Manuscript accepted on :06-Dec-2018
Published online on: 17-12-2018
Plagiarism Check: Yes
Reviewed by: Luis Gómez
Second Review by: Mohamed Elsheikh
Kadek Budi Santosa , Pande Made Wisnu Tirtayasa
, Pande Made Wisnu Tirtayasa and Anak Agung Gde Oka
and Anak Agung Gde Oka
Urology, Department of Surgery, Faculty of Medicine UniversitasUdayana /Sanglah General Hospital, Bali, Indonesia.
Corresponding Author E-mail: wisnu.tirtayasa@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1597
Abstract
Female urethral stricture is uncommon and difficult to diagnose. Currently, only a small amount of literature has reported the successful treatment of female urethral stricture using a reconstruction approach. In this study we describe our results with the management of female urethral stricture using a dorsal vaginal graft. Four patients were diagnosed with female urethral stricture and were treated with urethral reconstruction using a dorsal vaginal graft. Primary urethroplasty using dorsal vaginal graft can be considered as a first-line option in the management of female urethral stricture, especially in centers with experience in graft-based reconstruction.
Keywords
Female; Graft; Reconstruction; Urethral Stricture; Urethroplasty
Download this article as:| Copy the following to cite this article: Santosa K. B, Tirtayasa P. M. W, Oka A. A. G. Dorsal Vaginal Graft Urethroplasty as a Treatment for Female Urethral Stricture: Case Reports of Four Patients. Biomed Pharmacol J 2018;11(4). |
| Copy the following to cite this URL: Santosa K. B, Tirtayasa P. M. W, Oka A. A. G. Dorsal Vaginal Graft Urethroplasty as a Treatment for Female Urethral Stricture: Case Reports of Four Patients. Biomed Pharmacol J 2018;11(4). Available from: http://biomedpharmajournal.org/?p=24811 |
Introduction
A female urethral stricture is difficult to diagnose due to the low incidence and presenting symptoms, such as frequency, dysuria, urgency, hesitancy, retention and recurrent urinary tract infections. The rarity of occurrence and the difficulty to make a diagnosis make the management of female urethral strictures quite challenging.
The treatment options include observation, urethral dilation, self-catheterization, urethrotomy, and reconstruction depending on the severity and location of the stricture. Urethral dilation is usually the first line treatment albeit no specific treatment algorithm exists. Urethral dilation has been shown to have a failure rate as high as 94% recurrence rate at a mean follow-up of 2 years.1 Some studies showed urethral reconstruction has a better outcome.Several techniquesfor the management of female urethral stricture have been described in the literature.
In this study, we describe our results on themanagement of female urethral stricture using a dorsal vaginal graft as previously described.2 We assessed improvements in symptoms and the patency of urethral lumen post-operatively.
Presentation of Cases
A total of 4 patients with lower urinary tract symptoms were diagnosed with female urethral stricture at our institution (Table 1). All patients were treated with urethral reconstruction using a dorsal vaginal graft. All of the patients had undergone urethral dilation previously with two of them having had internal urethrotomy besides urethral dilation treatment.
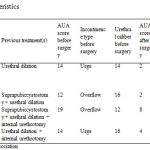 |
Table 1: Patient Characteristics |
All of the patients complained of frequency, urgency, straining and decreased flow during voiding. We investigated the patients’ history, and did a subjective assessment using AUAsymptom score, physical examination, urinalysis, urine cultures, and ultrasonography. All the patients had not undergone uroflowmetry and urodynamic examinations due to limitations in equipment at our institution. During surgery, urethrocystoscopywas performed with the patient under general or spinal anesthesia using a 7 F ureterorenoscope to assess the location of the stricture as well as bladder wall conditions and competence of bladder neck by observing its ability to open and its involvement in the fibrotic process. A biopsy was taken from the stricture area in all patients to exclude malignancy. Urethral calibration was done following urethrocystoscopy using urethral sound to assess the urethral diameter.
A total of 4 patients with an age range from 26 to 66 years were followed up for 3 months postoperatively. Two patients presented with urge incontinence, while the other two patients presented with overflow incontinence which had been treated provisionally with a suprapubic catheter. All of the patients had undergone urethral dilation repeatedly. Moreover, two patients had internal urethrotomy as the next treatment after urethral dilation. Two of the 4 women had a preoperative urethral calibration of 16 Fr. The remaining patients calibrated to 14 Fr and 12 Fr. Three of our cases (75%) of urethral strictures were due to E.Coli bacterial urethritis, while one case was due to excision of urethral hemangioma.
The successful anatomical repair was achieved in all our patients while all incontinence was resolved in 3 patients (75%). One patient had urge incontinence post-operatively where she had overflow incontinence pre-operatively. The mean AUA score had decreased from 14.75 to 4 post-operatively. We did urethral calibration 1 month after surgery to all patients to make sure of urethral patency. Three months following surgery, all of the patients stated that they were satisfied with the procedure, even the patient who presented an urge incontinence post-operatively. She was satisfied because she was free from the suprapubic catheter and she also felt that the incontinence symptom was getting better with the medication.
Description Of Operative Technique
The patient is prepared in lithotomy position under general or spinal anesthesia. The antiseptic procedure is performed on the vagina and around the vagina. Urethrocystoscopy and urethral calibration are done as described previously. A 14 F urethral catheter is introduced into the urethra, and the balloon is inflated inside the bladder. The anterior vaginal wall is assessed and a free graft of vaginal epithelium is harvested (Figure 1). The graft is dissected from vaginal tissue using a no.11blade with the injection of epinephrine mixture before dissection.
 |
Figure 1: Free graft of vaginal epithelium is harvested.
|
The harvest site is assessed,hemostasisis performed and closed with interrupted 2.0 absorbable sutures. The vaginal graft is stored in a normal saline-damp gauze for later use. Asuprameatal incision is made (Figure 2), and a plane is developed through the dorsal membrane to the urethral meatus. Dissection is performed towards the pubic bone without violation of the urethra. The pubic bone may be identified using palpation to assess the appropriate border of the proximal dissection point. The dissection is continued until the proximal point of the stricture.
 |
Figure 2: A suprameatal incision is made.
|
After the dissection is completed, the incision site on the urethra is identified at the 12 o’clock position. The incision is made at the 12 o’clock position withscissors, and this should be carried out until the proximal point of the stricture (Figure 3). The urethral catheter is removed, and the proximal urethra is calibrated with a 30 F metal sound to assess the normal urethral patency. The mucosal surface of the graft is sutured facing the urethral lumen using 4.0 vicrylsutures. Moreover, two sutures are placed in the center of the graft to minimise sliding and prevent graft migration (Figure 4). A 30 F metal sound is passed through the urethra to ensure the desired urethral diameter. A 20 F silicon catheter is inserted, and the balloon is inflated inside the bladder. An overnight vaginal pack is leftin place. The catheter is left in place for 2 weeks.
 |
Figure 3: The incision on the urethra is made at the 12 o’clock position.
|
 |
Figure 4: The graft’s mucosal surface is sutured facing the urethral lumen.
|
Discussion
A standardized management algorithm for female urethral strictures is lacking due to the rarity of the disease. The exact number of female urethral strictures is unknown with only less than 100 cases having been reported in the literature.3 Because of this issue, urethral dilation and internal urethrotomyare done to patients as a first-line treatment (4-6). However, the recurrence rate of this treatment is high and can exacerbate periurethral scarring and fibrosis, leading to a further complicated stricture.3,7,8 All the patients in this study had previously undergone unsuccessful dilation and internal urethrotomy.
We present our management of female urethral strictures using dorsal vaginal graft urethroplasty as initially described by Tsivian and Sidi.2 The patients who underwent this treatment were women who presented with a history of either combination of urethral dilation and internal urethrotomy or urethral dilation alone. Moreover, half of them presented with a suprapubic catheter due to overflow incontinence as a complication of urethral stricture.
Total urethral replacement with various tissues has been used for constructing a new urethra in severe urethral stricture using flap8-11 and graft2,12 based on urethroplasty techniques with efficacious and safe results. In line with previous reports, we use a suprameatal approach because of the ease of incision for urethrolysis and to make access for future anti-incontinence procedures less problematic.12,13 This approach also has the advantages of strong mechanical support for the graft provided by the well-vascularized clitoral cavernosal tissue, minimizing the risk of sacculation and facilitating a more physiologic reconstruction which directs the urinary stream away from the vagina.7,8 Another benefit includes the minimal risk of urethrovaginal fistula.12,14
The use of vaginal epithelium for the graft was inspired by the description of the technique by Tsivian and Sidi(2), and also the surgeon’s familiarity with dissection in harvesting vaginal hairless elastic mucosal grafts.
This study has similar limitations to the small number of previous studies regarding this issue. A female urethral stricture is a rareoccurrence and designing randomized controlled studies with long-term follow-up is extremely difficult. However, the success of the case management in the current study is quite similar to other approaches, even though our data is based on only a few patients and relatively short term. All of our patients did not need to perform daily clean intermittent catheterization as part of their treatment plan.
Conclusions
Female urethral strictures are a rare disease. The use of urethral dilation and internal urethrotomy as a primary treatment will mostly fail due to increased periurethral fibrosis. Primary urethroplasty using a dorsal vaginal graft can be considered as a first-line option in the management of female urethral stricture, especially in centers with experience in graft-based reconstruction.
Conflict of Interest
There is no conflict of interest.
References
- Blaivas J. G., Santos J. A., Tsui J. F., Deibert C. M., Rutman M. P., Purohit R. S., et al. Management of urethral stricture in women. Journal of Urology. 2012;188(5):1778-82.
CrossRef - Tsivian A., Sidi A. A. Dorsal Graft Urethroplasty for Female Urethral Stricture. Journal of Urology. 2006;176(2):611-3.
CrossRef - Schwender C. E. B., Ng L., McGuire E., Gormley E. A. Technique and results of urethroplasty for female stricture disease. Journal of Urology. 2006;175(3):976-80.
CrossRef - Keegan K. A., Nanigian D. K., Stone A. R. Female urethral stricture disease. Current Urology Reports. 2008;9(5):419-23.
CrossRef - Santucci R. A., Payne C. K., Saigal C. S. Office Dilation of the Female Urethra: A Quality of Care Problem in the Field of Urology. Journal of Urology. 2008;180(5):2068-75.
CrossRef - Smith A. L., Ferlise V. J., Rovner E. S. Female urethral strictures Successful management with long-term clean intermittent catheterization after urethral dilatation. BJU International. 2006;98(1):96-9.
CrossRef - Sharma G. K., Pandey A., Bansal H., Swain S., Das S. K., Trivedi S., et al. Dorsal onlay lingual mucosal graft urethroplasty for urethral strictures in women. BJU International. 2010;105(9):1309-12.
CrossRef - Migliari R., Leone P., Berdondini E., De Angelis M., Barbagli G., Palminteri E. Dorsal Buccal Mucosa Graft Urethroplasty for Female Urethral Strictures. Journal of Urology. 2006;176(4):1473-6.
CrossRef - Blaivas J. G., Heritz D. M. Vaginal flap reconstruction of the urethra and vesical neck in women: A report of 49 cases. Journal of Urology. 1996;155(3):1014-7.
CrossRef - Tanello M., Frego E., Simeone C., Cosciani Cunico S. Use of pedicle flap from the labia minora for the repair of female urethral strictures. Urologia Internationalis. 2002;69(2):95-8.
CrossRef - Wadie B. S., ElHifnawy A., Khair A. A. Reconstruction of the Female Urethra: Versatility, Complexity and Aptness. Journal of Urology. 2007;177(6):2205-10.
CrossRef - Petrou S. P., Rogers A. E., Parker A. S., Green K. M., McRoberts J. W. Dorsal vaginal graft urethroplasty for female urethral stricture disease. BJU International. 2012;110(11):E1090-E5.
CrossRef - Petrou S. P., Brown J. A., Blaivas J. G. Suprameatal transvaginal urethrolysis. Journal of Urology. 1999;161(4):1268-71.
CrossRef - Önol F. F., Antar B., Köse O., Erdem M. R., Önol Ş. Y. Techniques and results of urethroplasty for female urethral strictures: Our experience with 17 patients. Urology. 2011;77(6):1318-24.
CrossRef







