Vikram Singh1* , Girija Kumari2
, Girija Kumari2 , Bimal Chhajer3
, Bimal Chhajer3 and Mulavagili Vijayasimha1
and Mulavagili Vijayasimha1
1Department of Medical Laboratory Technology, Amity Medical School, Amity University Haryana, Gurgaon, India
2Department of Clinical Research, Amity Medical School, Amity University Haryana, Gurgaon, India
3Department of Preventive Cardiology, SAAOL Heart Center, New Delhi, India
Corresponding Author E-mail: vsmicroaiims@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1825
Abstract
To assess the effect of Enhanced External Counter Pulsation (EECP) treatment on clinical parameters and health related quality of life (HRQoL) in Coronary Heart Disease (CHD) patients with Diabetes Mellitus. This was a pretest-posttest designed prospective study among 163 diabetic and non-diabetic coronary heart disease patients enrolled from SAAOL Heart Center, New Delhi, India. Patients were divided into two groups- diabetic CHD group and non-diabetic CHD group. EECP treatment was given to both the groups for 35 day. After EECP treatment physical and clinical profile along with HRQoL of study participants was assessed. The physical profile of study participants was assessed using Cooper’s 12 minutes’ walk test, Canadian Cardiovascular Society (CCS) angina scale and Medical Research Council (MRC) dyspnea scale and HRQoL was assessed through SF-36 (short form) and Seattle Angina Questionnaire (SAQ) scale. The follow-up of both groups was done at 6th and 12th months. Collected data were assessed through IBM, SPSS software v 21. Descriptive analysis with sample t-test for two independent groups and paired sample t-test for EECP effectiveness within the group was done. A significant improvement was observed in blood pressure; heart rate, lipid profile angina and MRC score in both the groups at 6th and 12 month follow-up. A significant reduction was observed in blood sugar fasting, blood sugar postprandial (PP) and glycosylated hemoglobin (HbA1c) in diabetic CHD patients. A significant improvement was also observed in all health domains of SF-36 & SAQ scale HRQoL after EECP treatment. EECP therapy is an effective non-invasive method to treat diabetic and non–diabetic CHD patients. This therapy may improve both physical (physical functional capacity, angina, dyspnea) and clinical profile (lipid profile, lower the blood glucose level) in diabetic CHD patients. EECP may also improve clinical symptoms of CHD patients and lower the blood glucose level in diabetic CHD patients this may directly improve overall HRQoL of CHD patients with DM.
Keywords
Enhanced External Counter Pulsation (EECP); Coronary Heart Disease (CHD); Angina; Dyspnea; Diabetes Mellitus; Health-related Quality of life (HRQoL)
Download this article as:| Copy the following to cite this article: Singh V, Kumari G, Chhajer B, Vijayasimha M. Efficacy of Enhanced External Counter Pulsation on Clinical Parameters and Health-related Quality of Life in Coronary Heart Disease patients with Diabetes Mellitus. Biomed Pharmacol J 2019;12(4). |
| Copy the following to cite this URL: Singh V, Kumari G, Chhajer B, Vijayasimha M. Efficacy of Enhanced External Counter Pulsation on Clinical Parameters and Health-related Quality of Life in Coronary Heart Disease patients with Diabetes Mellitus. Biomed Pharmacol J 2019;12(4). Available from: https://bit.ly/2Xlyssf |
Introduction
Diabetes mellitus (DM) and coronary heart disease (CHD) are life style related diseases, epidemic in India and a leading cause of morbidity and mortality around the world 1-3. Currently, it is accounting for 21.9 percent of total deaths and projected to increase to 26.3 percent by 20304. The current prevalence of diabetes mellitus with coronary heart disease is 7.8 % in India. The mortality rate of diabetic CHD patients is two to four folds higher as compared to coronary heart disease patients without diabetes mellitus in India 5-6. Diabetic patients and coronary heart disease have the highest risk (20.2%) of myocardial infarction 7. Age, family history, obesity, hypertension, unhealthy eating habits, Physical inactivity, smoking, excess alcohol, and stress are the common risk factors for developing CHD and type 2 diabetes mellitus 8-10. In diabetes patients, the glucose unable to enter the cells and similarly the amount of glucose increase in the blood and on the other side cells deprived of fuel. Hyperglycemia or high level of blood glucose leads to the deposit of fatty acids and induce platelet activation and development of atherosclerosis very fast as compared to non-diabetic coronary heart disease patients 11. Coronary artery of the diabetic patient exhibit a large content of lipid, atheroma, macrophage infiltration and have the greater chance of atherosclerosis plaque that is more vulnerable to rupture in diabetes as compared to non-diabetic coronary heart disease patients 12.
Coronary heart disease patients can be treated with pharmacotherapy, percutaneous transluminal coronary angioplasty (PTCA), coronary artery bypass grafting (CABG), laser revascularization, gene therapy and EECP. Of these modalities, only EECP therapy is truly non-invasive and represents the effective clinical benefits in the profile of CHD patients 13, 14. After PTCA patiently becomes more susceptible to re-blockage, it is because of the stent that aside, is a foreign subject for patient body and his/her immune system act accordingly. This procedure is widely used but re-blockage occurs most frequently in PTCA treated patients as compared to naive 15. After CABG symptoms of angina, dyspnea generally improves but some patients get very serious complications. The most important complication of CABG is operative death. Operative death is more common if patients have low pumping power, recent heart attack history, valve problems, and co-morbidity with diabetes and hypertension. So there is great need to pay special attention to treat these life-threatening major complications 16. Enhanced external counter pulsations US-FDA approved non-invasive therapy for treatment of CHD patients, which are not suitable, unresponsive, and unwilling for PTCA and CABG procedures. Enhanced external counter pulsation therapy increases retrograde aortic blood flow during the diastolic phase of heart pumping and provide long term improvement in clinical symptoms of coronary heart disease patients. The mechanical device called EECP comprises sequential compression over legs, thighs, and buttocks to direct blood flow towards the heart when it is in the resting position. This treatment is recommended for 35 hours, one hour per day for 7 weeks (5 days in a week) 17, 18.
Several studies demonstrated the clinical effectiveness of EECP and prove the treatment as an adjuvant therapy for CHD patients 19-21. International EECP Patient Registry (IEPR) showed significant improvements in angina and health-related quality of life in coronary heart disease patients. It also observed that EECP may also improve glycemic control in diabetes patients 22, 23. Several studies showed significant improvement in CCS classification, breathlessness, blood pressure, and lipid profile in CHD patients. But none of the study has compiled all clinical parameter in one study and not compared diabetic and non-diabetic CHD groups in the larger amount of sample. Hence, this study was designed to evaluate the effect of EECP on clinical profile and quality of life in CHD patients with DM.
Research Methodology
Study Design
This was a pretest-posttest designed prospective study, conducted among diabetic and non-diabetic coronary heart disease patients in Science and art of living (SAAOL) Heart Center, New Delhi.
Sample Size
A total of 212 subjects were recruited based on consecutive sampling technique from SAAOL Heart Centre, Delhi. The sample size for this study was calculated with the assumption of 18% risk of CHD in the control group and 45% risk of CHD in diabetic patients with an allowable error of 5% (95% power) and 5% level of significance using the nMaster v2.0 software. Calculated sample size formula is given below:
Where ps was the proportion in the treatment group and pt was the proportion in control group. d is the superiority margin.
The minimum sample size was 85 for each study group with 20% loss to follow up from the total study sample 106 in each group.
Ethical Approval and Patient Consent
Prior initiation of study ethical approval for this study was obtained from the concerned authorities of study site (Ref.No.IEC/SHRF/Ph.D/P-02/01.05.2016) and the written informed consent was obtained from all study participants before initiation of the study.
Study Eligibility Criteria
Inclusion Criteria
Diabetic and non-diabetic CHD patients either sex, aged 30 years to 75 years, having Blood Sugar Fasting above 130mg/dl, PP above 180mg/dl, and HbA1c above 6.5%. CHD patients who were not responded to current allopathic treatment and not willing for CABG & PTCA and Patients having cardiac clinical symptoms of angina and dyspnea. CHD patients coronary angiographic test diagnosed at least one vessels coronary artery disease (blockage in any 3 main coronary arteries RCA, LAD, LCX more than 60%) and CHD patients willing to participate and able to give valid written informed consent.
Exclusion Criteria
CHD patients having following clinical history such as Blood Pressure greater than 180/110 mmHg, LVEF level more than 60%, Diabetic patient having foot wounds, patients on dialysis and Pregnant women and CHD patients were not suitable or contradict to EECP treatment like as Patients having cardiac Arrhythmia, Coagulation disorder, Deep vein thrombosis, Vaso occlusive disease, Abnormal Aortic aneurysm, Cardiac valvular disorder and Patients were unwilling or unable to give valid written consent.
 |
Table 1 |
Discussion
Study procedure
Initiation of the study was done through screening of diabetic and non-diabetic coronary heart disease patients and enrolled as per eligibility criteria. Total 301 participants were screened from SAAOL Heart Center, New Delhi for this study between November 2015 and May 2016. Out of 301 patients, 89 patients were excluded from this study, in which 51 subjects did not match the inclusion criteria completely and 38 subjects refused to give consent and 12 month follow-up. Finally, 212 patients were recruited as they fulfill all study eligibility criteria and agree to participate and 12-months follow-up. The patients were allocated into two groups (DM+ CHD group and CHD group), each group had 106 patients.
After allocation, the demographic profile (age, gender, locality etc.), risk factors, clinical symptoms (CCS angina class severity and MRC dyspnea score), Physical functioning capacity, physiological and biochemical profile (systolic and diastolic blood pressure, heart rate, blood sugar levels and lipid profile), and health-related quality of life of the all study subjects were assessed at baseline and followed at 6 and 12 months.
Measurements
Physiological Measurements
Height and Weight of the participants was measured in centimeters and kilograms by using a Stature meter height tape of Bio-plus Company and Salter goal tracker weighing scale model 9063. Body mass index (BMI) was calculated using Quetelet’s formula and weight in kilograms divided by the square of the height in meters (BMI= kg/m2). Systolic and Diastolic Blood pressure of the study participant was measured by a trained personnel, using an automatic digital blood pressure monitor of Diamond Company (Diamond clock model B.P monitor). Pulse was measured using Choice MMed MD300C2D pulse oximeter and crosschecked by the manual method by an experienced doctor.
Biochemical Assessment
Blood sugar fasting was analyzed using GOD-POD method and blood sugar PP was analyzed after 2 hours of the meal by the same procedure used for blood sugar fasting and HbA1c was assessed using an immune-turbidimetry method. Total cholesterol of the participants was estimated by the CHOD-PAP method, triglyceride by GPO method, High-Density Lipoprotein (HDL) by immune inhibition method, Low-Density Lipoprotein (LDL) was calculated using standard formula; LDL-cholesterol = Total cholesterol – HDL cholesterol – VLDL, Very Low-Density Lipoprotein (VLDL) was calculated using standard formula; VLDL= Triglyceride /5, and the Non -HDL (High-Density Lipoprotein) was calculating using the standard formula; Non -HDL =Total Cholesterol- LDL = Non HDL.
Clinical Assessment
Angina and dysapnea (Breathlessness) status of all study subjects was assessed through Canadian Cardiovascular Society (CCS) grading scale and Medical Research Council (MRC) scale by an experienced doctor.
Physical Functional Capacity
Physical functional capacity was assessed through Cooper 12-minute walk test, VO2max and SpO2. In Cooper 12-minute walk test, patients advised to walk for 12 minutes on a flat track and covered distance was recorded with the physical status of the subject. VO2max is the measurement of utilization of the maximum amount of the oxygen by a study subject during 12-minute walking. VO2max (in ml/kg/min) was estimated using a standard formula from the distance score: VO2max = (22.35 x kilometers) x 11.29. SpO2 that stands – peripheral capillary oxygen saturation, is the estimation of the amount of oxygen in the blood stream. It was assessed by Choice MMed MD300C2D pulse oximeter.
Health-Related Quality of Life (HR-QoL)
HRQOL of study participants of both the group (CHD and DM+ CHD group) was evaluated by short-form health survey (SF-36) questionnaire and a disease specific questionnaire Settle Angina Scale (SAQ). Health-related Quality of life of both the groups was evaluated by asking questions of both questionnaires (SF-36 and SAQ) to study participants and the responses were noted as the answer.
SF-36 is a non-disease specific instrument, containing of 36 questions, are divided into eight health domains, namely; physical functioning, social functioning, role limitations due to emotional problems, role limitations due to physical problems, bodily pain, vitality, mental health, and general health perception. The eight domains were scored from 0 to 100 indicating worst to best possible health status.
Settle Angina Questionnaire (SAQ) scale is a disease specific scale is a diabetes specific scale for assessing QOL of CHD patients; have 5 items covering domains; Physical Limitation, Angina Stability, Angina Severity, Treatment Satisfaction and Disease Perception. These five domains were scored from 0 to 100 indicating worst to best possible disease specific health related QoL.
Eecp Treatment
The ECP PSK machine having the model; P-ECP/TI was used for the treatment of diabetic and non-diabetic coronary heart disease patients. EECP, is an electro-mechanical device consist of three paired pneumatic cuffs applied to the lower leg, upper leg and buttocks. During treatment, the patient lies on EECP comfortable bed and cuffs are wrapped around patient’s legs and buttocks for one hour per day for treatment with 280 mmHg pressure. The cuffs inflate and deflate at specific times between patient’s heart beats. Cuffs inflate while the heart is at rest and deflate at the end of the rest period, just before next heartbeat. A continuous electro cardiogram (ECG), oxygen level and counter pulsation graph were monitored at the time of EECP treatment. An experienced doctor gives this EECP treatment for the one-hour session per day in seven consecutive weeks. All study subjects were followed up for 12 months after completion of EECP therapy.
Statistical Data Analysis
Collected data were analyzed with the help of Biostatistician using statistical package social sciences (SPSS) software version 21. Finally, 163 patients have been completed the whole study with 6, and 12 months the follow ups in which 82 participants were completed study follow-up from DM+CHD group and 81 from CHD group. Descriptive statistics with mean, percentage, Standard Deviation (SD) and chi-square was used to analyze the socio-demographic and clinical variables. Sample paired and independent t- test was used to assess significant differences of EECP within and between the DM+CHD and CHD group and data was analyzed with 95 % confidence interval with significant p-value <0.05.
Results
Demographic and baseline characteristics assessment of diabetic & non-diabetic CHD patients
Out of 212 patients, only 163 patients (82 participants from DM+CHD group and 81 patients from CHD group) were completed whole study with 12 months follow-up. The average age of study subjects were 59.6 ± 9.5 years. In this study the males participants (133) were higher as compare to female participants (30). The total number of rural subjects was 85 and urban was 78. The diabetic CHD group had higher numbers of urban subjects (56.4%) while CHD group had higher numbers of rural subjects (55.3%). Out of 212 patients 125 patients had obesity in which CHD group had higher number obese subjects 63.1% as compared to diabetic CHD group 36.9%. Total 91 subjects had hypertension in which Diabetic CHD had higher percentage 51.6% as compared to CHD group 48.4 % subjects.
Total 48 subjects had a family history of heart disease in which diabetic CHD had higher percentage 62.5 % as compared to CHD group 37.5 %. Total 36 subjects had a family history of diabetes and the diabetic CHD group had higher percentage 83.3% as compared to CHD group 16.7%. In this study total 77 subjects having the habit of smoking in which CHD group had higher percentage 51.9% as compared to diabetic CHD group 48.1 % and 25 subjects having the habit of chewing tobacco in which CHD group had higher percentage 83% as compared to diabetic CHD group subjects 16%. Out of 212 patients 62 subjects were physically active and CHD group had higher percentage 53.2% rate as compared to diabetic CHD group 46.8 %. In this study total 102 subjects were full of stress out of 163 in which diabetic CHD group Subjects having higher 50.8 % stress as compared to CHD group 49.2%. In this study out of 163 patients, 99 patients were vegetarian and vegetarian rate was higher in diabetic CHD group 52.5% as compared to CHD group 47.5%. The non-vegetarian rate was higher 53.1% in CHD group as compared to diabetic CHD group 46.9%.
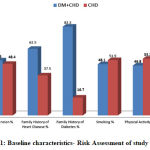 |
Figure 1: Baseline characteristics- Risk Assessment of study subjects. |
Discussion
Total 71 subjects had a history of MI in which diabetic CHD group had higher percentage 54.9% of MI history as compared to CHD group 45.1%. Total 35 subjects had the history of PCI and diabetic CHD had the higher percentage 62.9 % as compared to CHD group 37.1% and 75 subjects had the history of CABG in which diabetic CHD group had higher percentage 58.7% of CABG as compared to CHD group 41.3%. A significant difference in CABG history in this study was observed. In this study higher number of single vessel CHD 70 was observed and lower number 43 of double vessel CHD was observed. The number of single vessel CHD was equal 50% in both the groups. CHD group had a higher number of double vessel 62.8% as compared to diabetic CHD group 37.2 %. The diabetic CHD group had higher 60% rate of TVD as compared to CHD group 40%.
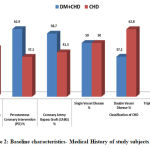 |
Figure 2: Baseline characteristics- Medical History of study subjects. |
Discussion
Effect of EECP on physiological profile
There was a minute difference in BMI was observed in diabetic and non-diabetic CHD group at 6th and 12th month. A significant improvement was also observed in systolic BP, diastolic BP and pulse in both diabetic and non-diabetic CHD group at 6th and 12th months of study follow up. That means EECP treatment is effective and significantly improves physiological parameters of both the groups approximately equal after EECP treatment.
Table 2: Changes in physiological measurements from baseline to 6- and 12-month follow-up
Outcome |
CHD Group (n=81) | CHD with DM Group (n=82) | ||
| Mean change (95% CI) from baseline | Mean change (95% CI) from baseline | |||
| 6-month | 12-month | 6-month | 12-month | |
| BMI | 2.28 (1.42 – 3.14) | 2.61 (1.63 – 3.59) | 2.17 (1.26 – 3.09) | 1.54 (0.54 – 2.54) |
| p-value | <0.0001 | <0.0001 | <0.0001 | 0.0029 |
| Systolic Blood Pressure | 4.71 (3.18 – 6.26) | 2.26 ( 1.21 – 3.31) | 4.74 (3.13 – 6.35) | 2.08 (0.94 – 3.21) |
| p-value | <0.0001 | <0.0001 | <0.0001 | 0.0005 |
| Diastolic Blood Pressure | 5.53 (3.08 – 7.96) | 0.04 ( -1.27 – 1.35) | 5.44 (3.51 – 7.36) | 1.85 (-0.69 – 4.39) |
| p-value | <0.0001 | 0.9497 | <0.0001 | 0.1519 |
| Pulse | 2.85 (2.16 – 3.55) | -0.12 (-0.86 – 0.63) | 3.05( 2.31 – 3.79) | 2.87 (1.74 – 3.99) |
| p-value | <0.0001 | 0.7502 | <0.0001 | <0.0001 |
Values are in mean (SD). Means differences within and between group are in mean (95% Confidence Interval), a negative change indicates a fall on average from baseline to 6 months and baseline to 12 months. Determined using repeated measures ANOVA a within groups comparison of mean difference, significant at p<0.05 are in bold letters
Effect of EECP on blood sugar levels
A significant reduction were observed in BSF, BSPP and HbA1c in diabetic CHD patients at 6th and 12th month follow-up after EECP treatment and this improvement in diabetic CHD patients can be due to the EECP treatment.
Table 3: Changes in Blood Glucose Profile in CHD with DM Group from baseline to 6- and 12-month follow-up
Outcome |
Blood Glucose Profile | |
| Mean change (95% CI) from baseline | ||
| 6-month | 12-month | |
| Fasting Blood Sugar | 8.72 (6.29 – 11.15) | 7.44 (4.21 – 10.67) |
| p-value | <0.0001 | <0.0001 |
| Blood Sugar PP | 13.0(11.44 – 14.57) | 13.48(10.98 – 16.06) |
| p-value | <0.0001 | <0.0001 |
| HbA1c | 6.58 (5.88 – 7.29) | 5.82 (4.67 – 6.96) |
| p-value | <0.0001 | <0.0001 |
Values are in mean (SD). Means differences within and between group are in mean (95% Confidence Interval), a negative change indicates a fall on average from baseline to 6 months and baseline to 12 months. Determined using repeated measures ANOVA a within groups comparison of mean difference, significant at p<0.05 are in bold letters
Effect of EECP on lipid profile
A statistical significant difference was observed in total cholesterol, triglyceride, HDL, LDL, VLDL, and Non-HDL in both diabetic and non-diabetic CHD group at 6th and 12th month. EECP may improve lipid parameters in coronary heart disease patients.
Table 4: Changes in lipid profile from baseline to 6- and 12-month follow-up
Outcome |
CHD Group (n=81) | CHD with DM Group (n=82) | ||
| Mean change (95% CI) from baseline | Mean change (95% CI) from baseline | |||
| 6-month | 12-month | 6-month | 12-month | |
| Cholesterol | 11.36 (9.57 – 13.15) | 7.15 (4.43 – 9.86) | 9.95 (8.18 – 11.72) | 12.59 ( 9.68 – 15.48) |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| Triglyceride | 11.19 (8.73 – 13.66) | 6.24 ( 4.53 – 7.95) | 10.45 (8.37 – 12.54) | 8.21 (5.06 – 11.37) |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| HDL | -15.74 (-18.73 – -12.76) | -12.5 (-15.41 – -9.59) | -18.84 (-22.49 – -15.19) | -22.27 (-26.28 – -18.26) |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| LDL | 19.87 (16.21 – 23.54) | 12.90 (7.81 – 17.98) | 17.57 (14.45 – 20.69) | 21.44 (16.51 – 26.38) |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| VLDL | -184.3(-214.28 – -158.28) | -224.3(-256.4 – -192.3) | -224.4(-256.4 – -192.4) | -198.1(-227.4 – -168.7) |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| Non-HDL | 17.96 ( 15.46 – 20.45) | 11.51 (7.84 – 15.19) | 16.22(13.98 – 18.46) | 19.78(16.15 – 23.38) |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
Values are in mean (SD). Means differences within and between group are in mean (95% Confidence Interval), a negative change indicates a fall on average from baseline to 6 months and baseline to 12 months. Determined using repeated measures ANOVA a within groups comparison of mean difference, significant at p<0.05 are in bold letters.
Effect of EECP on clinical symptoms
A significant change was observed in CCS angina classification score at 6th and 12th month follow-up in both diabetic and non-diabetic group. MRC score also showed the significant improvement within diabetic and non-diabetic group.
Table 5. Changes in clinical symptoms from baseline to 6- and 12-month follow-up
Outcome |
CHD Group (n=81) | CHD with DM Group (n=82) | ||
| Mean change (95% CI) from baseline | Mean change (95% CI) from baseline | |||
| 6-month | 12-month | 6-month | 12-month | |
| CCS Angina Class status | 26.85(22.88 – 30.83) | 27.57(21.47 – 33.67) | 20.73 (15.17 – 26.27) | 22.15( 14.89 – 29.41) |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| MRC Dyspnea Score | 9.97 (1.24 – 18.72) | 11.52 ( 1.70 – 21.34) | 24.18 ( 17.31 – 31.05) | 26.21 ( 18.57 – 33.86) |
| p-value | 0.0257 | 0.0221 | <0.0001 | <0.0001 |
Values are in mean (SD). Means differences within and between group are in mean (95% Confidence Interval), a negative change indicates a fall on average from baseline to 6 months and baseline to 12 months. Determined using repeated measures ANOVA a within groups comparison of mean difference, significant at p<0.05 are in bold letters
Effect of EECP on Physical functional capacity
A significant improvement was observed in Physical functional capacity, Cooper 12 minute walk test, VO2max and SpO2 at 6 months and 12 months follow up in both diabetic and non-diabetic CHD group. It means EECP may improve physical functional capacity in coronary heart disease patients with DM.
Table 6: Changes in physical functional capacity from baseline to 6- and 12-month follow-up
Outcome |
CHD Group (n=81) | CHD with DM Group (n=82) | ||
| Mean change (95% CI) from baseline | Mean change (95% CI) from baseline | |||
| 6-month | 12-month | 6-month | 12-month | |
| Spo2 Level | 97.76( 97.66 –12-Feb-201997.86) | 97.8 ( 97.65 – 97.94) | 97.68 (97.55 – 97.80) | 97.74 (97.57 – 97.90) |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| Cooper’s 12-minute Walk test status | -87.0(-98.86 – -73.16) | -83.1(-91.1 – -67.14) | -82.5(-98.5 – -66.5) | -80.5(-99.12 – -61.86) |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
Values are in mean (SD). Means differences within and between group are in mean (95% Confidence Interval), a negative change indicates a fall on average from baseline to 6 months and baseline to 12 months. Determined using repeated measures ANOVA a within groups comparison of mean difference, significant at p<0.05 are in bold letters
Effect of EECP on Health-Related Quality of Life
A statistical significant improvement was observed within both (diabetic & non-diabetic CHD) groups in almost all domains of SF-36 domains at 6th and 12 months. A significant change was also observed in vitality, social functioning, and general health at 6 months between the groups.
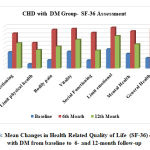 |
Figure 3: Mean Changes in Health Related Quality of Life (SF-36) of CHD with DM from baseline to 6- and 12-month follow-up |
Discussion
A statistical significant improvement was observed almost all domains of SAQ scale in both diabetic & non-diabetic CHD groups at 6th and 12 months as results were assessed through the independent t-test.
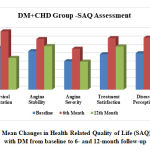 |
Figure 4: Mean Changes in Health Related Quality of Life (SAQ) of CHD with DM from baseline to 6- and 12-month follow-up |
Discussion
EECP effect on physiological profile
The present showed a minute change in BMI mean in diabetic and non-diabetic CHD patients which is not statistically significant. A study by Peter A Cullough et al showed a beneficial effect of EECP therapy on CHD obese patients having a higher BMI and similar findings we observed in our present study19.
A significant change was observed in SBP, DBP and pulse within diabetic and non-diabetic CHD group at 6 and 12 months after EECP treatment but no statistical significant difference was observed between the groups. Studies done by Dockery et al, and Braith et al shows that EECP treatment can significantly decrease SBP and DBP 24, 25. Several studies done by Nichols et al Kumar S et al and Subramanian R et al conclude that EECP treatment can reduce systolic and diastolic blood pressure in CHD patients 18, 20, 26.
EECP effect on biochemical parameters
The present study showed a significant improvement in total cholesterol, triglyceride, HDL, LDL, VLDL, and Non-HDL within diabetic and non-diabetic group at 6 and 12 months after EECP treatment that indicates the EECP is effective therapy to reduce cholesterol levels and improve HDL levels. Studies done by Braith et al and Tabary S Ziabakhsh et al observed in almost similar findings their studies hence they conclude that EECP maintain lipid profile 25,27. A statistical significant improvement was observed in BSF BSPP and HbA1c at 6 months and 12 months in diabetic CHD group subjects with significant p value <0.0001. Similarly studies done by Georgiann Linnemeier and J S Martin et al concluded that EECP may effective, and well-tolerated treatment for diabetic CHD patients 23,28.
EECP effect on Clinical Symptoms
The results of the Present study, showed a significant improvement in the clinical symptoms (angina and dyspnea) of diabetic and non-diabetic CHD patients after EECP treatment. A significant improvement was observed in CCS angina class score and MRC score of both diabetic and non-diabetic CHD group.
Studies done by Kozdag et al and Beck et al showed similar finding with Present study that mean showed significant improvement in CCS angina class score and MRC score of CHD patients 29,30. Petterson et al and Loh et al conducted research studies on the effectiveness of EECP on clinical symptoms of coronary heart disease patients revealed that EECP treatment provides both short and long term positive improvements on clinical symptoms of coronary heart disease 31,32. Ozlem Soran et al and Yavari et al studies conclude that EECP treatment had beneficial clinical effects and can improve clinical symptoms 33, 34. A study done by Erlding A et al also demonstrated that EECP could be more effective in patients having the history of severe angina 35. Our findings also verified the significant effects of EECP in patients having coronary heart disease.
EECP effect on Physical Functional Capacity
The results of the present study, showed a significant improvement in the physical functional capacity of diabetic and non-diabetic coronary heart disease patients after EECP and similar findings were reported by Rampengan et al and May et al in their study 36, 37. Before EECP treatment our study subjects were mostly poor in physical functional capacity but after EECP treatment they significantly improved. A significant effect of EECP treatment on CCS angina class and dyspnea improvement has been observed in this study in diabetic and non-diabetic coronary heart disease patients. Studies done by Chung Kuan Wu et al & Ziaeirad M et al have shown similar findings 38,39. The results of our study are in agreement with Petterson et al and Loh et al studies which have shown significant results on the effectiveness of EECP in patients with angina 31,32. Darren T Beck et al, and Casey DP et al study also indicated that EECP may be useful as an adjuvant therapy for improving functional capacity in CHD patients through reductions in blood pressure and improve myocardial oxygen demand for better physical functioning 40,41.
EECP effect on Health-Related QoL
The results of the present study showed significant improvement in health- related quality of life using both general SF-36 and disease specific SAQ scales in both diabetic and non-diabetic CHD patients. A study done by Arora RR et al reported a significant improvement in health – related quality of life especially in physical activity, general health and bodily pain using both general SF-36 and disease specific SAQ scales in CHD patients 17. Several studies done by Ziaeirad M et al et al. reported similar findings with present study that showed significant improvements in all domains of SF-36 a standard questionnaire of quality of life assessment 39. A Manchanda done by et al similar findings with present study and showed good results of EECP in respect of the improvement in the quality of life of heart patients 19,42.
Several studies done by the scientists Ozlem Soranet al, Ziaeirad M, and Nichols et al shows similar findings with present study and reported significant improvement in overall quality of life of CHD patients 26,33,39. Study done by Eslamian et al concluded that EECP therapy can improve the angina pectoris stability and severity of disease perception. Similarly, our study demonstrates that both diabetic and non-diabetic coronary heart disease patients get good results in almost all domains of SAQ quality of life assessment scale.
Studies done by Georgiann et al, Martin et al and Ramasamy et al validate the effectiveness of EECP towards glycemic control in DM patients 20,23,28. They conclude that EECP is an effective treatment for CHD and diabetes. It helps in lowering blood glucose level of alerting transport of insulin into skeletal muscle and thereby helps in glycemic control and ultimately improves the health-related quality of life of diabetic CHD patients. Our study reveals that EECP significantly improve the health-related quality of life and remained high for the following one year in diabetic and non-diabetic CHD patients. Jorgensen et al study demonstrates that the effect of EECP on quality of life sustained for three years in CHD patients 43.
Conclusion
The results of the present study recommend that EECP is a safe, beneficial, noninvasive treatment for diabetic and non-diabetic CHD patients, those not respond to routine invasive treatment In this study a significant improvement was observed in Heart Rate, SBP, DBP, Cholesterol, Triglyceride, HDL, LDL, VLDL, Non-HDL, BSF, BSPP, HbA1C, SpO2, Vo2max, 12 minute walk and exercise tolerance in diabetic and non-diabetic CHD patients equally. This non-invasive procedure also significantly improves the clinical symptoms (angina & dyspnea) of CHD patients with and without DM. Enhanced external counter pulsation therapy may also improve overall health-related quality of life of diabetic and non-diabetic CHD patients, including angina severity, angina stability and general health. Hence, the present study concludes that the EECP may improve physiological biochemical and clinical parameters with physical activity. This study also confirmed that EECP is well tolerated and proved to be an effective therapy for treatment of coronary heart disease patients with diabetes mellitus.
Acknowledgement
We are very thankful to SAAOL Heart Center, New Delhi, India and Amity University Haryana, India for providing us the relevant resources to complete this research and manuscript.
Conflict of Interest
There is no conflict of interest in relation to the publication of this manuscript.
Funding Source
Nil
References
- Pradeepa R, Mohan V. Prevalence of Type 2 diabetes and its complications in India and economic costs to the nation. Eur J Clin Nutr;71: 816–24 (2017).
- Prabhakaran Dorairaj, Panniyammakal Jeemon, Ambuj Roy. Cardiovascular diseases in India current epidemiology and future directions. Circulation; 133: 1605–20 (2016).
- Gandhi Andhuvan. Development and validation of patient information leaflet for heart attack patients. Int J Pharm Pharm Sci;8(8):381-3(2016).
- Mohammed K. Ali, K.M. Venkat Narayan , Nikhil Tandon. Diabetes and coronary heart disease: Current perspectives. Indian J Med Res; 132: 584-597(2010).
- Maniarasu K, Muthunarayanan L. Prevalence of certain chronic complications of diabetes among type 2 diabetic patients in rural population of Kancheepuram district, Tamil Nadu- A cross sectional study. Int J Med. Public Health; 7(1): 41-6 (2010).
- Jatinder Mokta, Kiran Mokta, Asha Ranjan, Mehak Garg. Prevalence of Cardiovascular Risk Factors among Diabetic Population and Awareness of Diabetes among Diabetic Patients: A Population Based Himalayan Study. Journal of the association of physicians of India; 65 (2) : 48-52 (2017).
- Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in non-diabetic subjects with and without prior myocardial infarction. N Engl J Med ; 339: 229–234 (1998).
- Jindrich S pinar. Hypertension and ischemic heart disease. Coretvasa; 54 :433–438 (2012
- Undurti N. Das. Obesity and its relationship to coronary heart disease. European Heart Journal;28 (23) : 2953-54 (2007).
- Robert H. Nelson. Hyperlipidemia as a Risk Factor for Cardiovascular Disease. Prim Care; 40(1): 195–211 (2013).
- S Department of Health and Human Services: Diabetes, Heart Disease, and Stroke, Livestrong.com: How does diabetes affect the heart, (2009).
- Cecilia C. Low Wang, Connie N. Clinical update: Cardiovascular disease in diabetes mellitus atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus – mechanisms, management, and clinical considerations. Circulation; 133: 2459–2502 (2016).
- Steen E Husted, E Magnus Ohman. Pharmacological and emerging therapies in the treatment of chronic angina. LANCET; 386 (9994):691-701 (2015).
- PC Block. Percutaneous transluminal coronary angioplasty. American Journal of Roentgenology;135: 955-959 (1980).
- Kannel WB. Bishop lecture. Contribution of the Framingham Study to preventive cardiology. J Am Coll Cardiol ;15(1):206-11 (1990).
- Fariba Zarani1, Gholamreza Sarami, Saeed Sadeghian. Adherence in CABG Patients: An Empirical Test of a Health Behavior Model. International Journal of Clinical Medicine; 5: 225-233 (2014).
- Arora RR, Chou TM, Jain D, Fleishman B, Crawford L, McKiernan T, et al. The multicenter study of enhanced external counter pulsation (MUST-EECP): Effect of EECP on exercise-induced myocardial ischemia and anginal episodes. J Am Coll Cardiol,;33(7):1833–1840 (1999).
- Kumar S, Lahiri TK. Enhanced external counterpulsation as an effective nonsurgical solution for ischemic heart disease patients. Heart India; 5(2): 55-60 (2017).
- Peter A. McCullough, Marc A. Silver, Elizabeth D. Kennard. Impact of body mass index on outcomes of enhanced external counter pulsation therapy. Am Heart J; 15: 9-13 (2006).
- Ramasamy Subramanian, Sushma Nayar, Chokkalingam Meyyappan. Effect of enhanced external counter pulsation treatment on aortic blood pressure, arterial stiffness and ejection fraction in patients with coronary artery disease. J Clin Diagn Res; 10: 30-4 (2016).
- Kumar Anil, Wilbert S. Aronow, Aniket Vadnerkar. Effect of enhanced external counter pulsation on clinical symptoms, quality of life, 6-minute walking distance, and echocardiographic measurements of left ventricular systolic and diastolic function after 35 days of treatment and at 1-year follow up in 47 patients with chronic refractory angina pectoris. Am J Ther; 16: 116–8 (2009).
- Kozdag G, Ertas G, Aygun F, Emre E, Kirbas A, Ural D et al. Clinical effects of enhanced external counter pulsation treatment in patients with ischemic heart failure. Anadolu Kardiyol Derg; 12: 214-21 (2012).
- Martin J. S., D. T. Beck, J. M. Aranda, R. W. Braith. Enhanced external counter pulsation improves peripheral artery function and glucose tolerance in subjects with abnormal glucose tolerance. J Appl Physiol;112: 868–76 (2012).
- Dockery F, Rajkumar C, Bulpitt CJ, Hall RJ, Bagger JP. Enhanced external counter pulsation does not alter arterial stiffness in patients with angina. Clin Cardiol; 27: 689-92 (2004).
- Braith RW, Conti CR, Nichols WW, Choi CY, Khuddus MA, Beck DT. Enhanced external counter pulsation improves peripheral artery flow-mediated dilation in patients with chronic angina a randomized sham-controlled study. Circulation; 122:1612-20 (2010).
- Nichols WW, Estrada JC, Braith RW, Owens K, Conti RC. Enhanced external counter pulsation treatment improves arterial wall properties and wave reflection characteristics in patients with refractory angina. J Am Coll Cardiol; 48: 1209–15 (2006).
- Shervinziabakhsh Tabary, Keyvan Yousefnejad, Taraneh Ziaee, Mehran Fazli. Assessment the clinical and para-clinical effects of enhanced external counter pulsation therapy in patients with coronary artery disease. Int J Med Invest; 4: 245-8 (2015).
- Georgiann Linnemeier, Martin K. Rutter, Gregory Barsness. Enhanced External Counterpulsation for the relief of angina in patients with diabetes: Safety, efficacy and 1-year clinical outcomes. Am Heart J; 146(3): 453-458 (2003).
- Kozdag G, Ertas G, Aygun F, Emre E, Kirbas A, Ural D et al. Clinical effects of enhanced external counter pulsation treatment in patients with ischemic heart failure. Anadolu Kardiyol Derg; 12: 214-21 (2012).
- Beck DT, Martin JS, Casey DP, Avery JC, Sardina PD, Braith RW. Enhanced external counter pulsation improves endothelial function and exercise capacity in patients with ischaemic left ventricular dysfunction. Clin Exp Pharmacol Physiol; 41: 628-36 (2014).
- Pettersson T, Bondesson S, Cojocaru D, Ohlsson O, Wackenfors A, Edvinsson L. One year follow-up of patients with refractory angina pectoris treated with enhanced external counterpulsation. BMC Cardiovasc Disord; 6 (28) : 1-7 (2006).
- Loh P. H., A. A. Louis, J. Windram. The immediate and long-term outcome of enhanced external counter pulsation in treatment of chronic stable refractory angina. J Intern Med; 259: 276–84 (2006).
- Soran Ozlem, Elizabeth D. Kennard, Abdallah Georges Kfoury. Two-year clinical outcomes after enhanced external counter pulsation therapy in patients with refractory angina pectoris and left ventricular dysfunction (report from the international EECP patient registry). Am J Cardiol; 97: 17–20 (2006).
- Yavari M, Montazeri H. Effects of enhanced external counter pulsation on anginal symptoms and improvements in objective measures of myocardial ischaemia: Cardiovascular topic. Cardiovasc J Afr; 18: 154-6 (2007).
- Erdling A, Bondesson S, Patterson T, Evvinsson L. Enhanced external counter pulsation in treatment of refractory angina pectoris: Two year outcome and baseline factors associated with treatment failure. BMC Cardiovasc Disord; 18: 39-43 (2008).
- Rampengan SH, Prihartono J, Siagian M, et al. The Effect of Enhanced External Counter pulsation Therapy and Improvement of Functional Capacity in Chronic Heart Failure Patients: A Randomized Clinical Trial. Acta Med Indones; 47(4):275-282 (2015).
- May O, Lynggaard V, Mortensen JC, Malczynski J. Scand. Enhanced External Counter pulsation – Effect on Angina Pectoris, QoL and Exercise Capacity after 1 Year. Cardiovasc J, ; 49 (1): 1-6 (2015).
- Chung-Kuan Wu, Huei-Fong Hung, et al. The immediate and one-year outcomes of dialysis patients with refractory angina treated by enhanced external counter pulsation. Clin. Nephrol,; 82(1):34-40 (2014).
- Ziaeirad M, Ziaei GR, Sadeghi N, et al. The Effects of Enhanced External Counter pulsation on Health related Quality Of Life in Patients with Angina Pectoris. Iran J Nurs Midwifery Res;17(1): 41–46 (2012).
- Darren T Beck, Darren P Casey, Jeffrey S Martin, et al. Enhanced External Counter pulsation Reduces Indices of Central Blood Pressure and Myocardial Oxygen Demand in Patients with Left Ventricular Dysfunction. Clin Exp Pharmacol Physiol, ; 42(4):315-320 (2015).
- Casey DP, Beck DT, Nichols WW, Conti CR, Choi CY, Khuddus MA, Braith RW. Effects of EECP on arterial stiffness and myocardial oxygen demand in patients with chronic angina pectoris. Am J Cardiol; 107(10): 1466-1472 (2011).
- Manchanda A, Soran O. Enhanced external counter pulsation and future directions: step beyond medical management for patients with angina and heart failure. J Am Coll Cardiol; 50 (16): 1523-1531 (2007).
- Jorgensen MT, May O. Improvement of angina, quality of life, and working capacity after enhanced external counterpulsation. Ugeskr Laeger; 175(3) : 114-116 (2013).








