Manuscript accepted on :15-April-2019
Published online on: 09-05-2019
Plagiarism Check: Yes
Reviewed by: Abdullah Noohu
Second Review by: Srini Vasan
Tamilisetti Vidya Sagar1 , Sanjay Kumar*1
, Sanjay Kumar*1 , Kagita Venkata Durga Navyamani2
, Kagita Venkata Durga Navyamani2 and Shantilata Patnaik3
and Shantilata Patnaik3
1Department of Pharmacology, GSL Medical College, Rajahmundry, India.
2Department of ENT, Rangaraya medical College, Kakinada, India.
3Department of Pharmacology, IMS and SUM Hospital, SOA University, Bhubaneswar, India.
Corresponding Author E-mail: sanjaykumarimssum@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1713
Abstract
Sore throat is a common presentation in outdoor patient setting, mostcases of sore throat are viral in aetiology and do not require antibiotics, it is a common practice to prescribe antibiotics to all patients presenting with sore throat without identifying aetiology, purpose of this study was to determine antimicrobial prescription pattern in patients with acute sore throat.This is a descriptive and observational study, observed participants without providing any interventions, after fulfilling inclusion and exclusion criteria, patients were enrolled into study and informed written consent was obtained from all patients after a detailed explanation prior to enrolment, data was obtained from medical records, analysed descriptively and Modified Centor scoring system was used to determine appropriateness of antibiotics, results depicted in the form of tables and figures. A total of 90 patients, who presented with sore throat were enrolled for the study. Inflammation of posterior pharyngeal wall was observed in 77% patients, while exudate was seen in 50%, tonsils were enlarged in 11% cases and cervical lymphadenopathy was present in 1.1%. Analysis of prescriptions showed that beta lactams,were widely prescribed antibiotics, followed by macrolides,followed by quinolones and aminoglycosides and 50% patients received antibacterial monotherapy, whereas 50% were on multiple antibacterial drug therapy, prescribing multiple antimicrobials without any culture sensitivity was encountered in this study and there were less generic drugs prescribed. There is a need of educational programmes in order to bring rational use of antibiotics and empirical prescription of antibiotics for sore throat in most cases is unjustified and the practice must be discouraged.
Keywords
Antibiotics; Beta Lactams; Centor Score; Generic Drugs; Inappropriate Prescribing
Download this article as:| Copy the following to cite this article: Sagar T. V, Kumar S, Navyamani K. V. D, Patnaik S. Patterns of Antimicrobial Therapy for Sore Throat in A Teaching Hospital of India. Biomed Pharmacol J 2019;12(2). |
| Copy the following to cite this URL: Sagar T. V, Kumar S, Navyamani K. V. D, Patnaik S. Patterns of Antimicrobial Therapy for Sore Throat in A Teaching Hospital of India. Biomed Pharmacol J 2019;12(2). Available from: https://bit.ly/2DYVdKd |
Introduction
Acute sore throat is one of the commonest complaints in medical practice, most of these cases are viral in aetiology and do not require antibiotics.1,2,3 Among healthy individuals with acute pharyngitis, the only bacterial pathogen of concern, which requires antibiotic treatment is Group A Streptococcus because of its potential to cause rheumatic fever4. However, it is a common practice to prescribe antibiotics to all patients presenting with sore throat without identifying aetiology by either throat swab culture or streptococcal antigen detection, such practices lead to a waste of resources, expose patients to potentially harmful side effects of drugs and promote development of resistance in the bacteria.2,3
Original Centor score uses four signs and symptoms to estimate probability of acute streptococcal pharyngitis in adults with a sore throat,5 score was later modified by adding age and validated in adults and children,6,7cumulative score determines likelihood of streptococcal pharyngitis and need for antibiotics, arguments for antibiotic treatment include acute symptom relief, prevention of suppurative and nonsuppurative complications, and reduced communicability.8, 9,10, 11
The purpose of this study was to determine antimicrobial prescription pattern in patients with acute sore throat.
Materials and Methods
Study was undertaken in collaboration with department of ENT at Government General Hospital, Kakinada, conducted for a period of 3 months. Institutional ethical committee clearance was taken. This is a descriptive and observational study where participants were observed without providing any interventions related to treatment prescribed and then results are presented descriptively.
After fulfilling the inclusion and exclusion criteria, patients were enrolled into the study and informed written consent was obtained from all patients after a detailed explanation prior to enrolment, patients presenting with sore throat, who were prescribed antibiotics were included in the study, patients who were taking or had taken antibiotics during the last 48 hours were excluded, results were depicted in the form of tables and Figures. Microsoft word and excel are used to generate figures and tables.
Results
A total of 90 patients were enrolled into the study out of which 46 (51.11%) were male patients and 44 (48.89%) were female patients; patients ranging from 16 to 60 years are included in the study.A modified Centor score, which also considers patient’s age, was calculated for all patients who met inclusion criteria.
Table 1: Modified Centor scoring system points.
| Criteria | Points |
| Absence of cough | 1 |
| Swollen tender anterior cervical nodes | 1 |
| Temperature >100.4 F | 1 |
| Tonsillar exudates | 1 |
| Age <15 | +1 |
| Age >44 | -1 |
Table 2: Modified Centor scoring system and risk of streptococcus infection for acute pharyngitis patients.
| Centor | Risk of streptococcus infection |
| <0 | 1-2.5% |
| 1 | 5-10% |
| 2 | 11-17% |
| 3 | 28-35% |
| >4 | 51-53% |
Table 3: Guidelines for management.
| -1,0 or 1 point | No antibiotic or throat culture necessary |
| 2 or 3 points | Should receive throat culture and treat with an antibiotic if culture is positive |
| 4 or 5 points | Consider rapid strep testing and or culture (risk of strep. Infection is >50%) |
Table 4: Showing frequency of presenting complaints, clinical findings and percentage.
| Presenting complaint | Frequency | Percentage |
| Sore throat | 90 | 100% |
| Cough | 70 | 77% |
| Clinical findings | ||
| Inflammation of posterior pharyngeal wall/tonsils | 70 | 77% |
| Exudate on posterior pharyngeal wall/tonsils | 45 | 50% |
| Enlarged tonsils | 10 | 11% |
| Follicular tonsillitis | 10 | 11% |
| Cervical lymphadenopathy | 1 | 1.1% |
 |
Figure 1: Bar diagram showing frequency of presenting complaints, clinical findings and percentage.
|
Table 5: Showing Percentage of Various antibiotics prescribed in study population.
| Antibiotics prescribed | Percentage |
| Penicillins | 50% |
| Cephalosporins | 20% |
| Macrolides | 20% |
| Flouroquinolones | 8% |
| Aminoglycosides | 2% |
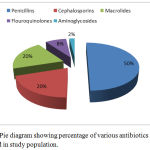 |
Figure 2: Pie diagram showing percentage of various antibiotics prescribed in study population.
|
It was observed that most commonly prescribed antimicrobials were β-lactams followed by macrolides, quinolones and aminoglycosides.
Table 6: Showing details of prescriptions with brand name and generic name.
| Prescribing practice | Number of prescriptions | Percentage |
| Brand name | 80 | 80% |
| Generic name | 20 | 20% |
 |
Figure 3: Bar diagram showing details of prescriptions with brand name and generic name.
|
Table 7: Showing Pattern of prescriptions.
| Prescription containing number of drugs | Number of prescriptions | Percentage |
| 1 | 50 | 50% |
| 2 | 40 | 40% |
| 3 | 10 | 10% |
Prescriptions showed that 50% patients received antibacterial monotherapy, whereas 50% were on multiple antibacterial drug therapy, among those who received multiple antibacterial therapies,40% received two drug therapies and 10% received three drug therapies.
Discussion
Ideally, throat swab cultures should be performed, which not only confirm the presence of Group-A Streptococci but also provide antimicrobial susceptibility report,5,12however, culture results take 48-72 hours and require follow-up visits, whileculture facilities are not widely available in under-developed countries. Rapid antigen detection tests (RADTs) for streptococcal antigens on throat swabs are bedside procedures, which provide immediate results but they may not be freely available,5,12 in the absence of these facilities, clinical criteria such as Centor score or its modification can be used to rule out streptococcal throat infection with reasonable confidence.5.McIsaac modification of Centor score assigns a low probability of streptococcal throat infection in the presence of cough and absence of cervical lymphadenopathy and tonsillar swelling/ exudates.13,14Majority of our patients (77%) complained of cough, while only a few had enlarged tonsils (11%) or cervical lymphadenopathy (2.2%),clinical findings alone should have precluded the use of antibiotics in most of these patients.
Injudicious use of antibiotics is a global problem, which is escalating healthcare costs, exposing patients to side effects of drugs and promoting antimicrobial drug resistance,2,3 studies from around the world have highlighted this problem with prescription rates varying from 35% to 80%.2,15,16
In our study,demographic characteristics showed that males were found to be predominant sufferers from ENT infections than females which might be attributed to occupational reasons and poor hygiene, similar findings were also reported in studies conducted by Yadav et al., Ain et al., Shankar et al. and Pradhan et al.17, 18, 19, 20
In our study most commonly prescribed category of antimicrobials were β-lactams followed by macrolides and quinolones, these results are similar to study conducted by Khan et al.21
The average number of antimicrobial agents prescribed per patient per course was found to be slightly high, these results are similar to studies conducted by Ain et al. and Das et al 18,23 Since it is an important indicator for assessing rationality of prescription, physicians should try to keep the average number of drugs per prescription to a minimum as higher values results in increased risk of drug interactions, adverse drug effects, development of bacterial resistance and increased cost of treatment.
Prescription by brand name is an issue that needs to be addressed; generic prescribing is more cost effective, associated with less potential for errors and is therefore encouraged by all prescribers.
Different strategies have been proposed to overcome the problem of irrational use of antibiotics, aggressive programmes to educate doctors, utilization of clinical decision rules like Centor score and wider availability of RADTs can help in reducing injudicious use of antibiotics for sore throat.
Limitations
Duration of study was short; hence effect of seasonal variation could not be determined, on generalizability of study findings as the study was carried out at a single centre, further large scale research is required for detail evaluation.
Conclusion
Prescribing multiple antimicrobials without any culture sensitivity was encountered in this study and there were less generic drugs prescribed, dedicated training hours onprescribing of antimicrobials in ENT diseases for doctors along with regular prescription audit will help promote rationale use of antimicrobials in the long run.
Acknowledgements
The authors acknowledge the help provided by the ENT department of the hospital and also acknowledge the guidance of Dr Sanjay Kumar, Professor, Department of Pharmacology, GSL Medical College, Rajahmundry in drafting the manuscript. Authors are deeply indebted to Dr Shantilata Patnaik, Professor, Pharmacology, for her valuable suggestions.
Conflict of Interest
There is no conflict of interest.
References
- Worrall G. Acute sore throat. Can Fam Physician. 2011; 57: 791-4.
- Ayranci U, Akgun Y, Unluoglu I, Kiremitci A. Antibiotic prescribing patterns for sore throat infections in a university-based primary care clinic. Ann Saudi Med. 2005; 25: 22-8.3.
- Park SY, Gerber MA, Tanz RR, Hickner JM, Galliher JM, Chuang I, et al. Clinicians’ management of children and adolescents with acute pharyngitis. Pediatrics.2006;117: 1871-8.
- Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the emergency room.MedDecis Making. 1981; 1(3):239-246.
- McIsaac WJ, Goel V, To T, Low DE. The validity of a sore throat score in family practice. CMAJ. 2000; 163(7):811-815.
- Ebell MH. Making decisions at the point of care: sore throat. FamPractManag. 2003; 10(8):68-69.
- Cooper RJ, Hoffman JR, Bartlett JG, et al., for the American Academy of Family Physicians, American College of Physicians, American Society of Internal Medicine, Centres for Disease Control and Prevention. Principles of appropriate antibiotic use for acute pharyngitis in adults: background. Ann Intern Med. 2001; 134(6):509-517.
- American Academy of Paediatrics, Committee on Infectious Diseases.Red Book. 26th ed. Elk Grove Village, Ill.: American Academy of Paediatrics; 2003:578-580.
- Dajani A, Taubert K, Ferrieri P, Peter G, Shulman S. Treatment of acute streptococcal pharyngitis and prevention of rheumatic fever: a statement for health professionals. Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young, the American Heart Association.Paediatrics. 1995; 96 (4 pt 1):758-764.
- Centor RM, Allison JJ, Cohen S. Pharyngitis management: defining the controversy. J Gen Intern Med. 2007; 22(1):127-130.
- Anjos LM, Marcondes MB, Lima MF, Mondelli AL, Okoshi MP. Streptococcal acute pharyngitis. Rev Soc Bras Med Trop. 2014; 47: 409-13
- McIsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE. Empirical validation of guidelines for the management of pharyngitis in children and adults.JAMA.2004; 291: 1587-95.
- Yuniar CT, Anggadiredja K, Islamiyah AN. Evaluation of rational drug use for acute pharyngitis associated with the incidence and prevalence of the disease at two community health centres in Indonesia. Sci Pharm. 2017; 85.
- Mazzaglia G, Caputi AP, Rossi A, Bettoncelli G, Stefanini G, Ventriglia G, et al. Exploring patient- and doctor-related variables associated with antibiotic prescribing for respiratory infections in primary care. Eur J ClinPharmacol. 2003; 59 (8-9): 651-7.
- Kumar S, Little P, Britten N. Why do general practitioners prescribe antibiotics for sore throat? Grounded theory interview study.BMJ.2003; 326: 138.
- Yadav P, Kanase V, Lacchiramka P, Jain S. Drug utilization trends in ent outpatient department in a teaching hospital. Int J Pharma Bio Sci, 2010; 1: 153-159.
- Ain MR, Shahzad N, Aqil M, Alam MS, Khanam R. Drug utilization pattern of antibacterials used in ear, nose and throat outpatient and inpatient departments of a university hospital at New Delhi, India. J Pharm BioalliedSci, 2010; 2: 8-12.
- Shankar PR, Upadhyay DK, Subish P, Dubey AK, Mishra P. Prescribing patterns among pediatric inpatients in a teaching hospital in western Nepal. Singapore Med J, 2006; 47: 261-265.
- Pradhan S, Jauhari AC. A study of antibiotics used in adult respiratory disorders in Kathmandu and Bhaktapur. Nepal Med Coll J, 2007; 9: 120-124.
- Khan FA, Nizamuddin S, Salman MT. Patterns of prescription of antimicrobial agents in the Department of Otorhinolaryngology in a tertiary care teaching hospital. Afr J Pharm Pharmacol, 2011; 5: 1732-1738.
- Das BP, Sethi A, Rauniar GP, Sharma SK. Antimicrobial utilization pattern in outpatient services of ENT department of tertiary care hospital of Eastern Nepal. Kathmandu Univ Med J, 2005; 3: 370-5.







