Manuscript accepted on :24-Aug-2018
Published online on: 06-09-2018
Plagiarism Check: Yes
Reviewed by: Prof Dr M Zak Khalil MD
Second Review by: Suprakash Chaudhury
Final Approval by: Dr Ayush Dogra
Bimal Chhajer , Vikram Singh
, Vikram Singh , Girija Kumari
, Girija Kumari and Mahendra Lohmor
and Mahendra Lohmor
Department of Preventive Cardiology, Saaol Heart Center, New Delhi, India.
Corresponding Author E-mail: vsmicroaiims@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1489
Abstract
This study was designed to evaluate the impact of yoga based lifestyle intervention on coronary artery disease (CAD) patients. This multi-centric prospective study was held in the Saaol heart center in different cities (Delhi, Kolkata, Bangalore, Chennai, and Mumbai) of India from 1995 to 2015. In this study, total 5,000 CAD patients having co-morbidity of obesity, hypertension, and diabetes were enrolled. A yoga-based lifestyle modification counseling (consist the essential components; cardiac education, plant-based balanced diet, regular walk, yoga, and meditation) was administrated to study subjects and clinical assessment was done using Saaol safety wheel as a holistic tool. In the beginning, lifestyle modification counseling was provided every month for one year and after one year the counseling was repeated for every six months with clinical assessment till the end of the study. The results of this study demonstrate a significant improvement in angina with reduction of New York Heart Association (NYHA) angina classification score from 3.08±0.56 (mean±SD) to 2.45±0.70 and also reduce the intake of anti-anginal drugs from 4.36±1.35 to 3.82±1.20. In this study, a significant improvement was also observed in heart attack protection score from 56.68±13.53 to 104.13±14.55. After the adherence to yoga-based lifestyle modification counseling components and Saaol safety wheel, 98% study subjects showed the significant improvements in clinical outcomes (BMI, blood pressure, and lipid parameters) and cardiac patients reduced the risk of heart attack and cardiac events. This study concludes that yoga-based lifestyle intervention is a non-invasive effective treatment method to control and prevent cardiac risk factors in CAD patients. This type of holistic approach may help to reduce the rate of cardiac events and heart attacks but there is further long-term multicentric randomized controlled trials are required for better clinical outcomes.
Keywords
Coronary Artery Disease; Cardiovascular Events; Heart Disease; Risk Factors
Download this article as:| Copy the following to cite this article: Chhajer B, Singh V, Kumari G, Lohmor M. Effect of Yoga based Lifestyle Intervention on Coronary Artery Disease Patients. Biomed Pharmacol J 2018;11(3). |
| Copy the following to cite this URL: Chhajer B, Singh V, Kumari G, Lohmor M. Effect of Yoga based Lifestyle Intervention on Coronary Artery Disease Patients. Biomed Pharmacol J 2018;11(3). Available from: http://biomedpharmajournal.org/?p=22293 |
Introduction
Cardiovascular diseases (CV) are the prime cause of premature death and disabilities throughout the world, more people die annually from CVDs when compared with from another cause. About 17.5 million people died from CVDs annually, representing 31% of all global deaths. Cardiovascular disease, especially coronary Artery Disease (CAD) is the leading cause of morbidity and mortality globally with more than 17.3 million deaths annually. CAD is responsible for about 15% of all deaths in the world. It is the number one killer in India and has a prevalence of 11% in urban and 5% rural settings. The problem of chronic diseases, including CAD, is rapidly rising worldwide. It is estimated that, by 2020, these diseases will be the cause of almost several quarters of all deaths worldwide understanding that 71% of deaths caused by coronary heart diseases (CHD), 75% of deaths caused by the stroke in addition to 70% of deaths caused by diabetes can occur throughout developing countries. Using a global foundation, 60% of the burden of chronic diseases will come about in developed countries. Cardiovascular diseases are however more quite a few in India and China than in all the in the economy developed countries on the globe put together.1-12
CAD is associated with a higher risk of cardiovascular events, including myocardial infarction (MI) and stroke. The prime cause of CAD is modern lifestyle and urbanization and several risk factors such as dyslipidemia, hypoglycemia, high triglyceride, hypertension. Obesity increases the progression of endothelial injury and develops atherosclerosis, which further causes serious cardiac arrest; heart attack.6,13
Numerous clinical research studies, including the Framingham, indicated the major risk factor for CAD includes high cholesterol, high triglyceride, low HDL, hypoglycemia, smoking, fatty food, excess intake of oil, lack of exercise, walking and less fibrous diet, stress. Changing of the modern lifestyle with medication can prevent coronary artery disease and the complication of preventive therapy for coronary artery disease patients. Primary prevention of CAD consists of interventions promoting a healthy lifestyle in the general population.8
CAD risk factors can be modified by lifestyle changes and it has been observed by various research studies that lifestyle changes can reduce the morbidity and mortality of CAD. Lifestyle modification counseling is the primary goals for prevention and control of CVD, and may significantly improve cardiac risk factors. Lifestyle modification counseling commonly used as an intervention tool, is a novel, non-invasive method to control CHD, T2DM, hypertension and other lifestyle- related chronic diseases. LMC includes- education about the disease (CHD), self-management and behavior change counseling, balanced diet, weight management, physical activity (walk, and yoga), tobacco and smoking cessation, and stress management counseling. Several studies showed that a poor knowledge about disease is associated with a higher BMI, prolonged use of medicines, poor glycemic control, and more complications and co-morbidities. Hence, patients require repeated health education and lifestyle modifying interventions through physicians and other health educators.14-16
A study done by Artinian et al demonstrates the effectiveness of lifestyle modification counseling with significant improvement in cardiovascular health and significant reductions In BMI, systolic and diastolic blood pressure, total cholesterol, fasting glucose and as well as improvements in physical activity and medication adherence. Lack of awareness and non-adherence to lifestyle modification program due to complexity in content and counseling are the aspects that encourage conduct SAAOL Heart study for preventing of coronary artery disease. To investigate this approach, a comprehensive, holistic model is used to prevent and manage coronary heart disease risk factors that reduce serious cardiac events such as heart attack and stroke.17-18
There are only a few studies in India, which have attempted to establish a comprehensive lifestyle modification counseling approach with larger populations and assessing long-term effectiveness of LMC. We aimed to introduce such intervention and hypothesized that lifestyle modification counseling will be more effective and will improve cardiac health in CHD patients. Therefore, the aims of this study were to evaluate the impact of the SAAOL lifestyle program using a holistic model in the prevention of coronary artery disease.
Materials and Methods
Study Design and Setting
This was a multi-centric prospective lifestyle intervention study, which was conducted in the SAAOL Heart Center in different cities (Delhi, Kolkata, Bangalore, Chennai & Mumbai) of India from September 1995 to December 2015. In this study, total 5,000 CAD patients with and without co-morbidity (Obesity, Hypertension, and Diabetes Mellitus) was enrolled based on a consecutive sampling technique. This study was conducted in two phases. In the first phase of planning, preparation for counseling components and recruitment of participants was done and in the second phase the implementation of counseling, data collection, follow-ups, and data analyses. The consort diagram is given in Table 1.
Eligibility Criteria
The patients were included in this study if they were clinically and diagnostically confirmed coronary artery disease with and without co-morbidity (obesity, hypertension and diabetes mellitus) patient either sex, aged 30 years to 70 years, CAD patients having symptoms of angina, Patients with coronary artery disease and unsuitable response to medical treatment and not willing for CABG (Coronary Artery Bypass Grafting ) & PTCA (Percutaneous Trans Coronary Angioplasty), patients with angiographically documented and having at least one vessels disease (blockage in any 3 main arteries RCA, LAD, LCX more than 70%) and willing to participate and able to give valid written inform consent. The patients were excluded if they were having several conditions such as peripheral arterial disease, cerebrovascular disease, Renal artery stenosis, aortic aneurysm, pulmonary heart disease, cardiac dysrhythmias, inflammatory heart disease, endocarditis, inflammatory cardiomegaly, myocarditis, valvular heart disease, congenital heart disease, rheumatic heart disease and pregnant woman and unwilling to participate and give written consent.
Sample Size
A total of 5,000 subjects was recruited based on consecutive sampling technique from the SAAOL Heart Centre, Delhi. The minimum calculated sample size for this study was 4147 with a margin of error 2% and confidence of the interval of 99%.
The sample size for the proposed study was calculated by the standard formula
Here, Z is the corresponding confidence interval, e is the margin of error and p is the estimated value of the proportion of samples having the condition of interest.
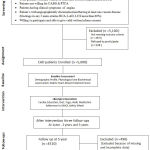 |
Table 1
|
Lifestyle Intervention
The intervention of the study participants commenced in 1995 and ended in 2015. The minimum 5-year intervention program consisted of two phases; with an active period (continuous Lifestyle modification counseling for one year at every month) and the maintenance period (Lifestyle counseling was provided at six-month intervals for four years). Lifestyle modification counseling through the Saaol safety wheel was used as an intervention tool for participants to prevent and control CHD. The Saaol safety wheel was developed as a tool for heart patients to follow their progress and also to find out their fault. The Saaol safety wheel has three wheels- one for reversing heart disease (green wheel), one for keeping blocks at a steady level (yellow wheel) and one for growing the blockage (red wheel). The Saaol safety wheel has 18 components (cholesterol, triglyceride, HDL ratio, systolic and diastolic blood pressure, blood sugar fasting, blood sugar PP, tobacco/ smoking, BMI,walk, oil intake, milk intake, fruit intake, salad intake, animal food intake, yoga, meditation, and stress level) marked at the level of green, yellow and red, as per their levels in the body. Saaol safety wheel is described in the below figure.
 |
Figure 1
|
Measurement and follow up of the study participants was done at baseline, 1st, 3rd and 5th year. The research team were prepared to study materials, support and supervised the lifestyle intervention sessions. All lifestyle intervention sessions were coordinated and facilitated by the trained and qualified dietitian, yoga teacher, and heart care expertise under the supervision of research expert in the SAAOL heart center, New Delhi. The intervention components were described through counseling in the local language, supported by pictures, videos, and discussions with separable or a group of patients. Each session took approximately 15-20 min and the five counseling components described in table 2.
Table 2: Five key components of Lifestyle Modification Counseling (LMC) using the SAAOL Safety Wheel.
| Intervention | Sessions Conducted by | Description of the Intervention | Rationale |
| 1. Cardiac Education | Heart care expert | Participants were educated about heart, heart diseases, heart attack, angina, signs and symptoms of angina, risk factors responsible for heart disease, complications and management of chronic diseases and emphasize the benefits of lifestyle modification; diet, walk, yoga, and meditation. | Cardiac education may increase awareness and adherence to follow a healthy lifestyle and help to reduce angina episode and preventing of coronary artery disease. |
| 2. Balanced (Oil-free) diet | Dietician | Participants were encouraged to cut down high-calorie food, animal food and minimal milk intake (skimmed) and advised to increase the amount of fibrous food (whole grain, salad, green vegetables, and fruits). Participants with family were trained to prepare oil-free food. Study participants advised to follow and adhere to zero oil food with balanced diet chart and SAAOL safety wheel. | Balanced diet help in weight & blood pressure management glycemic control. Fibrous diet fruits reduce the blood sugar and cholesterol level. |
| 3. Walking | Physical trainer | Participants were motivated to adhere on a regular brisk walk for at least 30 minutes per day. | Walking reduces the angina stability, blood glucose level, cholesterol and triglycerides, blood pressure, and improves the response to the anti-angina drugs. |
| 4. Yoga | Yoga teacher | Training of yoga asana (Mudrasana, Balasana, Vajrasana, Paschimottanasana, Ardha Matsyendrasana, Supta Vajrasana, Dhanurasana, Shavasana) was given and advised to adhere the practice for 30 minutes per day. | Yoga may reduce cardiac risk factors and improve angina stability, blood glucose level, cholesterol and triglycerides, blood pressure and also helps in stress management and improvement in health-related quality of life. |
| 5. Meditation | Yoga and spiritual teacher | The participants were encouraged to do daily Preksha meditation and breathing exercise at least for 15 minutes to control stress. | During meditation, the level of stress hormone (adrenaline and cortisol) reduced which further help to reduce stress levels and improve cardiac health and glycemic control. |
Measurements
Demographic details (Age, sex, medical history, family history) of the study participants had been done at baseline. The outcome measures for this study was BMI, systolic and diastolic blood pressure, pulse, total cholesterol, triglyceride, LDL cholesterol, HDL cholesterol, blood sugar fasting, blood sugar PP, and adherence to counseling or SAAOL safety wheel. The measurement of all study outcomes was assessed at baseline, 1st, 3rd and 5th year follow up. Height and weight of the participants were measured using a ‘Stadiometer’ and ‘SECA’ digital scale, and BMI was calculated using the formula of weight in kg divided by height in m2 (kg/m2). Trained personnel assessed the blood pressure using ‘Pagoda (mercury) B.P’ instrument. Cholesterol was assessed by the CHOD-PAP method, triglyceride by GPO method, HDL- cholesterol by immune inhibition method and LDL was calculated using a standard formula [LDL = Total Cholesterol – HDL – (Triglycerides/5)]. Fasting and PP blood glucose tests were analyzed using ‘Contour Plus One’ blood glucose monitoring system. Adherence to lifestyle intervention (saaol safety wheel) among CHD patients were assessed through SAAOL heart attack protection score. This is a unique scoring system to assess the adherence of the saaol safety wheel. The total possible score was 180 if the score above 90 or 50 % score indicated good adherence.
SAAOL Heart Protection Scoring was as follows ; Cholesterol (below 130mg/dl=10, 130-149mg/dl=5, 150-180mg/dl=1, above 180mg/dl=0), Triglyceride (below 100mg/dl=10, 100-129mg/dl=5, 130-160mg/dl=1, above 160mg/dl=0), HDL/Cholesterol percentage (above 40%=10, 25-40%=5, 20-24%=1, below 20%=0), Systolic B.P (below 120mmHg=10, 120-129mmHg =5, 130-140 mmHg =1, above 140 mmHg =0), Diastolic B.P (below 80mmHg=10, 80-89mmHg =5, 90-100 mmHg =1, above 100 mmHg =0), Fasting Blood Sugar (below 100mg/dl=10, 100-109mg/dl=5, 110-120mg/dl=1, above 120mg/dl=0), PP Blood Sugar (below 140mg/dl=10, 140-159mg/dl=5, 160-200mg/dl=1, above 200mg/dl=0), Tobacco (Zero=10, One/day=5, 2-3/day=1, more than 3/day=0), BMI (below 24 kg/m2 =10, 24-24.9 kg/m2 =5, 25-26 kg/m2 =1, above 26 kg/m2 =0), Walking per week (5-7d/week=10, 3-4d/week =5, 1-2d/week =1, Nil=0), Oil intake (Zero Oil=10, Negligible=5, Limited=1, Unlimited=0), Milk intake (below 200 ml (Skimmed)=10, 200-250ml (double tonned) =5, 250-300 ml (Full cream) =1, above 300 ml (Full cream)=0) , Fruits intake (5-7d/week=10, 3-4d/week =5, 1-2d/week =1, Nil=0), Salad intake (5-7d/week=10, 3-4d/week =5, 1-2d/week =1, Nil=0), Non-Veg (Animal) Food (None=10, one day/month =5, one day/week =1, almost everyday=0), Yoga (5-7d/week=10, 3-4d/week =5, 1-2d/week =1, Nil=0), Meditation (5-7d/week=10, 3-4d/week =5, 1-2d/week =1, Nil=0), Stress level (Negligible=10, Mild=5, Moderate=1, Severe=0), Total Score=180, Passing Mark = 90 (50%).
Statistical Analysis
Statistical package for the social sciences (SPSS) software version 21 was used for all statistical analyses. In this study percentage, mean, SD, median and sample paired t-test, repeated measures and multi-variant analysis was done to assess the study parameters.
Ethical Approval and Consent
Ethical approval for this study was granted by the ethics committee of SAAOL Heart Center New Delhi. Informed consent has been obtained from all enrolled study participants.
Results
Recruitment and Response Rate of Participants
This was a prospective lifestyle intervention, which was held in SAAOL Heart Center, New Delhi from September 1995 to December 2015. A total of, 5,000 subjects were enrolled. After 5 years of follow up only 4510 subjects to complete the entire process of study and their data were analyzed.
Baseline Characteristics of the Participants
The mean age of study participants was 54.96±9.87. This study data has 3836 (85.06%) males and 674 (14.94%) females. The majority of patients have co-morbidity of obesity 1291 (28.63%), hypertension 1759 (39.01%), and diabetes 679 (15.06%). In this study, 1264 (28.03%) patients were having the family history of heart disease. The positive cases of TMT were 4069 (90.22%) in this study. In this study, the maximum number of double vessel disease (DVD), 4068 (90.19%) was documented, followed by TVD (5.14%) and SVD (4.67%). Participant having CABG history were 1209 (26.81%) and PTCA were 1485 (32.93%). Participants having MI history were 329 (7.29) in this study. EF of participants was 48.20±8.41 and HR mean of participants was 70.71±4.59. The baseline characteristics of the study subjects are presented in table 3.
Table 3: Baseline demographic characteristics of participants.
| Baseline Characteristics of Study Participants | ||
| Variables | n=4510 | |
| Age (Mean ± SD) | 54.96±9.87 | |
| Gender (%) | Male | 3836 (85.06) |
| Female | 674 (14.94) | |
| Obesity (%) | Yes | 1291 (28.63) |
| No | 3219 (71.37) | |
| Hypertension (%) | Yes | 1759 (39.01) |
| No | 2751 (60.99) | |
| Diabetes (%) | Yes | 679 (15.06) |
| No | 3831 (84.94) | |
| Family history of Heart Disease (%) |
Yes | 1264 (28.03) |
| No | 3246 (71.97) | |
| TMT (%) | Positive | 4069 (90.22) |
| Negative | 441 (9.78) | |
| Classification of CHD (%) | SVD | 210 (4.67) |
| DVD | 4068 (90.19) | |
| TVD | 232 (5.14) | |
| CABG (%) | Yes | 1209 (26.81) |
| No | 3301 (73.19) | |
| PTCA (%) | Yes | 1485 (32.93) |
| No | 3025 (67.07) | |
| MI (%) | Yes | 329 (7.29) |
| No | 4181 (92.71) | |
| EF (Mean ± SD) | 48.20±8.41 | |
| HR (Mean ± SD) | 70.71±4.59 | |
Effect of LMC in Cardiac Risk Factors
A significant change was observed in cholesterol from baseline (175.43±44.82) to 5 years (128.97±47.72) of follow up with p<0.0001. There was also a significant change, observed in triglyceride from baseline (157.55±35.91) to 5th year (99.77±19.52) of follow up. A significant increment in HDL/Cholesterol percentage was also observed from baseline (24.96±7.94) to 5th year (42.10±16.54) of follow up.
A significant reduction in systolic blood pressure was observed from baseline (135.02±19.89) to 5th year (117.06±5.32) of follow up with p<0.001. A significant reduction in diastolic blood pressure was also observed from baseline (87.54±9.69) to 5th year (75.28±5.01) of follow up with p<0.001. There was a significant improvement in blood sugar fasting (106.47±29.44 to 98.47±23.81), blood sugar PP (140.88±66.50 to 128.97±47.72) was observed from baseline to 5th year of follow up. A significant improvement in BMI was also observed from baseline (25.71±3.90) to (23.98±4.34) with p<0.0001. The details of the results are given in table 4.
Table 4: Changes in Cardiac Risk Factors from Baseline to 1st year, 3rd year and 5th years of study follow-up.
| Variables | Baseline
Mean ± SD |
1 Year
Mean ± SD |
3 Year
Mean ± SD |
5 Year
Mean ± SD |
p-value
|
| Cholesterol | 175.43±44.82 | 128.97±47.72 | 134.0±30.06 | 144.78±47.83 | <0.0001 |
| Triglyceride | 157.55±35.91 | 99.77±19.52 | 107.37±15.44 | 128.67±41.09 | <0.0001 |
| HDL/Cholesterol percentage | 24.96±7.94 | 42.10±16.54 | 41.40±13.51 | 31.62±10.01 | <0.0001 |
| SBP | 135.02±19.89 | 117.06±5.32 | 118.0±4.17 | 119.99±1.73 | <0.0001 |
| DBP | 87.54±9.69 | 75.28±5.01 | 76.06±4.92 | 78.57±3.51 | <0.0001 |
| BSF | 106.47±29.44 | 98.47±23.81 | 100.18±23.71 | 102.45±27.37 | <0.0001 |
| BSPP | 140.88±66.50 | 128.97±47.72 | 130.28±45.93 | 135.57±56.63 | <0.0001 |
| BMI | 25.71±3.90 | 23.98±4.34 | 24.40±4.12 | 24.62±4.01 | <0.0001 |
A significant improvement in other cardiac risk factors Tobacco consumption, Walking, Oil intake, Milk intake, Fruit intake, Salad intake, Animal food, Yoga, Meditation and Stress Management was also observed. A significant change in tobacco consumption was observed from baseline median 2 to 0 at 5th year of follow up. Walking improves from median 2 to 6 at 5th year of follow up. Oil intake, the frequency was reduced from unlimited (median 3) to minimal (median 0) at 5th year of follow up. Milk intake was also reduced from unlimited (median 3) ; full cream milk to minimal (median 0); skimmed milk at 5th year of follow up. Fruit intake was increased from median 2 to 6 days/week at 5th year of follow up. Salad intake was also increased from median 1 to 6 days/week at 5th year of follow up. The frequency of animal food intake was also decreased from median 2 to 0 with the range of 0-3. Adherence to the yogic exercise was also increased from 1 day /week to 5 days/week at 5th year of follow up. Similarly, adherence towards meditation practice was also increased from 2 days/week to 5 days /week at 5th year of follow up. A significant improvement in stress management from excess (median 3) to a minimum (median 1) was observed at 5th year of follow up. The details of the results are given in table 5.
Table 5: Changes in Cardiac Risk Factors (Median) from Baseline to 1st year, 3rd year and 5th years of study follow-up.
| Variables | Median Range (Min-Max) | Baseline
Median |
1 Year
Median |
3 Year
Median |
5 Year
Median |
p-value |
| Tobacco | 0-3 | 2 | 0 | 1 | 1 | <0.0001 |
| Walking | 0-7 | 2 | 6 | 5 | 4 | <0.0001 |
| Oil intake | 0-3 | 3 | 0 | 1 | 1 | <0.0001 |
| Milk intake | 0-3 | 3 | 0 | 1 | 2 | <0.0001 |
| Fruit intake | 0-7 | 2 | 6 | 5 | 4 | <0.0001 |
| Salad intake | 0-7 | 1 | 6 | 5 | 4 | <0.0001 |
| Animal food | 0-3 | 2 | 0 | 1 | 2 | <0.0001 |
| Yoga | 0-7 | 1 | 5 | 4 | 4 | <0.0001 |
| Meditation | 0-7 | 2 | 5 | 4 | 3 | <0.0001 |
| Stress Level | 0-3 | 3 | 1 | 1 | 2 | <0.0001 |
Effect of LMC in Clinical Parameters
A significant improvement in New York Heart Association (NYHA) angina classification was observed from baseline (3.08±0.56) to 5th year (2.34±0.62) of follow up with p<0.0001. The number of drugs used for angina and heart disease was also decreased from baseline (4.36±1.35) to 5th year (2.95±0.65) of follow up after LMC. The detail of the results are given in table 6.
Table 6: Changes in Clinical Parameters from Baseline to 1st year, 3rd year and 5th years of study follow-up.
| Variables | Baseline
Mean ± SD |
1 Year
Mean ± SD |
3 Year
Mean ± SD |
5 Year
Mean ± SD |
p-value
|
| NYHA Angina Classification | 3.08±0.56 | 2.34±0.62 | 2.42±0.68 | 2.45±0.70 | <0.0001 |
| Intake of drugs (Anti-Anginal) | 4.36±1.35 | 2.95±0.65 | 3.12±0.58 | 3.82±1.20 | <0.0001 |
Impact of LMC using the SHS Wheel in CHD patients
A significant improvement in SAAOL Heart Attack (SHA) protection score was observed from baseline to 5th year of follow up. Cholesterol score was increased from 2.70±3.72 (baseline) to 8.48±3.48 (5th year) and triglyceride score was also increased from baseline (1.80±2.42) to 5 years (7.46±2.64) follow up. A significant increment in HDL/Cholesterol percentage was observed from baseline (2.69±2.52) to 5th year (7.02±3.03) of follow up. SBP score was increased from baseline (4.94±4.85) to 5th year (9.94±0.71) of follow up and DBP score was increased from baseline (3.56 ±1.96) to 5th year (7.36±2.49) of follow up. A significant improvement in BSF from baseline (6.74±3.61) to 5th year (7.60±3.63) of follow up and BSPP from baseline (8.43±3.56) to 5th year (8.65±3.23) of follow up was observed. Tobacco consumption score was also improved from baseline (4.89±4.48) to 5th year (7.57±2.50) of follow up. BMI score was also improved from baseline (4.99±3.67) to 5th year (6.78±4.52) of follow up. Walking score also increase from baseline (1.01±0.31) to 5th year (9.95±0.49) of follow up. The Oil intake score was also improved from baseline (1.12±0.46) to 5th year (7.76±2.51) of follow up. The Milk intake score was also improved from baseline (1.52±0.91) to 5th year (5.52±4.22) of follow up.
A significant improvement in fruit intake score was observed from baseline (3.73±1.90) to 5th year (9.85±0.90) of follow up. The salad intake score was also increased from baseline (2.79±2.02) to 5th year (8.58±2.27) of follow up. Intake of animal food score was also improved from 3.45±2.39 (baseline) to 8.46±2.43 (5th year) of follow up. A significant improvement in the yogic exercise was also observed from baseline (1.11±0.70) to 5th year (7.00±2.48) of follow up. Meditation score was also improved from baseline (1.04±0.51) to 5th year (7. 36±2.50) of follow up. A significant improvement in stress management score was observed from baseline (1.72±1.04) to 5th year (5.19±1.37) of follow up. A significant improvement was observed in total SHA protection score from baseline (56.68±13.53) to 5th year (140.60±15.62) of follow up after LMC with p<0.0001. The complete information about SHA protection scoring and clinical outcomes are given in table 7 and 8.
Table 7: Changes in SHA Protection score from Baseline to 1st year, 3rd year and 5th years of study follow-up.
| Variables | Baseline
Mean±SD |
1 Year
Mean±SD |
3 Year
Mean±SD |
5 Year
Mean±SD |
p-value
|
| Cholesterol | 2.70±3.72 | 8.48±3.48 | 6.75±4.12 | 5.47±4.30 | <0.0001 |
| Triglyceride | 1.80±2.42 | 7.46±2.64 | 6.17±2.50 | 4.44±2.26 | <0.0001 |
| HDL/Cholesterol percentage | 2.69±2.52 | 7.02±3.03 | 6.49±3.51 | 4.69±3.12 | <0.0001 |
| SBP | 4.94±4.85 | 9.94±0.71 | 9.98±0.37 | 9.97±0.46 | <0.0001 |
| DBP | 3.56 ±1.96 | 7.36±2.49 | 6.97±2.44 | 5.71±1.75 | <0.0001 |
| BSF | 6.74±3.61 | 7.60±3.63 | 7.58±3.67 | 7.56±3.69 | <0.0001 |
| BSPP | 8.43±3.56 | 8.65±3.23 | 8.60±3.28 | 8.52±3.50 | <0.0001 |
| Tobacco Consumption | 4.89±4.48 | 7.57±2.50 | 7.23±2.51 | 6.86±3.03 | <0.0001 |
| BMI | 4.99±3.67 | 6.78±4.52 | 6.42±4.57 | 5.54±3.98 | <0.0001 |
| Walking | 1.01±0.31 | 9.95±0.49 | 9.96±0.43 | 7.29±2.73 | <0.0001 |
| Oil intake | 1.12±0.46 | 7.76±2.51 | 7.25±2.50 | 5.53±4.14 | <0.0001 |
| Milk intake | 1.52±0.91 | 5.52±4.22 | 5.34±4.24 | 2.11±1.81 | <0.0001 |
| Fruit intake | 3.73±1.90 | 9.85±0.90 | 8.97±2.08 | 6.64±2.71 | <0.0001 |
| Salad intake | 2.79±2.02 | 8.58±2.27 | 6.25±2.17 | 5.93±2.28 | <0.0001 |
| Animal food | 3.45±2.39 | 8.46±2.43 | 5.58±4.23 | 4.41±4.25 | <0.0001 |
| Yoga | 1.11±0.70 | 7.00±2.48 | 5.91±2.27 | 5.34±2.00 | <0.0001 |
| Meditation | 1.04±0.51 | 7.36±2.50 | 5.78±2.08 | 4.59±1.33 | <0.0001 |
| Stress Level | 1.72±1.04 | 5.19±1.37 | 5.38±2.03 | 4.62±4.26 | <0.0001 |
| Total SHAP Score | 56.68±13.53 | 140.60±15.62 | 126.69±14.09 | 104.13±14.55 | <0.0001 |
Table 8: Changes in outcomes from baseline to 1 year, 3 year and 5 Year follow up follow-up with differences in within and between groups over time.
| Variables | Mean change from Baseline to 1 Year of follow up | Mean change from Baseline to 3 Year of follow up | Mean change from Baseline to 5 Year follow up | p-value |
| Cholesterol | 46.45 ( 44.52-48.38 ) | 41.43 (39.84-43.01) | 30.65(28.9-32.4 ) | <0.0001 |
| Triglyceride | 57.7 (56.58-58.95 ) | 50.17(49.03-51.32 ) | 28.88 (27.28-30.48 ) | <0.0001 |
| HDL/Cholesterol % | -17.14 (-17.68- – 16.61 ) | 16.44(-16.90 – – 15.98 ) | -6.65 ( -7.01 – – 6.30) | <0.0001 |
| SBP | 17.96(17.36-18.55 ) | 17.01(16.42-17.6) | 15.02(14.44-15.60) | <0.0001 |
| DBP | 12.25 ( 11.93-12.58 ) | 11.47( 11.15-11.79 ) | 8.9(8.66-9.26) | <0.0001 |
| BSF | 8.01 (7.46-8.54 ) | 6.29(5.77-6.80 ) | 4.02(3.56-4.47 ) | <0.0001 |
| BSPP | 11.9(10.94-12.86 ) | 10.59(9.64-11.55) | 5.30(4.64-5.96) | <0.0001 |
| Tobacco Consumption | 0.67 (0.64-0.71 ) | 0.62( 0.57-0.64 ) | 0.51(0.48-0.55) | <0.0001 |
| BMI | 1.68 (1.60-1.76) | 1.31(1.23-1.39 ) | 1.09(1.01-1.17 ) | <0.0001 |
| Walking | -4.01(-4.02- – 3.99) | -3.31(-3.33- – 3.29 ) | -2.46(-2.51- – 2.42 ) | <0.0001 |
| Oil intake | 1.94 (1.91- 1.96) | 1.84(1.81-1.86 ) | 1.41( 1.37 – 1.45) | <0.0001 |
| Milk intake | 1.41(1.37-1.44 ) | 1.35( 1.32-1.39) | 0.59(0.56-0.62 ) | <0.0001 |
| Fruit intake | -3.47 (-3.29- – 3.24) | -2.21 (-2.23- – 2.17 ) | -1.43(-1.46- – 1.38 ) | <0.0001 |
| Salad intake | -3.59 (-3.63- – 3.54 | -2.97(-3.02- – 2.93 ) | -2.25(-2.31 – – 2.19 ) | <0.0001 |
| Animal food | 1.63 (1.59-1.66 ) | 0.96(0.92-1.01 ) | 0.61(0.56-0.65 ) | <0.0001 |
| Yoga | -3.74 (-3.77- – 3.71 ) | -2.98(-3.02- – 2.94 ) | -2.46(-2.50 – – 2.43) | <0.0001 |
| Meditation | -3.45 (-3.47- – 3.42 ) | -2.45(-2.48 – – 2.41) | -1.23(-1.25- -1.21) | <0.0001 |
| Stress Level | 1.37 (1.34- 1.38) | 1.31(1.27-1.34 ) | 1.08(1.04- 1.12) | <0.0001 |
Means differences within and between group are in mean (95% Confidence Interval), a negative change indicates a fall on average from baseline to 1 year, baseline to 3 years and baseline to 5 years follow up. Determined repeated measures ANOVA within and between groups comparison and multi-variant analysis for significant change at p<0.05.
Cost – Effectiveness of Treatment
Lifestyle intervention was observed cost-effective treatment method with intervention cost (2400 INR-3000 INR) as compared to CABG (1,50,000 INR-4,50,000 INR) and PTCA (1,20,000 INR-1, 60,000 INR) treatments. The median of intervention cost was 2400 INR at 1 year follow up, 2500 INR at 3rd year follow up and 3000 INR at the end of the intervention (overall median 2700 INR) on the other side cost of CABG was range from 1,50,000 INR to 4,50,000 INR (Median 3,00,000) and PTCA was range 1,20,000 INR to 1,60,000 (median 1,40,000 INR) was observed. Hence, lifestyle intervention is a cost-effective treatment method for CAD patients.
Clinical Assessment at the end of the Study
Our study revealed that 98% of CAD patients avoided heart attack and other treatment options such as CABG and PTCA. Only 2% of CAD patients had the history of minor attacks and other health problems.
Discussion
The purpose of this study was to determine the effectiveness of lifestyle modification counseling using the SAAOL Heart Safety wheel on cardiac risk factors at the 1st, 3rd and 5th year follow-ups. The results of our study indicate the significant improvement in NYHA angina classification and reduced the number of medicines used to treat coronary heart disease patients. The SAAOL Heart Safety wheel was found an effective and reliable tool in the management and control of cardiac risk factors. A study done by Dean Ornish reported that CAD can be reversed and control through dietary changes, yoga, walk and meditation.14-15
Effect of LMC on Angina and Medications
The present study showed a significant improvement in NYHA angina class and number of angina medicines was also reduced from baseline to 5th year follow up. Similarly, a study done by Yogendra et al supports the present study and showed a significant improvement in functional class (NYHA II to NYHA I), angina symptoms, and reduce the consumption of the nitrate tablets (medicines) after lifestyle modification and yoga practice .19
Effect of LMC on Cardiac Risk Factors
The results of the present study showed significant improvement in lipid profile (total cholesterol, triglyceride, HDL/cholesterol ratio), from the 1st follow up to 5th year follow up after lifestyle intervention.
A similar study done by Ibhar et al showed a significant decrease in total cholesterol from baseline to 2 year follow-up.20 Similarly, studies done by Browning et al showed significant improvements in triglycerides, HDL, LDL cholesterol HbA1c, and BMI, in the intervention group after receiving a motivational intervention counseling.21 Likewise, Yogendra et al 19 found statistically significant changes in the serum total cholesterol, triglyceride and LDL cholesterol after receiving educational counseling regarding disease, diet, and exercise for three months.19 The role of healthy and balanced diet in lipid metabolism cannot be undervalued, and it was clearly recognized by Sasakabe et al in his study, they found that a significant reduction in LDL-C and a significant increase in HDL-C, by accepting a low fat and carbohydrate diet for three months.22 These findings indicate an improvement in health status, quality of life, and decreased the risk of cardiovascular other complications. These findings are similar to the present study, with the decrease in carbohydrates consumed together, and an increase in the frequency of vegetable consumption possibly accounting for these improvements. Another study on a heterogeneous group of patients with hypertension, CAD, DM, and a variety of other illnesses using lifestyle education program based on yoga, Manjunatha S et al. reported that fasting plasma glucose, serum total cholesterol, LDL, VLDL, the ratio of total cholesterol to HDL and triglycerides were significantly lower and HDL was significantly higher on the 5th Yearday of the lifestyle educational course compared to the first day of the course.23 The results of the present study showed a significant reduction in BMI from baseline to 5th year of study follow up.
The results of the present study showed significant improvement in systolic and diastolic blood pressure from baseline to 5th year study follow up. A randomized clinical trial done by Maruthur et al showed a significant reduction in cardiovascular risk factors and blood pressure after a 1-year telephonic intervention counseling.24 The authors reported a significant reduction in blood pressure similar to our study regarding the decline in hypertension in the study participants. Studies by Balducci et al25 found that with a significant reduction in SBP and DBP in the experimental group after following 12 months aerobic and resistance exercise program. Similar results were described by Ades et al 26 after following a six-month diet and exercise intervention where there was a slight decrease in SBP, but a statistically significant decrease in DBP. A 12 months exercise program, conducted by Balducci et al 25 testified decreases in SBP and DBP from baseline to 12 months in both the control and experimental groups, although the greater decrease had been observed in the experimental group for both SBP and DBP. A study done by Sasakabe et al reported that a statistically significant decrease in SBP and DBP after adopting a low-carbohydrate diet.22
The results of the present study showed significant improvement in body weight and BMI from baseline to 5th year study follow up. In A study done by Backer et al showed similar and significant decrease weight and BMI in the patients with a history of CVD by following structured lifestyle intervention program. 27 In a recent study by Emerenziani et al found a significant decrease in BMI in the experimental group and no change in the control group after adhering 3 month aerobic exercise program.28 A study by Ornish et al 14 showed a significant reduction in body weight of CHD patients in the intervention group.
A significant improvement was observed in BSF and BSPP from baseline to 5th year of study follow up. The study results conclude that lifestyle modification counseling can give significant and beneficial impact on blood sugar levels. Studies done by Oldroyd et al and Ibrahim et al reported a decrease in the blood sugar levels after lifestyle interventions in at 1 year to follow up.29-30 In the present study, we found similar results, i.e. a decrease in blood sugar levels in participants. Studies done by Greaves et al found the significant reduction in blood sugar levels, insulin resistance, anti-diabetic medicines and body weight through diet and physical activity interventions.31
The results of the present study showed the significant reduction in tobacco consumption from baseline to 5th year of study follow up. There was a statistically significant reduction in tobacco use at three and six months in the study group as compared to the control group.
The present study showed a significant improvement in walking and functional capacity from baseline to the 5th year of study follow up after following Saaol safety wheel. A randomized controlled trial done by Thomas et al demonstrated that physical activity like walking can delay the progression of cardiovascular risk factors, impaired glucose tolerance when combined with dietary changes. The significant Improvements in cardiovascular risk factors, cardiorespiratory fitness, blood pressure, insulin resistance glycemic control, blood lipid profile, and decreased stress, anxiety, depression and chronic medication dosages in CHD and other chronic disease patients after adhering regular walk and physical activity is documented.32
A study done by Franciosi et al shown that patient with CHD and T2DM who reported walking for at least two hours per week had a 39% lower all-cause mortality rate than those who reported no walking. 33 A significant reduction in animal food intake, oil intake, and milk intake was observed in study participants from baseline to 5th year of study follow up. It is proven that the vegetarian diet is healthful and effective in weight management, glycemic control, reversing atherosclerosis, decreasing blood lipids, blood pressure and have favorable effects on diabetes, cardiovascular problems, obesity and other chronic diseases. The vegetarian diet is effective in the prevention and treatment of CHD and provides metabolic and cardiovascular benefits.
A significant improvement was observed in fruit and salad intake from baseline to 5th year study follow up. The results of the present study are similar to study by Chandalia et al34 who found that the intake of a high fibrous diet shown 10 % improvement in glycemic control, 12 % improvement in insulin sensitivity and an about 9% decrease in lipid levels. A meta-analysis by Wu et al provided strong evidence that regular intake fibrous diet significantly reduces the risk of developing CHD, T2DM and other complications.35
It is validated the association between fruit and vegetable consumption and the risk of coronary heart disease using the nurses prospective health study and the health professionals follow-up cohort study.
A significant improvement was observed in yoga practice adherence from baseline to 5th year of study follow up. At baseline, there were very few patients practicing yoga asana, but after receiving education through yoga teacher most of the patient were adhere to yoga.
Mc Caffrey and Rao et al reported that yoga practice is helpful in weight management, waist-hip ratio, decrease cardiac risks, stress reduction, and quality of life of patients. The result of a study showed significant decreases systolic and diastolic blood pressure and heart rate, after Yoga. It is documented that yoga improves the immune system with enhanced immunoglobulin A and natural killer cells (NKC) in stressed people. In most of the clinical studies, modifiable CAD risk factors are heart rate, blood pressure, lipid profiles, and body mass index.36-37
A significant improvement in meditation adherence was observed in CHD patient from baseline to 5th year of study follow up. Studies done by Gotink et al found, in a recent systematic review and meta-analysis of systematic reviews, using standardized meditation program significantly improvement in depression symptoms, anxiety and stress, improving life quality and physical functioning.38 In a study by Rosensweig et al observed an improvement in glycemic control, depression, anxiety and psychological distress after following one month meditation program. A study conducted by Keyworth et al found a significant improvement in glycemic control, sleep, relaxation, and better acceptance of the disease.39-40
Limitations of the Study
There is no standard published tool to evaluate the holistic model adherence score of the participants besides only self-developed questionnaires and score was documented. This study was lacking the control group, which was the major drawback of the study design. Hence, there is a requirement of further multi-centric randomized control study with a larger population in the different region of India and abroad.
Conclusion
This study concludes that yoga-based lifestyle modification counseling through a holistic approach was effective in improving angina and cardiac risk factors. A significant reduction in the total number of medicines used for CHD was also observed in this study. This type of holistic approach may help to reduce the rate of cardiac events and heart attacks. There is further long-term multicentric randomized controlled trials are required for better clinical outcomes.
Conflict of Interest
The authors have no conflicts of interest related to the material presented in this original research paper.
Acknowledgments
Authors are thankful to health professionals of SAAOL Heart Center, New Delhi.
Funding Resource
Emami group of foundation gave financial assistance to carry out this study. Authors are very thankful for this kind of help.
References
- Dorairaj P., Jeemon P and Roy A. Cardiovascular diseases in India current epidemiology and future directions. Circulation. 2016;133:1605–20.
- Gupta R ., Mohan I and Narula J. Trends in Coronary Heart Disease Epidemiology in India. A n n a l s o f G l o b a l H e a l t h. 2016;82(2):307-315.
- Ramachandran S., Emelia V.,Benjamin J. The Future of Cardiovascular Epidemiology. Circulation. 2016;133:2626-2633.
- Ashna D. K. B., Lewey J., Sagar B. D and Niteesh K. C. The Burden of Cardiovascular Disease in Low- and Middle-Income Countries: Epidemiology and Management. Canadian Journal of Cardiology. 2015;31:1151-1159.
- Lin G. K. Cardiovascular epidemiology in the Asia–Pacific region. Asia Pacific J Clin Nutr. 2001;10(2):76–80.
- Kaur P ., Rao T. V and Sankarasubbaiyan S., et al. Prevalence and Distribution of Cardiovascular Risk Factors in An Urban Industrial Population in South India: A Cross- Sectional Study. JAPI. 2007;55:771-776.
- Chauhan S and Bani T. The rising incidence of cardiovascular diseases in India: Assessing its economic impact. Preventive Cardiology. 2015;4(4):735-740.
- Syed S. M., Levy D.,Ramachandran S. V and Thomas J. W. The Framingham Heart Study and the Epidemiology of Cardiovascular Diseases: A Historical Perspective. Lancet. 2014;383(9921):999–1008.
- Gerald M and Oppenheimer. Framingham Heart Study: The First 20 Years. Progress in Cardiovascular Diseases. 2010;53:55–61.
- Shrivastava A. M.,Mohan V. R. U and Bachani D. Obesity, Diabetes and Cardiovascular Diseases in India: Public Health Challenges. Current Diabetes Reviews. 2017;13:65-80.
- Chauhan A. S and Mukherjee K. Economic burden of coronary heart disease in North India. Int J Non-Commun Dis. 2016;1:18-25.
- Unnikrishnan R., Mohan R . A and Mohan V. Diabetes mellitus and its complications in India. Nature Reviews Endocrinology. 2016;12:357-370.
- Mokta J., Mokta K., Ranjan A and Garg M . Prevalence of Cardiovascular Risk Factors among Diabetic Population and Awareness of Diabetes among Diabetic Patients: A Population Based Himalayan Study. Journal of association of physicians of India. 2017;65:48-52.
- Ornish D., Larry W. S and James H. B. Intensive Lifestyle Changes for Reversal of Coronary Heart Disease. JAMA. 1998;280(23):2001-2007.
- Ornish D., Brown S. E., Billings J. H and Scherwitz L.W., et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. The Lancet. 1990;336(8708):129-133.
- Razavi M., Fournier S., Shepard D. S., Ritter G and Strickler G. K., et al. Effects of Lifestyle Modification Programs on Cardiac Risk Factors. PLoS ONE. 2014;9(12):114772.
- Artinian N. T., Fletcher G. F., Mozaffarian D and Burke L. E., et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:406–441.
- Aldana S. G.,Whitmer W. R., Greenlaw R and Avins A. L. Effect of intense lifestyle modification and cardiac rehabilitation on psychosocial cardiovascular disease risk factors and quality of life. Behav Modif. 2006;30(4):507-25.
- Yogendra., Hansaji J .Y and Ambardekar S., et al. Beneficial Effects of Yoga Lifestyle on Reversibility of Ischaemic Heart Disease : Caring Heart Project of International Board of Yoga. JAPI. 2004;52:283-89.
- Al I. M., Mohamed H. K and Yi-An K., et al. Effects of a Health-Partner Intervention on Cardiovascular Risk. J Am Heart Assoc. 2016;5:4217.
- Browning C.,Chapman A and Yang H., et al. Management of type 2diabetes in China: the Happy Life Club, a pragmatic cluster randomised controlled trial using health coaches. BMJ Open. 2016;6:9319.
- Sasakabe T., Haimoto H., Umegaki H and Wakai K. Association of decrease in carbohydrate intake with reduction in abdominal fat during 3-month moderate low carbohydrate diet among non-obese Japanese patients with type 2 diabetes. Metabolism. 2015;64(5):618–25.
- Manjunatha S., Vempati R. P., Ghosh D and Bijlani R. L. An investigation into the acute and long-term effects of selected yogic postures on fasting and postprandial glycemia and insulinemia in healthy young subjects. Indian J Physiol Pharmacol. 2005;49:319-324.
- Maruthur N. M., Wang N. Y and Appel L. J. Lifestyle interventions reduce coronary heart disease risk: Results from the PREMIER Trial. Circulation. 2009;119:2026–31.
- Balducci S., Leonetti F., Mario D. U and Fallucca F. Is a long-term aerobic plus resistance training program feasible for and effective on metabolic profiles in type 2 diabetic patients? Diabetes Care. 2004;27(3):841–42.
- Ades P., Savage P., Marney A., Harvey J and Evans K. Remission of recently diagnosed type 2 diabetes mellitus with weight loss and exercise. Journal of Cardiopulmonary Rehabilitation and Prevention. 2015;35(3):193–7.
- Backer G., Ambrosioni E., Borch-Johnsen K., Brotons C., Cifkova R., Dallongeville J., Ebrahim S., Faergeman O., Graham I and Mancia G., et al. European guidelines on cardiovascular disease prevention in clinical practice: third joint task force of European and other societies on cardiovascular disease prevention in clinical practice. Eur J Cardiovasc Prev Rehabil. 2003;10(4):1–10.
- Emerenziani G., Gallotta M., Meucci M., Luigi D. L., Migliaccio S., Donini L., Strollo F and Guidetti L. Effects of aerobic exercise based upon heart rate at aerobic threshold in obese elderly subjects with type 2 diabetes. International Journal of Endocrinology. 2014;2015; 1–7.
- Oldroyd J., Nigel C.U and White M., et al . Randomised controlled trial evaluating lifestyle interventions in people with impaired glucose tolerance. Diabetes Research and Clinical Practice. 2006;76:117-12.
- Ibrahim N., Moy M. F and Awalludin I. A. N., et al. Effects of a Community-Based Healthy Lifestyle Intervention Program (Co-HELP) among Adults with Prediabetes in a Developing Country: A Quasi-Experimental Study. PLoS. 2016;11(12):e0167123.
- Greaves., et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:119.
- Thomas D., Elliot E. J and Naughton G. A. Exercise for Type 2 diabetes. Cochrane Database of Systematic Reviews. 2006;3. Doi: 10.1002/14651858.CD002968.pub 2.
- Franciosi M., Pellegrini F., Berardis D. G., Belfiglio M., Cavaliere D., Nardo D and Nicolucci B. A. The impact of blood glucose self-monitoring on metabolic control and quality of life in type 2 diabetic patients: an urgent need for better educational strategies. Diabetes Care. 2001;24(11):1870-7.
- Chandalia M., Garg A., Lutjohann D., Bergmann V. K., Grundy and Brinkley S. L. Beneficial effects of high dietary fiber intake in patients with type 2 diabetes mellitus. New England Journal of Medicine. 2000;342:1392–1398.
- Wu Y., Zhang D., Jiang X and Jiang W. Fruit and vegetable consumption and risk of type 2 diabetes mellitus: A dose-response meta-analysis of prospective cohort studies. Nutrition, Metabolism and Cardiovascular Diseases. 2015;25(2):140–147.
- McCaffrey R., Ruknui P., Hatthakit U and Kasetsomboon P. The effects of yoga on hypertensive persons in Thailand. Holist Nurs Pract. 2005;19:173-180.
- Rao R. M., Telles S and Nagendra H. R. Effects of yoga on natural killer cell counts in early breast cancer patients undergoing conventional treatment. Comment to: recreational music-making modulates natural killer cell activity, cytokines, and mood states in corporate employees. Med Sci Mon. 2008;14:3-4.
- Gotink R. A., Chu P and Busschbach J. J. V., et al. Standardised Mindfulness-Based Interventions in Healthcare: An Overview of Systematic Reviews and Meta-Analyses of RCTs. PLoS ONE.,2015;10(4):0124344.
- Rosenzweig S., Reibel D. K and Greeson J. M., et al. Mindfulness-based stress reduction isassociated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Altern Ther Health Med. 2007;13(5):36-38.
- Keyworth C., Knopp J and Roughley K., et al. A Mixed-Methods Pilot Study of the Acceptability and Effectiveness of a Brief Meditation and Mindfulness Intervention for People with Diabetes and Coronary Heart Disease. Behavioral Medicine. 2014;40:53–64.







