Smita Shenoy1 , Abhijna Ballal R2*
, Abhijna Ballal R2* , Praveen Kumar S. E3
, Praveen Kumar S. E3 , Mamatha Ballal4
, Mamatha Ballal4 , Sohan Bangera5
, Sohan Bangera5 , Mohandas Rao KG6
, Mohandas Rao KG6 and Veena Nayak7
and Veena Nayak7
1Department of Pharmacology, Associate Professor, Kasturba Medical College, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India. 576104.
2Department of Pharmacology, Postgraduate, Kasturba Medical College, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India. 576104.
3Department of Pharmacology, Ph.D. Research Scholar, Kasturba Medical College, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India. 576104.
4Department of Microbiology, Professor, Kasturba Medical College, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India. 576104 .
5Department of Microbiology, Ph.D. Research Scholar, Kasturba Medical College, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India. 576104.
6Department of Anatomy, Professor and Head, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India. 576104.
7Department of Pharmacology, Associate Professor, Kasturba Medical College, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India. 576104.
Corresponding Author E-mail: abhijna.ballal@learner.manipal.edu
DOI : https://dx.doi.org/10.13005/bpj/1779
Abstract
The study was conducted to assess the effect of lignocaine and tramadol on healing of Staphylococcus aureus infected incision wound in rats. Incision wounds were created in three groups consisting of six rats in each group. The rats were infected with Staphylococcus aureus inoculum and the incision was closed. The rats were treated according to their group – Group I (Normal saline), Group II (2% Lignocaine) and Group III (5% Tramadol). All the drugs were applied topically, once a day for 10 days. The parameters measured to evaluate the wound healing was breaking strength, Colony Forming Units/ mL (CFU/ mL) of the tissue and histopathological examination. Data analysis was by one-way (Analysis of Variance) ANOVA followed by post hoc Tukey’s test. A significant difference (p<0.05 vs control) in the breaking strength and CFU/mL of tissue was observed between the control Group I and the test groups, Group II (2%lignocaine) and Group III (5% tramadol) when the drugs were used topically. Histopathological study did not show much difference in the morphology between the control and other groups, it revealed disorganised collagen fibres. This study suggests that lignocaine and tramadol do not impede healing of infected incision wound.
Keywords
Antibacterial; Breaking Strength; Colony Forming Units; Collagen; Incision; Staphylococcus Aureus
Download this article as:| Copy the following to cite this article: Shenoy S, Ballal R. A, Kumar P. S. E, Ballal M, Bangera S, Rao KG. M, Nayak V. A Comparative Study of the Effect of Lignocaine and Tramadol on Healing of Infected wound in Wistar Rats. Biomed Pharmacol J 2019;12(3). |
| Copy the following to cite this URL: Shenoy S, Ballal R. A, Kumar P. S. E, Ballal M, Bangera S, Rao KG. M, Nayak V. A Comparative Study of the Effect of Lignocaine and Tramadol on Healing of Infected wound in Wistar Rats. Biomed Pharmacol J 2019;12(3). Available from: http://biomedpharmajournal.org/?p=28869 |
Introduction
Wound healing involves restoration of the injured skin or other soft tissues. [1][2] The process of wound healing has different phases like increased vascularity, formation of extracellular matrix, inflammatory, proliferative and remodelling phases. [3] These phases of normal wound healing can be delayed by number of factors acting systemically and locally. Patient age, pre-existing diseases like diabetes mellitus, ischemia, tissue oxygenation, infection, etc lead to delayed healing. Contamination of wound with various pathogenic microorganisms and further colonization in the underlying tissues can cause necrosis. [4] The pathogens increase morbidity and mortality, prolong hospital stay and increase cost of treatment. Staphylococcus aureus is a common pathogen found in wound biopsy. Various topical treatments have been identified for control of infection caused by bacterial growth. Mupirocin is a standard treatment for infections caused by Staphylococcus aureus which prevents incorporation of isoleucine into the protein and thus exhibiting its antibacterial property. [5][6] Local anesthetic agents like lignocaine have been reported to have antimicrobial properties by causing ultrastructural changes, disruption, lysis of protoplast and altering the permeability of the cell membrane. [7][8] Various opioids have been shown to promote healing of cutaneous wounds but effect has not been seen on infected wounds. Tramadol, which is commonly used as an analgesic, has been reported to have local anesthetic property. [9] In addition, this synthetic analog of codeine is said to have antimicrobial property against some microbes. [10] There are hardly any studies on effect of these drugs on healing of infected wounds. Hence, this study was performed to study the effect of lignocaine and tramadol on healing of infected wounds in rats.
Materials and Methods
The experiment was conducted in the Central Animal Research facility, Manipal, Department of Microbiology, Kasturba Medical College, Manipal and Department of Anatomy, Melaka Manipal Medical College, Manipal.
The objective of the study was to evaluate the effects of lignocaine and tramadol on breaking strength, number of colony forming units /mL of tissue and histopathology of incision wound infected with Staphylococcus aureus in Wistar rats.
Chemicals and drugs
Thiopentone sodium (NICE Chemicals Pvt. Ltd., Kochi, India), 2% Lignocaine Hydrochloride gel, LOX -2% jelly (Neon laboratories Ltd., Mumbai, India), 2% Mupirocin ointment (Amideep pharmaceuticals, Gujarat, India), 5%Tramadol (Zydus Healthcare Ltd., East Sikkim, India), Normal saline (Fresenius Kabi Pvt. Ltd.,Kochi, India) , Paraffin (NICE Chemicals Pvt. Ltd., Kochi, India), Sheep Blood Agar Plates(HiMedia Laboratories Pvt. Ltd, Mumbai, India) were used in the study. Staphylococcus aureus strains were obtained from Department of Microbiology,Kasturba Medical College, Manipal.
Preparation of 5% tramadol ointment
5% Tramadol ointment was prepared using paraffin wax as a base. The ointment was freshly prepared every day and stored in an air tight container, labeled and maintained at room temperature.
Bacteria
The bacteria used in this study was a Gram-positive organism Staphylococcus aureus of clinical strain which was obtained from Department of Microbiology, Kasturba Medical College, Manipal. They were maintained at standard laboratory conditions.
Animals
Adult, healthy female Wistar albino rats, bred in Central Animal Research Facility, Manipal weighing 200-250 g were taken for the study. Standard housing, light and temperature conditions with continuous access to standard rat chow and water was provided to the rats. They were acclimatized to the laboratory conditions one week before the start of the experiment. The experiment was conducted for 10 days following approval from the Institutional animal ethics committee, according to the Committee for Control and Supervision of Experiments on Animals (CPCSEA) guidelines.
Study design
All the eighteen Wistar rats were randomly divided into three groups, with 6 in each.
Table 1 : Table showing Drug, Strain of the organism and number of animals used in the study
| Group | Drug | Strain of organism used | No. of animals used |
| Group I
(control) |
Normal saline, topical | Clinical strain | 6 |
| Group II
(Test) |
2% Lignocaine, topical | Clinical strain | 6 |
| Group III
(Test) |
5% Tramadol, topical | Clinical strain | 6 |
Incision wound model with infection
The rats of all groups were anesthetized with thiopentone sodium (30 mg/kg, intraperitoneally) and the incision area was shaved gently. Under aseptic conditions, the skin was incised vertically. The skin along with cutaneous muscle were raised. S. aureus in a concentration of 105 organisms/mL (total 0.2 mL) was inoculated into the wounds in Group I, Group II and Group III (105 inoculum was chosen because it is the necessary dose for induction of infection). [11] The wounds were mopped dry and closed with intermittent sutures at equal distance of 1 cm apart using black silk thread (No. 4) and round bodied needle. The drugs were applied topically once daily from day 1 to day 10. Sutures were removed on day seven. After ten days postoperatively, the rats were euthanized with thiopentone sodium given intraperitoneally. The following were assessed –
Breaking strength
Breaking strength of incision wound was measured in all the groups by continuous water flow technique of Lee. Force was applied on the wound in the form of the slow increase in weight of accumulating water and the resultant gaping of the tissue was noted. [12] The amount of accumulated water in the graduated bottle was quantified and the minimum weight of water required to tear the wound represented the breaking strength. Three such readings were taken for each rat. The mean breaking strength (g) obtained from each rat was calculated.
Colony Forming Units/mL
From the opened wounds, tissue was taken, and microbiological assessment was done to see the infection rates. For microbiological evaluation, CFU/mL of the sample was found out by serial dilution method. [9] The results were evaluated as follows 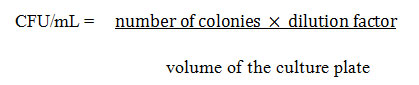
Histopathology
Histopathological evaluation of wound tissue was done by placing them in 10% formalin, tissue was then dehydrated using ethanol, embedded in paraffin, cut into thin sections and hematoxylin-eosin staining was done.
Statistical analysis
Analysis of data was by Statistical Package of Social Sciences (SPSS) software. To compare the means, one-way ANOVA was applied followed by post hoc Tukey’s test. p<0.05 was considered as statistically significant.
Results
Breaking strength
Tramadol and lignocaine enhanced the breaking strength (p< 0.05) in comparison to control. The breaking strength did not differ significantly between the test groups (Table 2).
Table 2: Effect of 2%lignocaine and 5% tramadol on breaking strength of wound
| GROUP | TREATMENT
(topical) |
BREAKING STRENGTH, g
(Mean±SD) |
| Group I | Normal saline | 314.1 ±30.40 |
| Group II | 2%Lignocaine | 437.5 ±46.77* |
| Group III | 5%Tramadol | 420.8 ±24.57* |
SD-standard deviation, *p ˂ 0.05 versus control
One-way ANOVA followed by post hoc Tukey’s test
Colony Forming Units/ml
The CFU/mL was counted after ten days post-instillation with 105 CFU/mL of S. aureus. There was a significant decrease in colony forming units /mL in the group treated with lignocaine and tramadol when compared with control. However, it did not differ between the test groups significantly (Table 3).
Table 3: Effect of 2%lignocaine and 5% tramadol on Colony Forming Units in the wound
| GROUP | TREATMENT
(topical) |
CFU/mL
(Mean±SD) |
| Group I | Normal saline | 3.933 ± 0.427×109 |
| Group II | 2% Lignocaine | 2.371 ± 0.421×109* |
| Group III | 5%Tramadol | 2.310 ± 0.531×109* |
SD-standard deviation, *p ˂ 0.05 vs control
One-way ANOVA followed by post hoc Tukey’s test.
Histopathological studies
Histopathology of the incision wound tissue showed various characteristics as shown in the Figure 1. Group I showed complete epithelialization and connective tissue of the dermis looked normal. The tissue in Group II showed good epithelialization and keratinization, collagen bundle formation has been initiated. The collagen fibres were not well organised; however, there were some areas which looked organised. Very few inflammatory cells are observed. In Group III, the tissue showed almost complete epithelialization. Collagen bundle formation was better than lignocaine group; not many inflammatory cells are observed. No evidence of edema was seen in any of the groups.
 |
Figure 1: Histopathology of incision wound model. (1a) Normal saline, (1b) 2% Lignocaine group, (1c) 5% Tramadol Group at 40x magnification. |
Discussion
In the present study, lignocaine and tramadol were evaluated for their effect on healing of the infected wound. S. aureus inoculum for wounds was selected because it is the commonly encountered pathogenic bacteria in surgical wounds.
Both tramadol and lignocaine increased the breaking strength of the infected wound. The histopathological reports did not show much difference between the tests and the control group. Epithelialization was complete in all the groups. Wound healing depends greatly on the production of collagen fibers. The amount of collagen fibers is one of the qualitative measures of the process of healing. During the initial phase of the healing (0-7 days), there is infiltration of inflammatory cells, granulation tissue formation and proliferation of epidermal cells. The later phase of the wound healing process (9-18 days) involves collagen formation and remodeling. [14]
The healing of wounds is disturbed by several factors including invasion by microorganisms. Staphylococcus aureus is the most frequently encountered pathogen in skin wounds detected by the neutrophil response to the infection. The pathogen escapes the defensive response of the body by several mechanisms. It obstructs chemotaxis, escapes the produced antibodies, forms a polysaccharide coat or biofilms and hides from detection. The complexity of the infection is increased by the emergence of methicillin resistant Staphylococcus aureus which has multiple virulence factors that result in abscesses, lysis of human white blood cells (WBCs) and increase the morbidity, hospital stay and mortality in patients. [15]
The standard treatment for staphylococcus skin infections is topical Mupirocin ointment. Local anesthetics are said to have wound healing and antibacterial effect. In our study, lignocaine and tramadol decreased the microbial load of the wound. A study by Sakuragi and his colleagues reported that exposure of 2% Lignocaine in the presence or absence of preservatives did not show significant bactericidal activity. [16] But, when the specimens were collected and cultured within 2 hours of exposure to 1% lignocaine, Miller and Shelley stated that there is a significant decrease in colony counts. [17] Craig et al. conducted an in-vitro study where lignocaine in a concentration as low as 0.5% inhibited S. aureus. The bacteria was incubated for 24 h at 370 C. Lignocaine was said to have a time-dependent inhibitory effect as reported by Parr et al., first 2 hours showed slight inhibition in the colonies while the maximum destruction of all bacteria was observed in the initial 8 hours.[18] A recent study conducted by H. Farzam and his colleagues showed that when tramadol was injected in doses of 12.5 and 25 mg/ml, there was no significant impact on the diameter of the lesions caused by Staphylococcus aureus at 24 and 48 hours or Pseudomonas aeruginosa at 24 hours. However, they found an increase in diameter of inflammation at 48 hours at the doses 12.5 and 25 mg/mL in P. aeruginosa. [19]
The probable mechanism by which local anesthetics exert antibacterial effects on bacteria are by interfering with cell membrane, modifying DNA synthesis, lysis of protoplasts, and ultrastructural changes. Membrane-bound enzymes are also inhibited by them. [11] There was no negative impact on the wound healing as reported by some of the studies. This study agrees with Yunus Oktay Atalay and his colleagues that local anesthetics do not impair cutaneous wound healing. [20] Though many in vitro analysis have proven the antibacterial effect of tramadol, the exact mechanism by which the antibacterial effect is carried out is not yet clear. It has been suggested that the action may be due to its local anaesthetic property and the changes in the cell membrane of the microorganism. [10]
Opioids like morphine, fentanyl are checked for their effect on wounds. µ-opioids receptors present on the keratinocytes gets activated by opioid agonists and results in upregulation of the type II transforming growth factor-β(TGF- β) which is responsible for regeneration of epithelial cells in acute wounds and cytokeratin 16(CK16) which is a filament protein exclusively expressed during wound healing.[21] Poonawala et al. tested the effect of topical application of opioids on ischemic delayed open-wound healing model in rats and observed an increase in granulation tissue and collagen formation. There was an increase in healing process also due to an increased epidermal and dermal organisation. [22] Tramadol, which is an analogue of codeine, acts through weak interaction with the mu opioid receptors. In addition, it also prevents the reuptake of 5 HT and epinephrine, hence modulating the pain. The serotonin present in the synaptic cleft plays a key role in upregulation of pro- inflammatory cytokines like TGF-β1, especially in the inflammatory and proliferative phase thus promoting wound healing and closure. Serotonin is also known to decrease apoptosis of cells. [23] This may be the possible reason for the healing of wounds by tramadol treated group. In addition to the healing effect shown by tramadol, its use also adds to the analgesic advantage provided to the patient.
Conclusion
The results of this study suggest that wound healing was not affected adversely by the topical application of Lignocaine and Tramadol; hence they can be used even in slow healers without the need for caution.
Acknowledgement
The authors express their gratitude to HOD department of Pharmacology, KMC, Manipal, Department of Anatomy, MMMC, Manipal, department of Microbiology, KMC, Manipal and Manipal Academy of Higher Education of their support and help.
Conflicts of Interests
All authors have none to declare.
References
- Malviya N, Jain S. Wound healing activity of aqueous extract of Radix paeoniae root. Acta Pol Pharm. 2009;66(5):543–7.
- Lindsay S, Oates A, Bourdillon K. The detrimental impact of extracellular bacterial proteases on wound healing. Int Wound J. 2017;14(6):1237–47.
- Nayak BS, Marshall JR, Isitor G. Wound healing potential of ethanolic extract of Kalanchoe pinnata Lam . leaf — A preliminary study. 2010;48(June):572–6.
- Robson MC. A Failure of Wound Healing Caused by imbalance of bacteria. Surg Clin North Am. 1997;77(3):637–50.
- Gisby J, Bryant J. Efficacy of a new cream formulation of mupirocin: Comparison with oral and topical agents in experimental skin infections. Antimicrob Agents Chemother. 2000;44(2):255–60.
- Spann CT, Turtrone WD, Weinburg JM, Scheinfeld N, Ross B. Topical Antibacterial Agents for Wound Care:A Primer. Dermatol Surg. 2003;29:620–626.
- Wachowski I, Jolly DT, Hrazdil J, Galbraith JC, Greacen M, Clanachan AS. The growth of microorganisms in propofol and mixtures of propofol and lidocaine. Anesth Analg. 1999;88(1):209–12.
- Johnson SM, Saint John BE, Dine AP. Local Anesthetics as Antimicrobial Agents: A Review. Surg Infect (Larchmt). 2008;9(2):205–13.
- Vahabi S, Heidari M, Ahmadinejad M, Akhlaghi J, Birjandi M. Comparison of local anesthetic effects of tramadol and lidocaine used subcutaneously in minor surgeries with local anesthesia. Middle East J Anaesthesiol. 2011;21(1):9–14.
- Shacoori T, Shacoori V, Gougeon A, Vo Van J, Repere M, Donnio M, Mallet M. The Antibacterial Activity of Tramadol Against Bacteria Associated with Infectious Complications After Local or Regional Anesthesia. International Anesthesia Research Society.2007;105(2):524-7.
- Kose AA, Karabaǧgli Y, Kiremitci A, Kocman E, Cetin C. Do local anesthetics have antibacterial effect on staphylococcus aureus under in vivo conditions? An experimental study. Dermatologic Surg. 2010;36(6):848–52.
- Lee KH. Studies on the Mechanism of Action of Salicylate II. Retardation of Wound Healing by Aspirin. J Pharm Sci. 1968;57(6):1042–3.
- Suvarna SK, Layton C (Histologist), Bancroft JD. Bancroft’s theory and practice of histological techniques. 536 p.
- Mcdougall S, Dallon J, Sherratt J, Maini P. Fibroblast migration and collagen deposition during dermal wound healing: mathematical modelling and clinical implications. Phil Trans R Soc A. 2006;364:1385–405.
- Tong SYC, Davis JS, Eichenberger E, Holland TL, Fowler VG. Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management. Clin Microbiol Rev. 2015;28(3):603–61.
- Sakuragi T, Ishino H, Dan K. Bactericidal activity of clinically used local anesthetics on Staphylococcus aureus. Reg Anesth. 1996;21(3):239–42.
- Miller MA, Shelley WB. Antibacterial Properties of Lidocaine on Bacteria Isolated From Dermal Lesions. Arch Dermatol. 1985;121(9):1157.
- Parr AM, Zoutman DE, Davidson JS. Antimicrobial activity of lidocaine against bacteria associated with nosocomial wound infection. Ann Plast Surg. 1999;43(3):239–45.
- Farzam H, Farahani A, Tafkik A, Gorgin Karaji A, Mohajeri P, Rezaei M, et al. Antibacterial effect of tramadol against Staphylococcus aureus and Pseudomonas aeruginosa: an in vivo study. New Microbes New Infect. 2018;24:42–6.
- Atalay YO, Umuroglu T, Yagmur C, Gogus FY, Bozkurt S. The comparative effects of local anaesthetics on wound healing in rats: Bupivacaine vs Levobupivacaine. J Exp Clin Med. 2016;33(2):93–8.
- Shanmugam VK, Couch KS, Nish S Mc, Amdur RS. Relationship between Opioid Treatment and Rate of Healing in Chronic Wounds. Wound Repair Regen . 2017 January ; 25(1): 120–130.
- Poonawala T, Levay-Young BK, Hebbel RP, Gupta K. Opioids heal ischemic wounds in the rat. Wound Repair Regen. 2005;13(2):165–74.
- Shah A, Amini-nik S.The role of serotoninergic system in skin healing. Int. J. Drug Res. Tech. 2017, Vol. 7 (3), 80- 106.








