Manuscript accepted on :05-Nov-2018
Published online on: 28-11-2018
Plagiarism Check: Yes
Reviewed by: Felix-Martin Werner
Second Review by: M. Mohan Varma
Final Approval by: Dr. Ayush Dogra
Sujata Jadhav and Chitra Khanwelkar
Department of Pharmacology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
Corresponding Author E-mail: drjadhavsujata@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1563
Abstract
Acute respiratory tract infections (ARTI) are very common in all age groups. Childhood respiratory tract infections are responsible for considerable morbidity and mortality. It is significant health problem in India also. The World Health Organization (WHO) estimates that 2 million children under five years of age die due to pneumonia. Majority of ARTIs have viral etiology. Rhinoviruses, respiratory syncytial viruses, parainfluenza and influenza viruses, human metapneumovirus, and adenoviruses are main causative agents. Among bacteria, group A streptococci, Corynebacterium diphtheriae, N. meningitides, H. influenzae, pneumococcus and Staphylococcus aureus are responsible for ARTIs. Drug utilization studies help to understand the pattern of prescription in that particular area for specific conditions.We included children from one to five years of age, diagnosed as ARTI and evaluated 298 prescriptions given to these children. Analysis of these prescriptions was done as well as they are compared with WHO prescription indicators. Cough (96%), fever (93%) and rhinitis (82.5%) were common symptoms observed, but sore throat, earache and breathlessness were also present in these children. Average number of drugs prescribed was 4.1/patient. Following drugs were prescribed, Antipyretics 98.3%, antimicrobials 91.3%, antihistaminics and cough syrups in 75.2%, Leukotriene antagonist in 25.1% patients, Vitamin B complex 11% and glucocorticoids 4.6%. All drugs were prescribed by brand names and not by generic name. 97.3% prescribed drugs were from national list of essential medicine. We found overuse of antimicrobials in our study. Educational programs are needed in order to bring rational use of antimicrobials. At the same time awareness in parents also should be done regarding antimicrobial use.
Keywords
ARTI; Antimicrobials; Essential Medicine; Prescriptions; Pediatric; WHO
Download this article as:| Copy the following to cite this article: Jadhav S, Khanwelkar C. Prescribing Pattern of Drugs in Acute Respiratory Tract Infection in Children Aged 1 To 5 Years At Tertiary Care Teaching Hospital. Biomed Pharmacol J 2018;11(4). |
| Copy the following to cite this URL: Jadhav S, Khanwelkar C. Prescribing Pattern of Drugs in Acute Respiratory Tract Infection in Children Aged 1 To 5 Years At Tertiary Care Teaching Hospital. Biomed Pharmacol J 2018;11(4). Available from: http://biomedpharmajournal.org/?p=24362 |
Introduction
Acute respiratory tract infections (ARTIs) are more frequent than infections of any other organ in human being. They are common in all age groups, but childhood acute respiratory infection is major public health problem all over the world including India. Especially pneumonia is a major cause of morbidity as well as mortality in a pediatric age group. According to UNICEF survey of 2006 in children less than five years, ARTIs especially pneumonia was attributed for 20% mortality. If neonatal pneumonia is included, this may rise upto 35-40%. It will account for 2.04 milllion deaths per year.1
Acute respiratory tract infection (ARTI) is defined as respiratory symptoms lasting for less than 3 weeks in that episode. On an average there are 3-6 episodes of ARTIs annually are observed in children under five. These ARTIs are the most common reasons for pediatric consultations in primary health care system.2 This is one of the major reasons for absenteeism from work for their parents also.
Upper respiratory tract infections include rhinitis (common cold), sinusitis, ear infections, acute pharyngitis or tonsillopharyngitis, epiglottitis and laryngitis. Most of the URTIs have a viral etiology but these may predispose the children for bacterial infections also. Amongst above URTIs, ear infections may cause deafness while pharyngitis due to group A beta haemolytic streptococci may be responsible for rheumatic fever as a serious complication. LRTIs include epiglottitis, laryngitis, laryngotracheitis, bronchitis, bronchiolitis and pneumonia.3,4,5
Rhinoviruses, respiratory syncytial viruses (RSV), parainfluenza and influenza viruses, human metapneumovirus and adenovirsues are common causative viruses for ARTI. Amongst this, Rhinovirus account for 25-30% acute URTIs and coronovirus for 10%, while other viruses account for 25-35%. According to WHO, in developing countries, ARTI caused by RSV is responsible for almost 6 lakhs deaths per year.6
Among bacteria, group A streptococci take the lead, though Corynebacterium diptheriae, N meningitides are also responsible for ARTI. H. influenza, Pneumococcus and Staphylococcus aureus are responsible for superimposed infections, and may cause complications of ears sinuses, mastoids, lymph nodes and lungs. Corynebacetrium diptheriae can cause acute pharyngitis and development of membrane on the throat. This is more common in developing countries. Now a days because of availability and awareness of vaccination, incidence of diphtheria has been declined.
Common symptoms of ARTIs are fever, running nose (rhinorrhoea), cough, sore throat, earache and breathlessness. Bodyache is observed along with other symptoms. Most of the times more than one symptoms are observed. They may last for more than three to ten days also. So the main aim of the treatment is to give the symptomatic relief.
The study of drug utilization in different conditions or diseases is very useful as it has great importance in pharmacoepidemiology. Its importance is still increasing because of their association with other areas like public health, pharmacoeconomics and pharmacovigilance.
The aim of our study is to analyze the prescribing pattern of medicines used in treatment of ARTIs in children who are below the age of 5 years and also to evaluate the rationality of the prevalent prescribing pattern with WHO indicators.
Many studies are conducted in which patients of respiratory tract infections included from different age groups e.g. one to twelve years or all age groups or only above 5 years of age.
We conducted study on children of the age group range from one to five years, as .this group is more vulnerable for repeated attacks of respiratory tract infections.
Methodology
The study was conducted in department of pharmacology, Krishna Institute of Medical Sciences, Karad and department of pediatrics, Krishna Hospital and Research center, Karad after taking the permission from Institutional ethics committee. The study is prospective and cross-sectional. Data were collected in the period of August 2014 to August 2017.
Inclusion Criteria
Patients of age group between one to five years of either sex, suffering from acute respiratory tract infections were included in the study.
Exclusion Criteria
Patients of other co-morbidities or other acute infections as well as patients having chronic respiratory or other inflammatory diseases and patients who had received antibiotic therapy in last fifteen days were excluded from the study. Patients having any other metabolic disorder were not included in the study.
Before starting the study, approval from Institutional ethics committee was taken. When patients came first time to outpatient clinic were first examined by consulting pediatrician. If patient diagnosed as ARTI and drugs were prescribed, they were included in the study according to inclusion and exclusion criteria. Informed consent of parent/guardian of each patient was taken before collecting the data. Drugs along with dosage, route of administration and duration of treatment from the prescription of patients were noted down in data record form. Other sociodemographic data such as age, sex weight of the patients and chief complains were also noted. The data obtained were subjected to statistical analysis.
Statistical Analysis
All statistical analysis was done by using window based software SPSS, Version 20. Data was summarized into numbers, percentages, mean and standard deviation. Demographic variables and symptoms were assessed by applying Chi-square test.
Results
Table 1: Agewise distribution of patients.
| Age (Months) | Male | Female | Total |
| 11-20 | 52 (27.4%) | 23 (21.3%) | 75 (25.2%) |
| 21-30 | 40 (21.1%) | 23 (21.3%) | 63 (21.1%) |
| 31-40 | 21 (11.1%) | 20 (18.5%) | 41 (13.8%) |
| 41-50 | 33 (17.4%) | 20 (18.5%) | 53 (17.8%) |
| 51-60 | 44 (23.2%) | 22 (20.4%) | 66 (22.1%) |
| Total | 190 (100%) | 108 (100%) | 298 (100%) |
Chi square = 4.093 p = 0.394
The agewise distribution of patients is given in the table (Table 1). Maximum, i.e. 75 patients presented were between 11-20 months of age which was 25.2%. There was gradual decrease in number of patients but again it was found to be increased between age group 51-60 months and it was 66 i.e. 22.1%.
Table 2: Age of Male and Female children (in months) included in the study.
| Sex | Number | Mean (Months) | Std. Deviation |
| Male | 190 | 35.0 | 16.8 |
| Female | 108 | 36.3 | 15.5 |
| Total | 298 | ||
t = 0.675 , p = 0.500
Mean age of male children was 35 months with standard deviation 16.8 and female in children it was 36.3 months with standard deviation 15.5.
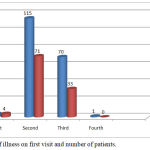 |
Graph 1: Day of illness on first visit and number of patients.
|
Only 8 patients came on first day. On second and third day, 186 (62.4%) and 103 (34.6%) patients came respectively, while on forth day only one patient consulted.
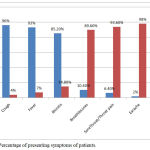 |
Graph 2: Percentage of presenting symptoms of patients.
|
In our study, maximum patients presented with cough as a common presenting symptom. Total 286 (96%) patients were having cough as common presenting symptom. Next common symptoms noted were fever in 277 (93%) and rhinitis in 254 (85.2%). Pain in the throat (sore throat) was present in 31 (10.4%) and breathlessness was in 19 patients (6.4%). Earache was observed in only 6 (2%) patients.
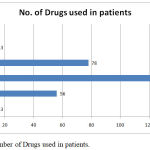 |
Graph 3: Number of Drugs used in patients.
|
Number of drugs used range from 2-7. Maximum i.e. 133 patients received four drugs. Minimum 2 drugs were received by only 13 patients and maximum 7 drugs were received by 5 patients.
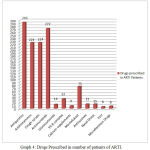 |
Graph 4: Drugs Prescribed in number of patients of ARTI.
|
Most commonly used drugs were Antipyretics in 293, Antimicrobials were prescribed in 272, Antihistaminics and bronchodilators were in 224 patients each. Montelukast (leucotrine antagonist) was prescribed in 75 while antitussives in 15 patients and Glucocorticoids were used in 14 patients. Vitamin B complex and iron supplements were prescribed in 33 and 6 patients respectively. Nasal drops and other miscellaneous drugs prescribed in remaining 33 patients.
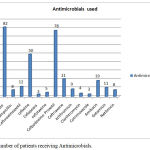 |
Graph 5: Number of patients receiving Antimicrobials.
|
Amoxicillin+clavulanic acid was prescribed in 82 patients. Cephalosporins like Cefuroxime axetil, Cefixime, Cefoperazone, Cefotaxime, Cefpodoxime proxetil, Cefriaxone were prescribed in 169 patients, Macrolides like Azithromycin and clarithromycin were prescribed 13 patients, Aminoglycosides like Amikacin, Gentamicin and Netilmicin were prescribed in 38 patients and Cotrimoxazole were prescribed in 3 patients.
Table 3: Details of prescribing indicators.
| Sr. No. | Parameters | Number |
| 1 | Total number of prescriptions analysed | 298 |
| 2 | Total number of drugs prescribed | 1229 |
| 3 | Total number of prescriptions without drugs | 0 |
| 4 | Total number of prescriptions without antibiotics | 26 |
| 5 | Average number of drugs per prescription | 4.1 |
| 6 | Total number of prescriptions containing antibiotics | 272 |
| 7 | Total number of antibiotics prescribed | 313 |
| 8 | Average number of antibiotics per prescription | 1.05 |
| 9 | Percentage of medicine prescribed by generic name | 0 |
| 10 | Percentage of drugs prescribed by intravenous route | 24.83% |
| 11 | Percentage of prescriptions with cough& cold preparations | 75.16% |
| 12 | Percentage of prescriptions with antihistaminic preparations | 75.16% |
| 13 | Percentage of prescriptions with antibiotics are prescribed | 91.27% |
| 14 | Percentage of prescriptions without medications | 0.00% |
| 15 | Percentage of drug prescribed from NLEM | 97.32% |
NLEM – National List of Essential Medicine
Discussion
Studies of drug utilization pattern of different diseases have become very important tool to evaluate health care system. It will throw a light on different aspects of prescribing pattern in the particular area in specific period, and will help to analyze it. Such studies will also help to implement different ways to improve prescribing trends.
The study period of present study was from August 2014 to August 2017. The study was conducted in pediatric department of Krishna hospital and research centre, Karad. Total 298 prescriptions were evaluated of children between 1-5 years of age suffering from acute respiratory tract infections. Out of 298 patients 190 (63.75%) were male and 108 (36.25%) were female children. Though number of male children was high, statistically there is no difference. A similar study by S. Ganesh Kumar et al also reported higher number of boys than girls in their study.7
Out of the total number of patients in the study, the maximum patients were from age group 11-20 months i.e. 25.2 %. This suggests that respiratory tract infections are more common in these age groups. Our observation coincides with observation of Alkahtani et al. They also noted maximum number of respiratory tract infection from same age group.8 The patient number started decreasing gradually. It was least between 31-40 months age group 41(13.8%). However, this percentage again increased after 51 months and it became 22.1%. This may be due to increased exposure to public places or contact with other children in preschool group (Table 1). Mean age of male children in the study was 35 months and that of female children was 36.3 months (Table 2) which is statistically similar.
We also noted the day of illness on presentation (Graph 1). Patients presented to clinic from second to fourth day from onset of symptoms. Only 8 patients came on first day. Maximum patients came on the second (n=186) and third day (n=103). There was no statistical difference between male and female patients who visited clinic on second or third day. Thus there was no gender disparity for seeking the treatment.
In our study, presenting symptoms and signs observed in patients coming first time to outpatient clinic were cough, rhinitis, fever, breathlessness, earache and sore throat/throat pain. (Graph 2) Common symptoms of presentation found in our study were cough in 96% patients, fever in 93% patients and rhinitis in 85.2% patients. Other symptoms observed were throat pain (sore throat) in 10.4%, breathlessness in 6.4% and earache in 2% patients. Most of the patients presented with three or four symptoms from above. Maximum i.e.224 patients were having cough, fever and rhinitis as chief complains. In our study we found cough as the most common symptom. Our observation coincides with observation of MF Cotton et.al. In their study cough and rhinitis were the most common symptoms noted and they found fever in only 15 % cases, on the day of presenting to clinic. 9 In our study fever was present in 93% patients, Abbasali Javadi et.al also found fever as the most common symptom in children.10 Sore throat, coryza and cough are other common symptoms noted by them. The reason given by them is, in younger children rhinovirus is the most common causative agent for ARTI, so fever may be the commonest symptom of presentation. Marie- louise von Listow et al11 found nasal discharge (rhinitis) was the most common symptom in children below one year of age. We found sore throat / pain in throat in 31 (10.4%) patients. In under 5 children, 70 % sore throat are caused by viruses.
In our study we found that drugs received by patients ranges from 2-7, i.e on an average minimum 2 and maximum 7 drugs were received by the patients (Graph 3). Average number of drugs prescribed was 4.1 drugs per patient. In other similar type of studies, average number of drugs prescribed are 2.24, 2.81 and 3.4 per patient,12,13,14, thus they were less than our study. But Mirza Beg et al found it as 8.32 drugs per prescription.15 This was quite higher than our study; the reason for this may be that they included acute as well as chronic respiratory diseases. Study conducted by Sunil Karande et al found average number of drugs used was 2.9 per patient.16 Shruthi et. al. found it was 6.9 drugs per prescription where she included only LRTI in age group 1 month to 14 years.17 Average numbers of drugs prescribed per patient were high in our study as compared to other studies. We included children from age group one to five years. In this age group severity of disease is more. Because of more number of symptoms child remain irritable, therefore parents demand for quick symptomatic relief, so more drugs must have been prescribed.
The Most common drugs used were from antipyretic group (Graph 4). Out of 298 patients, 293 i.e. 98.3% of them received at least one antipyretic. In the study by Alkahtani et al, antipyretics and analgesics were the most commonly used drugs followed by antihistaminics and decongestants.8 Anti histaminics and combination of mucolytics, expectorants + bronchodilators were also prescribed in 224 patients i.e. 75.2%. In study conducted by Biswadeep et al, antihistaminics were used in 41.8% patients.18 Antihistaminics were prescribed for symptomatic relief but there is no evidence that they will shorten the course of the disease. Though cough was the most common symptom of presentation antitussives were prescribed in only 15 patients that means very few patients were having dry cough and most of the patients were having productive cough. Monteleukast, a leukotriene antagonist, was used in 75 patients, i.e. 25.2%; recently the trend of using this is increased, so in previous studies use of this was not observed. Nasal drops having nasal saline or nasal decongestant were also prescribed in 15 (5%) patients and they also give symptomatic relief. In study by Alkahtani, use of nasal decongestants was in 5.6% patients. Our observation is similar to him. In the study by Biswadeep et al, these nasal preparations were used in 21% patients; this number is higher as compared to our study.18 Glucocorticoids were used in only 14 patients. In a study by Mirza Beg et al, out of total drugs prescribed, 90% drugs were glucocorticoids. They included patients of all age groups having respiratory tract infections.15 Other drugs prescribed were calcium in 9 patients and vitamin B complex in 33 patients. Iron supplements were prescribed only in 6 patients, Vitamin supplements; calcium supplements as well as iron preparations were also used in few patients. Since viral infection also causes generalized weakness and reduce appetite, these drugs must have been prescribed. In one survey based study of drugs used in respiratory tract infections, it was noted that multivitamins were prescribed in quite a large number of patients. Reason for this was stated that concurrent antibiotic prescription can disturb intestinal bacterial flora and may lead to vitamin B complex deficiency; to prevent that vitamins were prescribed. 19
Most of the ARTIs were viral origin, but the percentage of antimicrobial (AMA) prescription observed in our study was quite high, it was almost 91%. In a study by Alkahtani et al, antibiotic prescription was 72.7% in upper respiratory tract infections.8 In the study conducted by Naseer et al, 62.6% children of less than five received antibiotics for acute respiratory tract illness.20 According to their study, rate of antibiotic consumption was more in urban area than in rural area. Most of the antibiotics used in this study were given by oral route. On the basis of our observations we can say that the clinicians first want to focus on the treatment of infection and symptomatic treatment, while other drugs used were less. But overall antibiotic prescription rate is high for a respiratory tract infection irrespective of it was bacterial or viral.
In our study, amoxycillin + clavulanic acid was the most commonly used antimicrobial (Graph 5). It was used in 82 patients i.e. 27.5%. In a study conducted by Biswadeep Das et al, it was found that amoxycillin + clavulanic acid was the most commonly used antimicrobial.18 They conducted study on age group between 0-12 years. But most of the children in their study were between 2-5 years. Even in the study by Mirza A Beg et al, amoxycillin + clavulanic acid was the most commonly used AMA. Amongst cephalosporins, Cefpodoxime proxetil was used in 26.2%, cefixime in 16.8% and Cefuroxime axetil was used in 4% patients. From the above observations, we can infer that different cephalosporins were preferred antimicrobials. Azithromycin and Clarithromycin were used in 9 and 4 patients respectively. According to study by Pramil et al, azithromycin was most commonly used for respiratory tract infections in children, but in our study azithromycin was used in a less number of patients. Cotrimoxazole was used only in 3 patients. Commonly used antimicrobials by IV route were amikacin and ceftrixone. In 19 patients, amikacin and ceftriaxone were used simultaneously.
Thus in our study we observed that beta lactam antimicrobials were the choice of antimicrobial for respiratory tract infections in children. The treatment pattern of ARTI in the hospital shows the high prevalence of antibiotic prescribing. Training and education of doctors and other health care professionals is needed for rational drug utilization and to ensure appropriate therapy.
97.32% drugs were prescribed from National List of Essential Medicine (NLEM). All drugs were prescribed by brand names and not a single drug was prescribed by generic name (Table 3). In study of Pal et.al. Prescription from essential list was 67.60% and in study by Bikash Gairola it was only 22.67%.21,22 In both of these studies percentage of prescription from NLEM was very less as compared to our study. In above two studies percentage of drugs by generic name was 0.56% and 34.62% respectively whereas it was 0% in our study. There is a scope for improvement in prescribing drugs by generic name. However since 2016 prescription of drugs by generic name made compulsory and our study period is from August 2014 to August 2017 so prescription by generic name must not have followed.
Conclusion
It was observed that prescription from NLEM was good, suggesting rational approach in giving the treatment, but prescription by generic name was not there which needs the improvement.
Overuse of antimicrobials was observed. In ARTI, use of antibiotic is always an area of concern. The misuse of antibiotics, especially in children can lead to bacterial resistance as well as various undesirable side effects associated with its use. As there was no immediate availability of culture and sensitivity report for outpatient setting, there is always dilemma for prescribing an antibiotic. There is a need of educational programmes in order to bring rational use of antibiotics that requires development of standard guidelines for antibiotic prescription. It is also needed to create awareness in parents regarding the risk-benefit of antibiotics or other drugs for the self-limiting condition. The present investigations are regularly needed to study the drug prescribing practices so that appropriate criticism and awareness will be generated. The findings from this study highlight the important aspects to optimize the rationale use of drugs for ARTIs in under five children and can help to establish the prescribing guidelines.
References
- Wardlaw T. M., Johansson E. W., Hodge M. J. Pneumonia the forgotten killer of children. New York: The United Nations Children’s Fund (UNICEF) / World Health Organization (WHO). 2006.
- Karen C., Larryr. Microbiology and Laboratory diagnosis of upper respiratory tract infections. Clin Infect. Dis. 1996;23:442-448.
- Simoes A. F. E.,Cherian T., Chow J., Shahid-Salles A. S., Laxminarayan R and John J. T. Acute Respiratory Infections in Children. Disease Control Priorities in Developing Countries. 2nd edition Chapter 25.
- Jamison T. D., Breman G. J.,Measham R. A., Alleyne G., Claeson M., Evans B. D., Jha P.,Mills A., Musgrove P (eds). Disease Control Priorities in Developing Countries, 2nd ed. Washington (DC): The International Bank for Reconstruction and Development The World Bank. 2006;8:483-498. Epidemiology of communicable diseases. Park K (ed). Park’s Textbook Of Preventive And Social Medicine , 21st ed. Jabalpur: Banarsidas Bhanot Publishers. 2011.
- Chourjit K., Gupte S. Pediatric viral infections. Gupte S (ed). The Short Textbook of Pediatrics, 11 ed. New Delhi: Jaypee. 2009;247-269.
- World Health Organization, Acute respiratory tract infections in children, Family and Community Health cluster (FCH). 2011.
- Kumar S. G., Majumdar A., Kumar V., Naik B. N., Selvaraj K., Balajee K. Prevalence of acute respiratory infection among under-five children in urban and rural areas of puducherry, India. Journal of Natural Science, Biology and Medicine. 2015;6(1):3-6.
CrossRef - Alkahtani A. S. Drug utilization pattern of upper respiratory tract infections in pediatric at Najran university hospital, KSA. Biomedical Research. 2017;28(20):8981-86.
- Cotton M. F., Innes S., Jaspan H.,Madide A., Rabie H. Management of upper respiratory tract infections in children. South African Family Practice. 2008;50(2):6-12.
CrossRef - Javadi A., Adibi P.,Ataei B., Nokhodian Z.,Yaran M. Surveillance of acute respiratory infections among outpatients: A pilot study in Isfahan city.Journal of Research in Medical Sciences. 2015;20(2):115–21.
- Von Linstow M. L., Holst K. K., Larsen K., Koch A., Andersen P. K., Hogh B. Acute respiratory symptoms and general illness during the first year of life: A population‐based birth cohort study.Pediatric Pulmonology. 2008;43(6):584-93.
CrossRef - Joshi U., Hishikar R., Agrawal S., Halwai A., Kirtania L.,Kurrey K. Study of drug use in outdoor pediatric patients of upper respiratory tract infections in a tertiary care hospital. International Journal of Basic & Clinical Pharmacology. 2015;4(5):1009-12.
CrossRef - Das B., Sarkar C., Majumder A. G. Medication use for pediatric upper respiratory tract infections.Fundamental & Clinical Pharmacology. 2006;20(4):385-90.
CrossRef - Pramil T., Rajiv A., Gaurav G. Prescription practice in patients of upper respiratory tract infection at a pediatric outpatient clinic in Punjab.Indian Journal of Pharmacy Practice. 2014;7(2):26-32.
CrossRef - Beg A. M., Dutta B. S.,Bawa S., Kaur A.,Vishal S., Kumar U. Prescribing trends in respiratory tract infections in a tertiary care teaching hospital. International Journal of Research in Medical Sciences. 2017;5(6):2588-91.
- Karande S., Sankhe P., Kulkarni M. Patterns of Prescription and Drug Dispensing . Indian Journal of Pediatrics. 2005;72(2):117-21.
CrossRef - Shruthi K. V., Dr. Bhandare B and Dr. Adarsh E. prescribing pattern of drugs in paediatric in-patients with lower respiratory tract infection at a tertiary care hospital. world journal of pharmacy and pharmaceutical sciences. 2396-2409;5(4).
- Das B., Sarkar C.,Majumder G. A. Medication use for pediatric upper respiratory tract infections. Fundamental and Clinical Pharmacology. 2006;20(4):385-90.
CrossRef - Bhasin S. M., Budden E. H., Ketkar A. R., Pawar A. P. Current trends in the treatment of upper respiratory tract infections in neonates, infants and children: A Survey. Indian Journal of Pharmacology. 2002;34:62-63.
- Mostafavi N.,Rashidian A., Karimi-Shahanjarini A.,Khosravi A and Kelishadi R. The rate of antibiotic utilization in Iranian under 5-year-old children with acute respiratory tract illness: A nationwide community-based study. Journal of Research Medical Sciences. 2015;20(5):429–433.
- Pal P., Bhattacharyya D., Kokila B. N., Herle M., Ghosh A., Sen S. Drug utilization pattern in out-patients with respiratory tract infections in a rural teaching hospital: a prospective observational study. International Journal of Basic & Clinical Pharmacology. 2017;6(12):2894–99.
- Gairola B., Devarsi C., Daisy P., Anupama D. Drug Prescribing Pattern in Respiratory Tract Infection in Children Aged 1 to 12 Years at Outpatient Department at Silchar Medical College and Hospital, Assam. India J Pharm Biomed Sci. 6(10):537–545.







