Parithimar Kalaignan and Jaya Shree Mohan
and Jaya Shree Mohan
Department of Prosthodontics, Vinayaka missions Sankarachariyar dental college, Salem.
Corresponding Author E-mail: parithisiva@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1506
Abstract
Cancers of the orofacial region can be devastating in their impact on physical structure and function of the affected individual, leading to potentially severe compromises in quality of life. A total of Twenty (20) mandibular resected patients were selected for this study. All the patients’ were rehabilitated with mandibular resection prosthesis. Novel scale known as Maxillofacial Prosthesis Performance Scale (MFPPS) was developed for mandibulectomy patients to assess the oral health related quality of life. This scale has been tested for validity and reliability. The OHRQol was measured using the oral health impact profile (OHIP-Edent-19), Obturator functioning scale (OFS-15) and Maxillofacial Prosthesis Performance Scale (MFPPS-10) with standardized questionnaire after 2 weeks & 3months of prosthesis function for twenty (20) mandibular resected patients. For OHIP –Edent scale; when comparing 2 weeks, all subscale scores shown significant progress on oral health impact profile-Edent scale after 3 months of prosthesis function. For OFS scale; when observing the score of 2 weeks and 3 months, there was dramatic improvement of (75%) in miscellaneous factors which include Problems in dryness of mouth, engagement in social events and obturator positioning. For MFPPS; all rehabilitated patients’ were observed two weeks later, negative impacts have been eliminated and positive impacts increased on oral health. The patient was reviewed again 3months later and confirming an even higher level of overall satisfaction with the Mandibular Resection Prosthesis. The maxillofacial prosthesis had a strong positive impact on quality of life .Hence mandibular resection prosthesis enhance the oral health related quality of life.
Keywords
Mandibular Resection Prosthesis; Maxillofacial Prosthesis Performance Scale; Obturator Functioning Scale; Oral Health Impact Profile–Edent
Download this article as:| Copy the following to cite this article: Kalaignan P, Mohan J. S. Oral Health Related Quality of Life with Mandibular Resection Prosthesis. Biomed Pharmacol J 2018;11(3). |
| Copy the following to cite this URL: Kalaignan P, Mohan J. S. Oral Health Related Quality of Life with Mandibular Resection Prosthesis. Biomed Pharmacol J 2018;11(3). Available from: http://biomedpharmajournal.org/?p=22158 |
Introduction
The patient with maxillofacial defects who has been partial or completely resected mandible is one of the most challenging tasks in maxillofacial rehabilitation.1,2 In discontinuity mandibular defects primarily affects mandibular movements, function, swallowing and speech. Loss of mandibular continuity leads to deviation of mandible towards resected side because of absent musculature and cicatricial changes in the surgical site.3,4 The severity and stability of mandibular deviation is highly unpredictable is dependent upon many factors such as extent and location of the resection, the amount of soft tissue and muscles involvement and the presence of remaining teeth.
Brown’s classification proposal (panel) is based on the principle that the mandible has four corners: two vertical corners that make the angles of the mandible, and two horizontal corners that are centred at the canine teeth on each side in the dentate mandible, and are roughly 7 mm anterior from the mental foramen in the edentulous jaw. The anterior or horizontal corners are essential to maintain function and aesthetics.5,6
Class I : Lateral mandibulectomy (includes the angle or one vertical corner but not the condyle),
Class I c: Lateral mandibulectomy and condyle.
Class II : Hemimandibulectomy (includes the angle [vertical corner] and the ipsilateral canine [horizontal corner], but not the contralateral canine),
Class II c: Hemimandibulectomy and condyle,
Class III : Anterior mandibulectomy (includes both canines [two horizontal corners] but neither angle),
Class IV: Extensive mandibulectomy (includes both canines and one or both angles [three to four corners])
Class IV c : Extensive mandibulectomy and condyles (extensive anterior mandibulectomy, including both canines and one or both condyles).
The use of the corners of the mandible at the angles and the canine regions make this classification system a logical approach to classify defects, increasing in size and complexity from class I (a simple lateral defect not including the condyle involving the angle or vertical corner) to class IV (which involves at least three corners) and class IVc (which includes total mandibulectomy). The proposed classification system represents the increase in morbidity in aspects of aesthetics and function from class I to class IV.
The present study investigated the oral health related quality of life of patients with maxillofacial defects after prosthodontic therapy with mandibular resection prosthesis. However, only a few studies have evaluated the change in quality of life in mandibulectomy patients after rehabilitation.7,8
Even though the numerous scales currently exist to measures the oral health related quality of life, no single scale / instrument is more precise / specific for maxillofacial defects.
Hence, this study was planned to establish a novel scale and the assessment of oral health related quality of life (OHRQol) in mandibulectomy patients rehabilitated with mandibular resection prostheses.
Materials and Methods
A total of Twenty (20) mandibular resected patients were selected for this study. Thorough clinical and radiological examinations were done .The patient explained about prosthodontics procedures and informed consent was obtained. Maxillary and mandibular preliminary impressions were made with irreversible hydrocolloid (Alginate). Impressions were poured with type III dental stone. Diagnostic cast was surveyed and tripoded for mandibular resected prosthesis frame work design .Mouth preparation was done based on the planned framework design. Polyvinyl siloxane putty –wash impression was made to fabricate a master cast. Master cast was duplicated with phosphate bonded investment material to fabricate a refractory cast. Frame work pattern was designed with cast partial denture wax on refractory cast. A final framework was casted with base metal alloys then trimmed and polished. Metal framework try in was performed to check the prosthesis stability. Maxillomandibular records were made by manually assisting the mandible into Maximum Intercuspal Position (MI). Teeth arrangement was done then; final mandibular resection prosthesis was fabricated and inserted. The design which includes guide flange on buccal portion and the supporting appliance on lingual portion .Accessory retention were provided by interdental clasps on posterior teeth. Post maintenance instructions were given and recalled visits were scheduled on periodic basis.
Data Collection
Novel scale known as Maxillofacial Prosthesis Performance Scale (MFPPS) was developed for mandibulectomy patients to assess the oral health related quality of life. This scale has been tested for validity and reliability.
The OHRQol was measured using the oral health impact profile (OHIP-Edent-19), Obturator functioning scale9,10 (OFS-15) and Maxillofacial Prosthesis Performance Scale (MFPPS-10) with standardized questionnaire after 2 weeks & 3months of prosthesis function for twenty (20) mandibular resected patients.
Patients were asked serious of questions by using all three scales. Answers were recorded by a single operator.
Results and Observation
For Oral Health Impact Profile –Edent-19 Scale
The mean oral health impact profile (OHIP-EDENT-19) score of twenty (20) mandibular rehabilitated patients’ shows 4.7 & 3.9 through 2 weeks and 3 months of prosthesis function respectively.
The average percentage score for OHIP-Edent subscales: functional limitation (37%), physical pain (371%), psychological discomfort (41%), physical disability (38%), psychological disability (27%), social disability (30%) and handicap (38%).
Table 1: Total OHIP Score of twenty patients from all domains.
| Total OHIP Score (Sum of Scores from all domains) |
||
| OHIP Score (After 2 weeks) | OHIP Score (After 3 months) | %Decrease |
| 32 | 28 | 13% |
| 47 | 36 | 23% |
| 51 | 46 | 10% |
| 43 | 35 | 19% |
| 47 | 36 | 23% |
| 25 | 22 | 12% |
| 49 | 42 | 14% |
| 33 | 28 | 15% |
| 20 | 20 | 0% |
| 23 | 20 | 13% |
| 21 | 19 | 10% |
| 34 | 26 | 24% |
| 29 | 22 | 24% |
| 28 | 22 | 21% |
| 29 | 21 | 28% |
| 32 | 27 | 16% |
| 24 | 21 | 13% |
| 42 | 35 | 17% |
| 23 | 19 | 17% |
| 27 | 22 | 19% |
| Decrease in OHIP Score is Significant | ||
 |
Figure 1: Comparison of OHIP Score between 2 weeks and 3 months of Prosthesis.
|
The most prevalent impact on OHRQOL by psychological discomfort (41%) stated that more than half percentage of patients upset with dental problems and self-conscious about the prosthesis even after the 2 weeks of prosthesis function.
Despite the discomfort in psychological subscale, there was significant improvement in functional limitation, physical pain, psychological disability and social disabilities after 2 weeks of prosthesis.
When comparing 2 weeks, all subscale scores shown significant progress on oral health impact profile-Edent scale after 3 months of prosthesis function.
For Obturator Functioning Scale (OFS-15)
The mean obturator functioning scale (OFS) score of twenty (20) mandibular rehabilitated patients’ shows 6.2 & 5.4 through 2 weeks and 3 months of prosthesis function respectively.
When observing the scale for 2 weeks of function, average percentage of score for chewing problems (37%),speech problems (36%),aesthetics problems (44%) and miscellaneous problems (27%) .
Similarly, average percentage of score for chewing problems (33%), speech problems (30%), aesthetics problems (34%) and miscellaneous problems (25%) after 3 months of prosthesis function.
Table 2: Total OFS Score of twenty patients from all domains.
| Total OFS Score (Sum of Scores from all domains) |
||
| OFS Score (After 2 weeks) | OFS Score (After 3 months) | %Decrease |
| 24 | 23 | 4% |
| 39 | 29 | 26% |
| 38 | 34 | 11% |
| 37 | 31 | 16% |
| 33 | 25 | 24% |
| 16 | 16 | 0% |
| 36 | 32 | 11% |
| 24 | 23 | 4% |
| 16 | 15 | 6% |
| 17 | 16 | 6% |
| 20 | 15 | 25% |
| 22 | 19 | 14% |
| 20 | 18 | 10% |
| 24 | 20 | 17% |
| 20 | 18 | 10% |
| 24 | 23 | 4% |
| 18 | 17 | 6% |
| 35 | 30 | 14% |
| 16 | 15 | 6% |
| 23 | 20 | 13% |
| Decrease in OFS Score is Significant | ||
 |
Figure 2: Comparison of OFS Score between 2 weeks and 3 months of Prosthesis.
|
When observing the score of 2 weeks and 3 months, there was dramatic improvement of (75%) in miscellaneous factors which include Problems in dryness of mouth, engagement in social events and obturator positioning.
All other factors shown marked improvement of 65-70% in chewing, speech and aesthetics only after 3 months of prosthesis function.
For Maxillofacial Prosthesis Performance Scale (MPPS)
The mean maxillofacial prosthesis performance scale (MPPS) score of twenty (20) mandibular rehabilitated patients’ shows 2.07& 1.66 through 2 weeks and 3 months of prosthesis function respectively. The average percentage of score for MPPS -10 shown 37 % which indicates only 63 % of patients problems were improved after 2 weeks. However, when observing 3 months, average percentage of scores were 30 % Except for problems in taste ability (37%), functional comfort (38%) and phonetics (36%), for all other dimensions where significant changes were observed, mean scores were found to be significantly increased after 2 weeks of treatment.
Table 3: Total MFPPS Score of twenty patients from all domains.
| Total MFPPS (Sum of Scores from all domains) |
||
| MFPPS (After 2 weeks) | MFPPS (After 3 months) | %Decrease |
| 21 | 16 | 24% |
| 26 | 19 | 27% |
| 30 | 25 | 17% |
| 24 | 21 | 13% |
| 27 | 20 | 26% |
| 12 | 11 | 8% |
| 28 | 22 | 21% |
| 20 | 16 | 20% |
| 12 | 11 | 8% |
| 12 | 11 | 8% |
| 11 | 10 | 9% |
| 17 | 12 | 29% |
| 16 | 12 | 25% |
| 17 | 13 | 24% |
| 16 | 11 | 31% |
| 20 | 16 | 20% |
| 13 | 12 | 8% |
| 22 | 20 | 9% |
| 12 | 10 | 17% |
| 18 | 12 | 33% |
| Decrease in MFPPS is Significant | ||
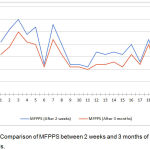 |
Figure 3: Comparison of MFPPS between 2 weeks and 3 months of Prosthesis.
|
For 3 months of treatment evaluations, minimum scores were observed for the dimensions psychological aspects 32%), aesthetics (25%), taste ability (31%) oral hygiene (27%) and general satisfaction (30%) whereas maximum scores were obtained for the item saliva co Detailed observation of the completed MPPS scale after provision of mandibular resection prostheses showed marked positive changes in the patient’s responses to the questions. Question for general satisfaction (dealing with do you have any problem with overall performance of the prosthesis?) shifted from very often to occasionally after 2 weeks and to hardly ever after 3 months.
Discussion
Prosthodontic rehabilitation of the mandibulectomy patients who is having partial or complete loss of mandibular segment poses strong impact in functional and psychological aspects.11
For mandibular resected patients, certain basic principles of complete denture fabrication steps should be modified due to many restrictive physical and psychosocial factors. In edentulous patients, a broad occlusal table developed in the palatal portion of the maxillary arch on the unaffected side will certainly support to Position the residual fragment into the correct sagittal relationship, enhance the stability of the prostheses and thus, improves masticatory performance12,13
The constructive thinking about the rehabilitation is that concentration should not be on what is missing in the eradication of disease, but rather captivating full advantage of the remaining structures.14
The average percentage score for OHIP-Edent subscales: functional limitation (37%), physical pain (371%), psychological discomfort (41%), physical disability (38%), psychological disability (27%), social disability (30%) and handicap (38%)
Despite the discomfort in psychological subscale, there was significant improvement in functional limitation, physical pain, psychological disability and social disabilities after 2 weeks of prosthesis.
When comparing 2 weeks, all subscale scores shown significant impact on oral health impact profile-Edent scale after 3 months of prosthesis function.
When observing obturator functioning scale (OFS-15) the score of 2 weeks and 3 months, there was dramatic improvement of (75%) in miscellaneous factors which include Problems in dryness of mouth, engagement in social events and obturator positioning.
All other factors shown marked improvement of 65-70% in chewing, speech and aesthetics only after 3 months of prosthesis function.
All rehabilitated patients’ were observed two weeks later and completed 10 Point MPPS scale. All negative impacts have been eliminated and positive impacts increased on oral health. The patient was reviewed again 3months later and confirming an even higher level of overall satisfaction with the Mandibular Resection Prosthesis.
References
- Hassan S.J, Weymuller E.A Jr. Assessment of quality of life in head and neck cancer patients. Head Neck. 1993;15:485-496.
CrossRef - Young C.W, Pogrel M.A, Schmidt B.L. Quality of life in patients undergoing segmental mandibular resection and staged reconstruction with no nvascularized bone grafts. J Oral Maxill of acSurg. 2007;65:706-712.
CrossRef - Jacob R.F. Prosthodontic rehabilitation of mandibulectomy patient. In: Taylor T.D, editor. Clinical Maxillofacial Prosthetics. Illinois: Quintessence Publishing Co. Inc. 2000;171–88.
- Taylor D.T. Diagnostic considerations for prosthodontics rehabilitation of the mandibulectomy patient. In: Taylor T.D, editor. Clinical Maxillofacial Prosthetics. Illinois: Quintessence Publishing Co Inc; 2000;155–70.
- Cella D.F, Cherin E.A. Quality of life during and after cancer treatment. ComprTher. 1988;14:69-75.
- Rogers S.N, Lowe D, McNally D, Brown J.S, Vaughan E.D. Health-related quality of life after maxillectomy: a comparison between prosthetic obturation and free flap. J Oral Maxill. of. acSurg. 2003;61:174-181.
CrossRef - Gift H.C, Atchison K.A, Dayton C.M. Conceptualizing oral health and oral health-related quality of life. SocSci Med. 1997;44:601-608.
CrossRef - Schrag C, Chang Y.M, Tsai C.Y, Wei F.C. Complete rehabilitation of the mandible following segmental resection. J Surg. Oncol. 2006;94:538-545.
CrossRef - Cantor R, Curtis T.A. Prosthetic management of edentulous mandibulectomy patients. I. Anatomic, physiologic, and psychologic considerations. J Prosthet Dent. 1971;25:446–57.
CrossRef - Mancuso D.N., Goiato M.C.,Filho G .H., Gomes E.A. Bite force and masticatory efficiency in implant-retained dentures: literature review. Dent Today. 2008;27(8):56–5810.
- Iizuka T., Hafliger J., Seto I., Rahal A,Stern R., Smolka K. Oral rehabilitation after mandibular reconstruction using an osteocutaneous fibula free flap with endosseous implants. Factors affecting the functional outcome in patients with oral cancer. Clin. Oral. Implants Res. 2005;16(1):69–79.
CrossRef - Schiegnitz E., Al-Nawas B., Kammerer P.W., Grotz K.A. Oral rehabilitation with dental implants in irradiated patients: a meta-analysis on implant survival. Clin. Oral Investig. 2014;18(3):687–698.
CrossRef - Patil P.G. Conventional complete denture for a left segmental mandibulectomy patient: A clinical report. J Prosthodont Res. 2010;54:192–7.
CrossRef - Meijer G.J, Dieleman F.J, Bergé S.J, Merkx M.A. Removal of an oral squamous cell carcinoma including parts of osseointegrated implants in the marginal man dibulecto my. A case report. Oral Maxillofac Surg. 2010;14:253–6.
CrossRef








