plaque Microorganisms - A Clinical Research. Biomed Pharmacol J 2019;12(4) Available from: https://bit.ly/33SA1jJ |
Introduction
Oral health is an inseparable part of general health and a healthy mouth enables an individual to speak, eat and socialize without experiencing active disease, discomfort or embarrassment.1 Health promotion measures are deemed incomplete without promotion of oral health and prevention of many oral diseases that have a major bearing on general health1. The prevalence of dental caries is progressively increasing and periodontal diseases are one of the most common human afflictions.2 Loss of teeth attributable to periodontitis often causes discomfort, compromises esthetics and function. Moreover, recent studies suggest an association between chronic low grade infections such as periodontitis with systemic health problems3 including cardiovascular diseases4, pre-term low birth weight5, diabetes mellitus6 and chronic obstructive pulmonary disease.3 Treatment of established dental diseases is very expensive and not a realistic option for the poor. There is an immediate need for promoting preventive measures that are acceptable, cost-effective and easily available.
The conventional practices for prevention of dental caries and periodontal diseases are use of fluorides in various forms and mechanical oral hygiene combined with proper professional maintenance respectively. In reality, however, the degree of motivation and dexterity required for optimum oral hygiene is beyond the ability of a large section of the population. Antimicrobial mouth rinses have also been suggested as adjuncts for mechanical plaque control methods. Most commonly used antiplaque agent is chlorhexidine gluconate. The use of chlorhexidine has some potential drawbacks like altered taste sensation, staining of teeth and development of resistant microorganisms that incapacitate their long term use.7There exists a need to develop some innovative strategies that act against microorganisms responsible for these highly prevalent oral diseases. One such strategy would be to authenticate the enormous wealth of medicinal plants richly available in natural world.
Our in vitro studies have demonstrated antimicrobial efficacy of plant extracts of Acacia nilotica, Murraya koenigii L.Sprengel, Eucalyptus hybrid and Psidium Guajava against dental caries and plaque bacteria.8-10
In most studies, individual plant extracts have been tested against various bacteria and fungi. Some studies have tested the antimicrobial efficacy of plant extracts on microorganisms that caused either dental caries or periodontal diseases. The combination of these plant extracts that can act against both dental caries and periodontal pathogens was never investigated. A methodical and orderly evaluation of plant extracts and their combinations present an ideal approach for evolution of novel drugs from plants.11 In this background, the present clinical research was undertaken with the aim of developing a novel, innovative polyherbal formulation that can prevent both dental caries and periodontal diseases.
Objectives
To determine the MIC of the combinations of Acacia nilotica, Murraya koenigii Linn Sprengel, Eucalyptus hybrid, and Psidium Guajava on Streptococcus mutans, Lactobacillus acidophilus (dental caries bacteria), Streptococcus sanguis, Strptococcus salivarius (primary plaque colonizers), Fusobacterium nucleatum (secondary plaque colonizer) and Porphyromonas gingivalis (tertiary plaque colonizer).
To undertake a qualitative assay of phytochemical constituents present in the four plant extracts
To determine the median lethal dose and adverse drug reactions following single oral dosage of the combinations of Acacia nilotica, Murraya koenigii L.Sprengel, Eucalyptus hybrid and Psidium Guajava extracts using female Albino Wistar rats.
To assess the feasibility of using this polyherbal formulation as a mouth rinse for daily use.
To evaluate the antiplaque and antimicrobial efficacy of the polyherbal mouth rinse on a group of adults in a randomized control trial.
Materials and method
This research was carried out over a period of three and half years from March 2013 to September 2016 at the center for Scientific Research and Development, People’s University, Bhopal following approval of research protocol by the Institutional Review Board. The study involved in vitro studies to assess antimicrobial efficacy of plant extracts followed by qualitative evaluation of phytochemical constituents in these plant extracts. Then, an animal experimentation was carried out to determine the median lethal dose and adverse drug reactions following single oral administration of the polyherbal extract. This was followed by a short term randomized controlled trial on human adults.
The branches of four plants with ethno-pharmacological background which were easily available in central India were collected from surrounding areas. The plants were identified and authenticated by a taxonomist. Healthy leaves were separated from these branches, washed and shade dried over a period of three-four weeks at room temperature. The dried leaves were hand crushed and fine powder was prepared using a mixer grinder. Powders were stored in coded airtight plastic bottles in refrigerator at 40C till further use. Soxhlet apparatus using ethanol was used for plant extraction process.
Preparation of combination of extracts
Stock solutions of the individual plants were prepared by dissolving 100 mg of the extract in 1000 µl of dimethyl sulfoxide (DMSO). The quadruple combinations of plant extracts were prepared by mixing equal quantities of the stock solutions of individual extracts.
Minimum Inhibitory Concentration (MIC) of the herbal formulation
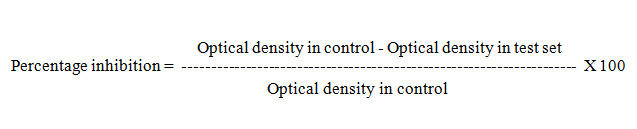
MIC of the combinations of Acacia nilotica, Murraya koenigii Linn Sprengel, Eucalyptus hybrid, and Psidium Guajava on Streptococcus mutans, Lactobacillus acidophilus (dental caries bacteria), Streptococcus sanguis, Strptococcus salivarius (primary plaque colonizers), Fusobacterium nucleatum (secondary plaque colonizer) and Porphyromonas gingivalis (tertiary plaque colonizer) was carried out using broth dilution method. MIC was defined as the minimum concentration of extract that caused 20% inhibition in growth of test microorganism.12, 13 The percentage of bacterial inhibition by each extract was computed using the following equation
Phytochemical constituent analysis
A qualitative analysis was carried out to determine the phytochemical constituents in Acacia nilotica, Murraya koenigii Linn Sprengel, Eucalyptus hybrid, and Psidium Guajava extracts. Alkaloids were determined using Mayer’s test, Wagner’s test and Hager’s test. Terpenoids were detected using Salkowski Test, saponins using foam test, flavonoids using Magnesium and hydrochloric acid reduction test, tannins using Ferric chloride test and cardiac glycosides using Legal test and Killer Kiliani test. The presence of anthraquinones was detected by adding 1ml dilute ammonia solution to 2 ml of extract dissolved in distilled water. The development of pink color in ammonia layer following vigorous shaking confirmed the presence of anthraquinones.
Animal experimentation
Median lethal dose and adverse drug reactions following single oral dosage of the combinations of Acacia nilotica, Murraya koenigii L.Sprengel, Eucalyptus hybrid and Psidium Guajava extracts was evaluated using female Albino Wistar rats. These rats weighed approximately 150-200g. Animal experiment was conducted at Center for Scientific Research and Development (CSRD), People’s University, Bhopal between 1st January 2015 and 30th March 2015 after obtaining ethical clearance from the Institutional Animal Ethics Committee (IAEC), CSRD, Bhopal. Experiment was undertaken according to the OECD (Organization for Economic Co-operation and Development) guidelines-425.14 15 healthy adult female Albino Wistar rats from Central Animal Facility (All India Institute of Medical Sciences, New Delhi), were procured and allowed to get accustomed to the experimental conditions for 5 days. All animals were fed standard dry rat pellet diet, and ad libitum of tap water. 15 rats were assigned into five groups of three rats each. The first group was kept as control while other groups of were fed different doses of the herbal formulation by single oral administration (500, 1000, 1500, 2000 mg /kg body weight). Control group of rats were fed normal saline. 18 h prior to dosing, rats were fasted. The compound was administered orally as a single dose using a 22-gauze oral feeding needle. Animals were observed continuously for first two hours and subsequently, at 4th, 6th and 24 hrs following administration of extract to identify changes in the behavioral responses such as tremors, convulsion, salivation, diarrhoea, lethargy, sleep, coma and monitored for any mortality. The numbers of deceased rats in each group was counted and percentage of mortality was calculated using graphical method of Miller and Tainter.15An approximate LD50 was determined by observing the mortality experienced by the rats in different groups at the end of 24 hours. Blood samples from the surviving rats were collected at the end of 24 hours and subjected to liver function tests. Estimation of serum total protein, albumin, total bilirubin, aspartate aminotranferases (AST), alanine aminotransferases (ALT), and alkaline phosphatase (ALP) activities were performed as various biochemical indices of liver function. Liver weight, body weight, feed intake and faecal output were also determined.
Preparation of the mouth rinse for In vivo study
The mouth rinses were prepared in the department of Pharmacology, in a Pharmacy college. 0.25 gm of each plant extract was accurately weighed into a clean sterile mortar. The required quantity of Tween -80 and menthol were added to obtain a homogenous mixture. This was triturated after adding small quantity (5-10ml) of sterile water to get a homogenous solution which was made up to 1000 ml and packed in coded plastic bottles. Since mouth rinses were prepared without any added preservatives, they were preserved for seven days following their preparation to observe any changes in colour, odour, and consistency. The mouth rinses were inoculated in nutrient agar plates after seven days of preservation to check for any bacterial contamination. Mouth rinses were simultaneously used by the investigator to test their odor, consistency and side effects by the investiator by using them for seven days.
In vivo study
A short term parallel double blind randomized controlled trial was undertaken to assess the antiplaque and antimicrobial efficacy of the herbal formulation on a group of adults selected from a hostel. Study was conducted among thirty four adult volunteers aged between 18-30 years residing in a hostel. The study was conducted over a period of two weeks in August 2016. After obtaining permission from concerned authorities to conduct the study, written informed consent was obtained from each participant. Principal investigator addressed all prospective participants in a group discussion and clarified their doubts. Ethical clearance was obtained from the Institutional Ethics Committee (IEC). The research was conducted in accordance with the guidelines of World Medical Association declaration of Helsinki. The null hypothesis for in vivo study was stated as “there is no significant difference in the antiplaque and antimicrobial efficacy of three mouth rinses”. The sample size was estimated based on hypothesis testing between two means using nMaster software. The sample size was estimated to be 11 per group at an assumed mean difference of 0.45, effect size of 1.12, at 5% alpha error and 80% power. However, the sample size was increased to 12 per group to compensate for 10% drop out.
The participants offering informed consent with eligible criteria cited beneath were recruited
Inclusion Criteria
Adult participants aged between 18-30 years
Free from systemic diseases
Free from physical and mental disabilities
Willing to offer informed consent
Minimum 20 natural permanent teeth
Exclusion Criteria
Gross oral defects that interfered with chewing
History of use of antibiotics in the last three months
Any deleterious and parafunctional habits
Presence of removable / fixed appliances
Forty eight participants residing in the hostel were considered for initial screening. However, twelve participants were excluded. Six participants were not recruited as they expressed non availability, three participants admitted that they have some deleterious habit, two participants had unilateral mastication owing to grossly decayed teeth and one participant had used amoxicillin for five days within the last 20 days for severe throat infection.
Pre-intervention prophylaxis
Scaling and polishing was offered to all eligible thirty six participants using a portable ultra sonic scaler to reduce plaque score to zero. This was confirmed by a trained and calibrated clinical evaluator using Turesky’s modification of Quigley Hein Plaque Index.16 Cronbach’s alpha value was 0.9 for intra-examiner reliability indicating good correlation between the scores during test – retest method.
Randomization and Group allocation
The eligible participants were randomly assigned to three different categories. Thirty six participants were requested to stand in a line and were asked to loudly spell out numbers 1, 2, 3 in an order. All participants calling out number 1 were assigned to group 1 while participants calling out 2 and 3 were assigned to group 2 and 3 respectively. The randomization and group allocation was done by the coordinator and information on group allocation was kept confidential till the research was over.
Intervention
Each participant was given a oral hygiene kit consisting of a medium bristled tooth brush, a 200 gram non-fluoridated tooth paste and a 150 ml coded mouth rinse bottle. The mouth rinses were coded as A, B and C.
Group 1
Saline Mouth rinse
Group 2
Mouth rinse containing Acacia nilotica, Murraya koenigii Linn Sprengel, Eucalyptus hybrid, and Psidium Guajava extracts at 1%.
Group 3
0.2% chlorhexidine diluted to 50% with distilled water.
Each participant was distributed a 150 ml mouth rinse bottle. The participants were instructed to use 10 ml of mouth rinse once in the morning before breakfast and once in the night after dinner for one minute. The participants were directed to avoid intake of any solid and liquid food items for half an hour following mouth rinsing. All participants refrained from using any other oral hygiene aids other than tooth brush and paste provided to them. A medium bristled brush and a 200 gram non-fluoridated tooth paste was given to each of these participants. Directions for the use of mouth rinse in local language were written on the bottles. Contact details of investigator were also written on the bottle and participants were informed to report any adverse events such as altered taste sensation, burning, nausea, vomiting etc. The mouth rinse bottles were collected back at the end of one week and the second set of mouth rinse bottles were distributed on day 7. This ensured that the participants were scrutinized for compliance with regard to use of mouth rinse.
Assessment criteria
On 15th day after intervention, plaque buildup in each participant was assessed by one blinded investigator using Turesky’s modification of Quigley Hein Plaque Index. Along with clinical evaluation, supragingival plaque samples were collected from the buccal surface of maxillary left first permanent molar in each participant. Salivary flow before and 90 minutes after mouth rinsing was assessed on day fifteen. The unstimulated saliva samples were collected before and 90 minutes after mouth rinsing in each participant. Microbial evaluation was undertaken using plaque samples while saliva samples were used for assessing the change in salivary pH before and after rinsing the mouth.
Microbial evaluation
S mutans and total viable count in plaque samples was evaluated using spread plate technique in a microbiology laboratory at Mysuru. The plaque samples also were coded as A, B and C to ensure blinding.
Estimation of salivary parameters
The salivary flow before and after mouth rinsing was evaluated besides saliva samples were estimated for pH. Salivary pH was determined using pH meter (Systronics, Ahmedabad, MK – 6). The CONSORT (Consolidated Standards of Reporting Trials) flow diagram for the randomized trial is presented as figure 1.
 |
Figure 1: Diagrammatic representation of clinical research |
Statistical methods
The statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 20 (IBM, Chicago USA). One way Analysis of Variance (ANOVA) and Tukey’s post hoc test, independent sample t-test and Pearson’s chi square test were used. The statistical significance was fixed at 0.05.
Results
In vitro study
MIC of the combinations of Acacia nilotica, Murraya koenigii L.Sprengel, Eucalyptus hybrid and Psidium Guajava on S. mutans, S. sanguis, S. salivarius, L. acidophilus, F. nucleatum and P. gingivalis was found to be 0.25%, 0.05% , 0.05%, 0.1%, 0.25% and 0.25% respectively (table 1 A and B). The summary of qualitative assay of phytochemical constituents in four plant extracts derived using hot and cold extraction methods is presented in table 2.
Table 1 A: Minimum Inhibitory Concentration of combinations of Acacia nilotica, Murraya koenigii L.Sprengel, Eucalyptus hybrid and Psidium Guajava on S. mutans, S. sanguis and S. salivarius.
| Concentrations | S. mutans
(Mean optical density ± SD ) |
% inhibition | S. sanguis
(Mean optical density ± SD ) |
% inhibition | S. salivarius
(Mean optical density ± SD ) |
% inhibition |
| 0.05% | 0.4±0.01 | 11.9 | 0.4±0.02 | 20.5 | 0.4±0.02 | 24.6 |
| 0.1% | 0.4±0.02 | 19.4 | 0.4±0.02 | 26.6 | 0.4±0.03 | 30.3 |
| 0.25% | 0.4±0.02 | 30.7 | 0.4±0.02 | 33.5 | 0.4±0.03 | 34.1 |
| 0.5% | 0.3±0.01 | 41.3 | 0.3±0.01 | 36.2 | 0.3±0.01 | 41.9 |
| 0.75% | 0.3±0.02 | 45.6 | 0.3±0.01 | 44.4 | 0.3±0.02 | 49.2 |
| 1.0% | 0.3±0.03 | 50.9 | 0.3±0.02 | 53.2 | 0.2±0.01 | 57.4 |
| 1.25% | 0.2±0.02 | 70.0 | 0.1±0.02 | 75.8 | 0.2±0.01 | 67.7 |
| 1.5% | 0.1±0.02 | 75.5 | 0.1±0.02 | 83.6 | 0.1±0.01 | 73.4 |
| Chlorhexidine | 0.2±0.02 | 69.3 | 0.2±0.01 | 66.5 | 0.2±0.01 | 73.1 |
| Control (without extract) | 0.5±0.03 | 0.5±0.03 | 0.6±0.03 | |||
| Percentage inhibition is computed using equation OD control / OD control – OD test X 100 | ||||||
| Concentration inhibiting at least 20% of bacterial growth is considered MIC | ||||||
Table 1 B: Minimum Inhibitory Concentration of combinations of Acacia nilotica, Murraya koenigii L.Sprengel, Eucalyptus hybrid and Psidium Guajava on L. acidophilus, F. nucleatum and P. gingivalis.
| Concentrations | L. acidophilus
(Mean optical density ± SD ) |
% inhibition | F. nucleatum
(Mean optical density ± SD ) |
% inhibition | P. gingivalis
(Mean optical density ± SD ) |
% inhibition |
| 0.05% | 0.5±0.01 | 16.0 | 0.6±0.02 | 4.0 | 0.5±0.01 | 13.8 |
| 0.1% | 0.5±0.02 | 22.1 | 0.5±0.03 | 17.2 | 0.5±0.02 | 17.5 |
| 0.25% | 0.4±0.02 | 33.5 | 0.5±0.02 | 222.0 | 0.4±0.01 | 31.2 |
| 0.5% | 0.4±0.02 | 37.4 | 0.4±0.01 | 29.9 | 0.4±0.02 | 37.6 |
| 0.75% | 0.3±0.02 | 45.0 | 0.4±0.01 | 38.0 | 0.3±0.02 | 43.1 |
| 1.0% | 0.3±0.02 | 56.6 | 0.3±0.01 | 48.5 | 0.3±0.02 | 54.9 |
| 1.25% | 0.2±0.02 | 63.4 | 0.3±0.02 | 55.2 | 0.2±0.01 | 65.1 |
| 1.5% | 0.2±0.02 | 70.1 | 0.2±0.02 | 61.3 | 0.2±0.02 | 66.8 |
| Chlorhexidine | 0.2±0.02 | 63.5 | 0.2±0.02 | 65.3 | 0.2±0.01 | 71.3 |
| Control (without extract) | 0.6±0.02 | 0.6±0.02 | 0.6±0.01 | |||
| Percentage inhibition is computed using equation OD control / OD control – OD test X 100 | ||||||
| Concentration inhibiting at least 20% of bacterial growth is considered MIC | ||||||
Table 2: Summary of qualitative assay of phytochemical constituents in plant extracts derived using hot and cold extraction methods
| Phytochemical constituents and test used | Extraction method | Acacia Arabica | Murraya koenigii L.Sprengel | Eucalyptus hybrid
|
Psidium Guajava |
| Alkaloids (using Mayer’s reagent) | Cold | – | + | – | + |
| Hot | – | – | – | – | |
| Alkaloids (using Dragendorff’s reagent) | Cold | – | + | – | + |
| Hot | – | – | – | – | |
| Anthraquinones (Borntrager’s test) | Cold | + | – | – | + |
| Hot | + | – | – | + | |
| Terpenoids (Salkowski’s test) | Cold | – | + | + | + |
| Hot | – | – | + | + | |
| Saponins (Froth and emulsion test) | Cold | + | – | + | + |
| Hot | – | – | + | – | |
| Flavanoids (Shinoda test) | Cold | + | – | + | + |
| Hot | + | – | + | + | |
| Flavanoids (alkaline reagent test) | Cold | + | – | + | + |
| Hot | + | – | + | + | |
| Tannins (Ferric chloride test) | Cold | + | + | + | + |
| Hot | + | + | + | + | |
| Tannins (lead acetate test) | Cold | + | + | + | + |
| Hot | + | – | + | + | |
| Cardiac glycosides (Legal test) | Cold | + | + | + | + |
| Hot | + | + | + | + | |
| Cardiac glycosoids (Killer – kiliani test) | Cold | + | + | + | + |
| Hot | + | + | + | + |
Median lethal dose (LD50) for the combinations of A.nilotica, Murraya koenigii L.Sprengel, Eucalyptus hybrid and Psidium Guajava extracts was found to be more than 2000mg/kg body weight as there was no mortality in any groups. There was no statistically significant difference in the body weight, liver weight, and various parameters of liver function between rats that received different doses of herbal formulation in comparison with control group (table 3).
Table 3: Summary of acute toxicity results on experimental rats
| Parameter | Control
|
500 mg/kg B.W | 1000 mg/kg B.W | 1500mg/kg
|
2000mg/kg
|
Statistics |
| Number | (n=3) | (n=3) | (n=3) | (n=3) | (n=3) | Total (n=15) |
| Body weight (gms) | 276.9±11.0 | 289±16.6 | 292.1±3.8 | 291.5±10.6 | 288.5±1.0 | F value: 1.091
p: 0.41 |
| Total Proteins (g%) | 7.6±0.0 | 7.5±0.2 | 7.5±0.1 | 7.6±0.1 | 7.6±0.1 | F value: 0.665
p: 0.63 |
| Albumin (g%) | 3.4±0.0 | 3.4±0.2 | 3.5±0.1 | 3.5±0.2 | 3.6±0.0 | F value: 1.279
p: 0.34 |
| Bilirubin (mg%) | 0.6±0.1 | 0.7±0.0 | 0.7±0.1 | 0.7±0.0 | 0.7±0.0 | F value: 2.203
p: 0.14 |
| AST (IU/L) | 61.2±1.4 | 64.3±2.1 | 60.0±1.3 | 60.2±1.8 | 61.7±2.6 | F value: 2.375
p: 0.12 |
| ALT (IU/L) | 40.3±1.0 | 41.6±0.5 | 40.9±0.9 | 40.6±0.7 | 40.4±1.5 | F value: 0.860
p: 0.52 |
| ALP (IU/L) | 65.4±1.1 | 65.1±0.5 | 64.7±0.3 | 64.2±0.5 | 66.4±2.1 | F value: 1.681
p: 0.23 |
| Liver weight (gms) | 6.2±0.2 | 6.1±0.1 | 6.8±0.4 | 6.7±0.1 | 6.3±0.6 | F value: 2.89
p: 0.08 |
| No mortality was observed in any of these groups | ||||||
Acute toxicity
In vivo study
Thirty four participants were available for follow up examination on day 15 and one participant each from group 2 and 3 were dropped out. The dropped out participant in group 2 used an antimicrobial drug that was prescribed for fever during the intervention period while participant in group 3 stopped using the assigned mouth rinse due to unpleasant taste. Mean age of study participants was 19.7 ± 1.9 years. There was no significant difference in the mean age of study participants between different intervention groups (p = 0.06, table 4). The mean plaque build-up was highest in group 1 that used placebo (1.82 ± 0.12) compared to other groups. The difference in mean plaque score between different categories was statistically significant (p < 0.001, table 5). The post hoc test found a significant difference between group 1 against groups 2 and 3. However, the difference in the mean plaque scores between group 2 (0.36 ± 0.02) that used 1% polyherbal mouth rinse and group 3 (0.28 ± 0.01) that used 0.2% chlorhexidine with 50% dilution was not statistically significant (p = 0.93, table 5). Mean S. mutans colony count (CFU/ml) was highest in group 1 (282.4 ± 22.2) followed by group 2 (195.3 ± 9.7). The least count was found in group 3 (158.3 ± 12.2). The difference in the mean S. mutans count between different categories was statistically significant (p < 0.001, table 6). The post hoc revealed a significant difference between group 1 with other groups as well as between group 2 and 3. The mean total viable count (CFU/ml) was highest in group 1 (328.4 ± 28.6) followed by group 2 (232.5 ± 18.6). The least count was found in group 3 (212.5 ± 14.3). The difference in mean total viable count between different categories was statistically significant (p < 0.001, table 6). The post hoc test revealed a significant difference between group 1 with others. However, the difference between group 2 and 3 was not statistically significant (p =0.91, table 6). There was no significant difference in the mean salivary flow rate and pH between different groups at baseline and post-intervention as well as between baseline and 90 minutes after mouth rinsing in each group (Table 7). No significant differences were observed in compliance and reported adverse effects between three groups.
Table 4: Distribution of study participants in different intervention groups
| Group | Number of participants
N (%) |
Mean age ± Standard deviation (years) |
| Group 1 (Placebo) | 12 (35.2) | 19.4 ± 1.4 |
| Group 2 (polyherbal mouth rinse) | 11 (32.4) | 20.3 ± 2.3 |
| Group 3 (0.2% chlorhexidine) | 11 (32.4) | 19.3 ± 2.0 |
| Total | 34 (100) | 19.7 ± 1.9 |
| Statistical inference | F value: 0.72, p value: 0.06 | |
Table 5: Comparison of mean plaque build up between different intervention groups on day 15 following intervention
| Group | Number of participants
N (%) |
Mean plaque score ± Standard deviation | |
| Group 1 (Placebo) | 12 (35.2) | 1.82 ± 0.12 | |
| Group 2 (polyherbal mouth rinse) | 11 (32.4) | 0.36 ± 0.02 | |
| Group 3 (0.2% chlorhexidine) | 11 (32.4) | 0.28 ± 0.01 | |
| Total | 34 (100) | 0.76 ± 0.7 | |
| Statistical inference | F value: 1721.41, p value < 0.001 | ||
| Post hoc comparison | Effect size (r) | p value | |
| Group 1 Vs Group 2
Group 1 Vs Group 3 Group 2 Vs Group 3 |
0.92
0.93 0.22 |
< 0.001
< 0.001 0.93 |
|
Table 6: Comparison of mean S. mutans and total viable count between different intervention groups on day 15 following intervention.
| Group | Number of participants
N (%) |
Mean S. mutans CFU (10-2) ± Standard deviation | Mean total viable count CFU (10-2) ± Standard deviation | ||
| Group 1 (Placebo) | 12 (35.2) | 282.4 ± 22.2 | 328.4 ± 28.6 | ||
| Group 2 (polyherbal mouth rinse) | 11 (32.4) | 195.3 ± 9.7 | 232.5 ± 18.6 | ||
| Group 3 (0.2% chlorhexidine) | 11 (32.4) | 158.3 ± 12.2 | 212.5 ± 14.3 | ||
| Total | 34 (100) | 208.4 ± 48.2 | 251.4.3 ± 56.261.5 | ||
| Statistical inference | F value: 123.2
p value < 0.001 |
F value: 175.3,
p value < 0.001 |
|||
| Post hoc comparison | Effect size (r) | p value | Effect size (r) | p value | |
| Group 1 Vs Group 2
Group 1 Vs Group 3 Group 2 Vs Group 3 |
0.9
0.9 0.8 |
< 0.001
<0.001 <0.001 |
0.9
0.9 0.1 |
< 0.001
<0.001 0.91 |
|
Table 7: Comparison of salivary parameters before and 90 minutes after mouth rinsing in different intervention groups
| Group
|
Salivary flow rate before mouth rinsing in
ml/minute (Mean ± SD) |
Salivary flow rate after mouth rinsing in
ml/minute (Mean ± SD) |
Statistical inference | Salivary pH before mouth rinsing | Salivary pH after mouth rinsing
|
Statistical inference
|
| Group 1 (Placebo) | 0.36 ± 0.1 | 0.36 ± 0.03 | t value: 0.40
p = 0.70 |
6.8 ± 0.13 | 6.8 ± 0.2 | t value: -0.23
p = 0.82 |
| Group 2 (polyherbal mouth rinse) | 0.4 ± 0.03 | 0.4 ± 0.04 | t value: – 1.09
p = 0.30 |
6.9 ± 0.13 | 6.9 ± 0.2 | t value: -1.13
p = 0.52 |
| Group 3 (0.2% chlorhexidine) | 0.4 ± 0.04 | 0.4 ± 0.05 | t value: – 1.19
p = 0.30 |
6.8 ± 0.11 | 6.9 ± 0.12 | t value: – 1.39
p = 0.25 |
| Statistical inference
|
F value: 1.23
p value: 0.31 |
F value: 2.01
p value: 0.15 |
F value: 2.4
p value: 0.11 |
F value: 3.3
p value: 0.06
|
CFU = Colony Forming Units
Discussion
The increasing trends in dental caries and gingival periodontal diseases amongst the populations in developing countries, the increasing costs of treating these diseases, and the potential side effects associated with conventional antiplaque agents call for alternate strategies. Herbs are one of remedial agents that have been used in traditional medicine for several thousand years.
The combinations of Acacia nilotica, Murraya koenigii L.Sprengel, Eucalyptus hybrid and Psidium Guajava inhibited the growth of S. mutans, S. sanguis, S. salivarius, L. acidophilus, F. nucleatum and P. gingivalis with MIC of 0.25%, 0.05%, 0.05%, 0.1%, 0.25% and 0.25% respectively. MIC of the combinations of plant extracts against these bacteria was varying from 0.05% to 0.25% and its antimicrobial efficacy was found to be good.17 This was the first of its kind where MIC of combinations of Acacia nilotica, Murraya koenigii L.Sprengel, Eucalyptus hybrid and Psidium Guajava was assessed on oral bacteria. Hence, our results could not be compared with previous published literature. The study found no significant differences in the behaviors as well as hepatic function of rats at different doses in comparison with control group of rats. None of the rats experienced mortality confirming that a dose of 2000 mg / kg body weight of this herbal formulation is safe and did not produce any symptoms of acute toxicity. These results were consistent with the findings of a study by Guta et al (2007)18 who while evaluating oral acute toxicity of ethyl acetate fruit fraction of A. nilotica found the LD50 value to be 7393.4 mg/kg (95% CI, 6019.5-9207.9 mg/kg). Tanko et al (2014)19 while assessing the methanol crude leaves extract and aqueous fraction of Acacia nilotica found the median lethal dose (LD50) in rats to be 2,154 mg/kg body weight for both crude and aqueous fractions similar to the results of the present study. The in vivo study found the polyherbal mouth rinse group to have lesser plaque build up, S mutans and total viable count compared to saline group. The lack of significant difference in plaque build-up and total viable count between polyherbal rinse group and 0.2% chlorhexidine suggest that this herbal formulation could be evaluated further as an effective herbal alternate to chlorhexidine. The antiplaque and antimicrobial efficacy of herbal mouth rinse was attributed to various phytochemical constituents present in A.nilotica, Murraya koenigii L.sprengel, Eucalyptus hybrid and Psidium guajava leaf extracts. Bhadbhade et al (2011)20, Parwani et al (2013)21, Biswas et al (2014)22, have all found different herbal mouth rinses to be effective as antiplaque agents. Phatak et al (2011)23 while assessing the efficacy of a polyherbal mouth rinse found the total viable count in the plaque samples to reduce in 85% of the participants using the polyherbal mouth rinse similar to our findings. The study found no significant differences in the reported side effects, and willingness to use these mouth rinses on a regular basis if given along with tooth brushing while some studies22, 24, 25 reported minimal side effects with polyherbal mouth rinse compared to chlorhexidine.
Strengths and limitations
This was the first of its kind where plant extract combinations have been assessed on microorganisms involved in two most prevalent dental diseases. The use of plant extracts in combinations offer increased potency due to synergistic action of phytochemicals, slower rate of development of resistance as they are complex mixtures which can make microbial adaptability difficult.26
The in vitro antimicrobial efficacy testing was assessed on important dental caries and plaque microorganisms while assessment on other secondary and tertiary plaque colonizers could offer a more comprehensive assessment. The quantitative evaluation using high pressure liquid chromatography rather than qualitative assay could highlight the concentration of active ingredients in these plant extracts. The polyherbal mouth rinse in the present study was free from any preservatives. The concerns related to shelf life, compelled us to undertake short term study using freshly prepared mouth rinses on healthy adult human volunteers. The long term studies using mouth rinses containing preservatives having a longer shelf life on participants preferably with high risk for dental caries and periodontal diseases such as differently abled participants are essential to provide external validity to the study.
Conclusion
The polyherbal mouth rinse containing Acacia nilotica, Murraya koenigii L.sprengel, Eucalyptus hybrid and Psidium guajava is feasible to be used as a mouth rinse. It was effective against most common microorganisms involved in dental caries and periodontal diseases. Hence, this polyherbal mouth rinse may be considered as a simple and effective alternate to chlorhexidine for preventing and controlling dental caries and plaque induced dental diseases. However, future research using purified extracts of these plants and their combinations are recommended to validate our results.
References
- Kwan SYL, Petersen PE, Pine CM, Borutta A. Health promoting schools: an opportunity for oral health promotion. Bull World Health Organ 2005; 83: 677- 85.
- Botelho MA, Santos RAD, Martins JG, Carvalho CO, Paz MC, Azenha C et al. Efficacy of a mouth rinse based on leaves of the neem tree (Azadirachta Indica) in the treatment of patients with chronic gingivitis: A double-blind, randomized, controlled trial. J Med Plants Res 2008; 2(11): 341- 6.
- Weidlich P, Cimoes R, Pannuti CM, Oppermann RV. Association between periodontal diseases and systemic diseases. Braz Oral Res 2008; 22(Spec Iss 1): 32-43.
CrossRef - Fentoglu O, Bozkurt The Bi-Directional Relationship between Periodontal Disease and Hyperlipidemia. Eur J Dent 2008; 2:142- 9.
CrossRef - Agueda A, Echeverria A, Manau C. Association between periodontitis in pregnancy and preterm or low birth weight: Review of the literature. Med Oral Patol Oral Cir Bucal. 2008 Sep1; 13(9): E609-15.
- Mealey BL, Oates TW. AAP-Commissioned Review: Diabetes Mellitus and Periodontal Diseases. J Periodontol 2006; 77:1289- 303.
CrossRef - Eley BM. Antibacterial agents in the control of supragingival plaque – A review. Br Dent J 1999; 186: 286-96.
CrossRef - Chandrashekar BR, Nagarajappa R, Singh R, Thakur R. An in vitro study on the anti-microbial efficacy of ten herbal extracts on primary plaque colonizers. J Young Pharm 2014; 6 (4): 33 – 39.
CrossRef - Chandrashekar BR, Nagarajappa R, Singh R, Thakur R. Antimicrobial efficacy of the combinations of Acacia nilotica, Murraya Kinigii L sprengel, Eucalyptus hybrid and psidium guajava on primary plaque colonizers. J Basic Clin pharm 2014; 5 (4): 115 -119.
CrossRef - Chandrashekar BR, Nagarajappa R, Singh R, Thakur R. Antimicrobial efficacy of Acacia nilotica, Murraya koenigii L.Sprengel, Eucalyptus hybrid and Psidium Guajava on primary plaque colonizers – An in vitro comparison between hot and cold extraction process. J Indian Soc Periodontol 2015; 9 (2): 174 – 9.
CrossRef - Gupta P, Nahata A, Dixit VK. An update on Murraya koenigii Spreng: A multifunctional Ayurvedic herb. J Chin Integr Med 2011; 9 (8): 824-33.
CrossRef - Wiegand I, Hilpert K, Hancock RE. Agar and broth dilution methods to determine the minimum inhibitory concentration (MIC) of antibacterial substances. Nat Protoc 2008; 3 (2): 163 – 75.
CrossRef - Bussmann RW, Malca – Garcia G, Sharon GD, Chati G, Diaz D, Pourmand K. Minimum inhibitory concentrations of medicinal plants used in Northern Peru as antibacterial remedies. J Ethnopharmacol 2010; 132 (1): 101 – 8.
CrossRef - Organization for Economic Co-operation and Development]. 2001a. OECD Guidelines for the Testing of Chemicals. Guideline 425 Acute Oral Toxicity—Up-and-Down Procedure. Paris:
- Randhawa MA. Calculation of LD50 values from the method of Miller and Tainter, 1994. J Ayub Med Coll Abbotabad 2009; 21 (3): 184 – 5.
- Cugini M, Thompson M, Warren PR. Correlations between two plaque indices in assessment of toothbrush effectiveness. J Contemp Dent Pract 2006; 7: 1‑
CrossRef - Dabur R, Gupta A, Mandal TK, Singh DD, Bajpai V, Gurav A M et al. Antimicrobial activity of some Indian medicinal plants. J. Trad. CAM 2007; 4 (3): 313 – 8.
CrossRef - Guta M, Ugra K, Assefa A, Lemma H, Addis G, Gemeda N et. al. Antibacterial activity and acute toxicity study of Acacia nilotica. Ethiop J Bio Sci 2007; 6 (1): 43 – 9.
CrossRef - Tanko Y, Abdulazeez A, Muhammad AJA, Mohammed KA, Mohammed A. Effect of methanol crude leaves extract and aqueous fraction of Acacia Nilotica on lipid profile and liver enzymes on alloxan -induced diabetic wistar rats. Ann Exp Bio 2014; 2 (3): 36 – 40.
CrossRef - Bhadbhade SJ, Acharya AB, Rodrigues SV, Thakur SL. The antiplaque efficacy of pomegranate mouth rinse. Quintessence Int 2011; 42 (1): 29 – 36.
CrossRef - Parwani SR, Parwani RN, Chitnis PJ, Dadlani HP, Saiprasad SV. Comparitive evaluation of anti-plaque efficacy of herbal and 0.2% chlorhexidine gluconate mouthwash in a 4-day plaque re-growth study. J Indian Soc Periodontol 2013; 17 (1): 72 – 7.
CrossRef - Biswas G, Anup N, Acharya S, Kumawat H, Vishnani P, Tambi S. Evaluation of the Efficacy Of 0.2% Chlorhexidine versus Herbal Oral Rinse on Plaque Induced Gingivitis- A Randomized Clinical Trial. IOSR Journal of Nursing and Health Science 2014; 3 (2): 58 – 63.
CrossRef - Phatak AA, Patankar RD, Galgatte UC, Paranjape SY, Deshpande AS, Pande AK et.al. Antimicrobial activity of a poly-herbal extract against dental microflora. Res J Pharm Biol Chem Sci 2011; 2(2): 533- 9.
- Ravivarma Prasad KA, John S, Deepika V, Dwijendra KS, Reddy BR, Chicholi S. Anti-Plaque Efficacy of Herbal and 0.2% Chlorhexidine Gluconate Mouthwash: A Comparative Study. J Int Oral Health 2015; 7 (8): 98 – 102.
- Aspalli S, Shetty VS, Devarathnamma MV, Nagappa G, Archana D, Parab P. Evaluation of antiplaque and antigingivitis effect of herbal mouthwash in treatment of plaque induced gingivitis: A randomized, clinical trial. J Indian Soc Periodontol 2014; 18 (1): 48 – 52.
CrossRef - Abd El – Kalek HH, Mohamed EA. Synergistic effect of certain medicinal plants and amoxicillin against some clinical isolates of methecillin – resistant Staphylococcus aureus (MRSA). International Journal of Pharmaceutical applications 2012; 3 (3): 387 – 98.








