Ahmad Fauzi1, Asrafi Rizky Gatham2, S. Dohar Al-Tobing3 and Luthfi Gatham2
1Department of Orthopaedic Surgery, Lampung University, Indonesia.
2Department of Orthopaedic Surgery, Fatmawati Hospital, University of Indonesia.
3Department of Orthopaedic Surgery, Ciptomangunkusumo Hospital, University of Indonesia.
Corresponding author E-mail: ahmadfauzi_dr@yahoo.co.id
DOI : https://dx.doi.org/10.13005/bpj/1458
Abstract
There are several options of surgical treatment of Hernia Nucleous Pulposus (HNP) such as discectomy and micro-endodiscectomy (MED). The fundamental differences between these procedures are the size of the incision, the discectomy procedure and the volume of disc taken. However, until now, there has not been any class 1 evidences explaining the efficacy of these procedures, and there is only a few studies about its safety and factors influencing its efficacy in treating HNP, especially in Indonesia. This study is aimed to assess clinical outcomes and safety of MED in HNP patients who underwent this procedure. Patient with HNP who underwent MED were followed prospectively in a period of January 2015 until December 2016. Clinical outcomes were evaluated by using Visual Analog Score (VAS) for assessing back pain and leg, and Oswestry Disability Index (ODI). The mean of pre-treatment score was compared with the mean of post-surgical treatment score by using paired t-test. Sampel were 78 HNP patients treated surgery. The average surgery duration (± SD) was 60 ± 17.1 minutes. The pretreatment score mean on VAS and ODI were 4.88 ± 1.10 and 35.21 ± 8.24. After surgical treatment, the VAS and ODI score obtained were significantly reduced to 1.53 ± 1.14 and 5.16 ± 5.52, respectively (p<0,001). A type of complication was observed, which was 5 (6.4%) cases of dural tear; no deficit in ankle dorsiflexion nor foot paresis were found. MED has been shown to be able to treat HNP with clinical outcomes similar to conventional open discectomy but with better levels of safety and effectiveness. However, this procedure still requires high quality randomized controlled trials studying about its efficacy and cost effectiveness in HNP treatment.
Keywords
Clinical Outcomes; Hernia Nucleous Pulposus; Microendodiscectomy
Download this article as:| Copy the following to cite this article: Fauzi A, Gatham A. R, Al-Tobing S. D, Gatham L. Clinical Outcomes of Hernia Nucleous Pulposus After Microendodiscectomy. Biomed Pharmacol J 2018;11(2). |
| Copy the following to cite this URL: Fauzi A, Gatham A. R, Al-Tobing S. D, Gatham L. Clinical Outcomes of Hernia Nucleous Pulposus After Microendodiscectomy. Biomed Pharmacol J 2018;11(2). Available from: http://biomedpharmajournal.org/?p=21032 |
Introduction
Due to the increasing incidence of chronic low back pain, including the one caused by hernia nucleous pulposus, numerous modalities have been available for diagnosis and management of this disorder. Besides that,the escalating costs and its impact on health care resources and our understanding of the causes, diagnosis and treatment of lumbar disc herniation has evolved over the past century.1
Symptomatic HNP has several options of treatment, including conservative treatment with only paintreatment, andsurgical treatment.2 Surgery is usually indicated when patients still have persistent or progressive symptoms despite 6 to 12 weeks of conservative treatments. Disc herniation is seen in 1:10,000 ratio in general population and among all the patients, 10% patients may require surgical intervention.
HNP was first treated by performing laminectomy to remove the offending disc material. Unfortunately, this method requires long rehabilitation time and high morbidity.3Therefore, various studies have been conducted for the past 20 years to looking for safer and less invasive techniques.4
Nowadays, conventional open microdiscectomy is still chosen as the first choiceof HNP treatment,5 despite its lack of sufficient evidence. However, with the development of modern microspinal surgical techniques, minimally invasive techniques have revolutionized the management of pathologic conditions of the spine such as lumbar disc herniation.6 Developmentin the design and use of optics as well as surgical instruments, induce the aplication off ullendo scopic surgical procedures, suchas themicro-end odiscectomy (MED).
The effectiveness of this technique is expected to be similar to the conventional procedures, but with shorter hospitalization and recovery time.Micro-endodiscectomy (MED) is a surgical technique with a very small incision size, only about 1 inch.Moreover, this procedure do not cut nor detach paraspinal muscle from its insertion. Therefore, with its less invasiveness, MED can reduces the injury of muscle and epidural.Since its introduction, several studies have proven that MED is a safe and less invasive surgical technique.7
One of the advantages of MED when compared to other procedures used in HNP treatment is the lack of tissue damage that occurs. Less tissue damage in this procedure could potentially lead to a lower intensity of post-surgical leg and back pain, faster rehabilitation and integration, and lower treatment costs.Neverthless, study describing the outcome, safety and factors influencing the efficacy of this treatment is still lacking, especially in Indonesia. In this study we describe and analyze the clinical outcome of patients who underwent MED for HNP.
Method
We performed prospective analysis of data of all patients who underwent MED for HNP between January 2015 until December 2016. There were 78 patients who underwent single-level end odiscectomy at L2-3, L3-4, L4-5, or L5-S1 levels for the first time during this period. Records of these patients were then reviewed to gain data including patients’ demographics (age, sex, height, weight, and body mass index), type of radiculopathy (level and side), VAS and ODI score before and after surgery, comorbid factors (diabetes, hypertension, smoking), operative time, estimated amount of blood loss, number of patients with intraoperative CSF leakage and neurological deficits, number of patients who need change to open procedures and repeated surgery, length of hospitalization and days of mobilization.Occupational activities were divided into the following 2 categories: light work (i.e., office jobs, household tasks), and heavy work (e.g., construction workers, farming, etc).8
Surgical Procedure
Preoperative preparation includes patient positioning, instrument preparation and sterilization. First, patient were given general anesthesia in the operating rooms. Patient was then turned onto prone position. After positioning the patient, a fluoroscope that was intended to be used during the remainder of the operation was prepared. After the fluoroscope ready, we create sterile fields by scrubbing patient’s back with sterile soap. Then drapes were placed appropriately, and surgery begins.
The fluoroscope was used to confirmed the disc space. Patients were given local anesthesia on the muscles surrounding the bone, and after it’s works, a half-to-one-inch incision was made. Through the incision, a thin wire was placed and lowered until it reached the bone. After that, some increasingly larger dilators are take down on top of one another following the wire. Therefore, the muscle was split instead of separated from the bone.
When the fourth or fifth dilator was placed, the muscle was stretched until it creates a nickel-sized opening.This opening was going to be the place in which the procedure was performed. The working channel will be positioned during the installation of the last dilator. Furthermore, a circular rectator mounted using a mechanical arm, will hold back the muscle so that the dilator can be removed.
Surgery was performed using an endoscope that will enlarge the projection of the base image of the working channel up to the TV screen. This instrument helps the surgeon to remove tissue and perform microscopic manipulations. However, this tool is only capable of giving monocular images, such as sight using one eye, so that depth perception will decrease.
A small amount of muscle that was exposed to bone or left in the lamina, was cleansed. Furthermore, the covering of the bone that covers the nerves is opened using a small drill with high speed or Kerrison ronguer. This was intended to make the nerves easier to move. After the bone cover was released, we would see a yellow ligament that protects the underlying nerve. The yellow ligaments were then separated and removed carefully, allowing thecal sac, which was where the nerve grouped, and exiting the nerve root. Then, the nerve and thecal sac were removed simultaneously after a very small rectator was placed on the outside of the nerve root, so the herniated disc was just at the bottom of the rectator.9
Furthermore, the disc was removed by making a small prick on the surrounding tissue. Sometimes discs are found that have been damaged or broken, so that the area around them need to be cleaned from the fractional disk. When finished, a small hole made will be closed by itself. Then the wound that was formed was irrigated with antibiotics. One or two stitches, usually added to hold the tissue and help the healing process. The wound was then closed using a loose bandage. Once the patient was conscious, the patient was transferred to the recovery room.9
Outcomes
Thisstudy outcomewere thescoresonVisual Analog Score (VAS) for assessing leg and back pain and Oswestry Disability Index (ODI) for assessing disability caused by back pain.10 The VAS for back and leg pain score range of 0, indicating no pain, until10 representing the worst pain in their back and leg.Meanwhile,ODI scores were rangedfrom 0, indicating no functional impairment, until 100,indicating maximum functional impairment. Assesment done at baseline and 12 weeks prospectively.The patient’s condition was monitored for 12 weeks after surgery. If there are signs of recurrent or persistent radiculopathy, a postoperative MRI was done to identify the presence of HNP recurrence.Additionally, operating time, complications, and the estimated amount of blood loss were evaluated.
Statistical Analyses
Demographic data were presented as means with standard deviations. Preand postoperative ODI and VAS scores were compared by using paired t-tests with a significant level of 0,05. All statistical analyses were performed by using SPSS version 24.0.
Results
There are 78 HNP patients undergoing MED during January 2015 – December 2016. The average age of our sample was 45.23 ± 13.73 years and 51 (65.4%) were male (Table 1). The mean body mass index of the patients was 24.9 ± 3.29kg/m2. Fifty seven patients (73.1%) complained about radicular pain before the operation and 21 (26.9%) complained about back pain with radicular pain. Most patients (57.7%) felt pain for more than 12 months.
Table 1: Sociodemographic, clinical, and radiological characteristic of the patients
| Characteristic | Value |
| Average age (years) | 45.23 ± 13.73 |
| Sex | |
| Male | 51 (65.4%) |
| Female | 27 (34.6%) |
| Mean Body Mass Index (kg/m2) | 24.9 ± 3.29 |
| Onset of pain (months) | |
| < 12 Months | 33 (42.3%) |
| > 12 Months | 45 (57.7%) |
| Symptom | |
| Back pain | 0 (0%) |
| Radicular pain | 57 (73,1%) |
| Back pain with radicular pain | 21 (26,9%) |
| Occupation | |
| Light | 56 (71.8%) |
| Heavy | 22 (28.2%) |
| Sport | 29 (37.2%) |
| Frequent (>3x/week) | 9 (11.5%) |
| Rare (<3x/week) | 20 (25.6%) |
| Position of Defecation | |
| Squat | 42 (53.8%) |
| Sit | 36 (46.2%) |
| HNP Level | |
| L2-3 | 0 (0%) |
| L3-4 | 2 (2,6%) |
| L4-5 | 44 (56.4%) |
| L5-S1 | 32 (41.0%) |
| HNP Location | |
| Central | 11 (14.1%) |
| Paracentral & Lateral recess | 43 (55.1%) |
| Foraminal | 24 (30.77%) |
| Far Lateral | 0 (0%) |
| Neurological Deficits | 1 (1.3%) |
| Paresthesia/tingling | 70 (89,7%) |
| Risk Factors (Comorbid) | |
| No Risk Factor | 49 (62.8%) |
| Diabetes | 0 (0%) |
| Hypertension | 9 (11.5%) |
| Smoking | 9 (11.5%) |
| Diabetes and Hypertension | 7 (8.9%) |
| DM, Hypertension, and Smoking | 4 (5.1%) |
One patient (1.3%) had neurological deficits and 70 (89,7%) complained about paresthesia or tingling. Forty nine patients (62.8%) had no comorbid factors for the operation. Patients who have light occupation were 56 (71.8%), while the other 22 (28.2%) patients have heavy occupation. Forty two patients (53.8%) performeddefecation in a squatting position and 36 (46.2%) in sitting position. Among 78 patients, only 29 (37.2%) patients doing sports. Themostusual vertebraelevelof HNP wasL4-5(56.4%), followedbyL5–S1 (41.0%) and L3–4(2.6%). The most common location of HNP in our study population was paracentral 43 (55.1%).
Themean durationofsurgerywas 60 ± 17.41 minutes with 48.49 ± 42.5 ml of blood loss. Most of the patients (88.5%) could perform mobilization within 1 day after surgery, and 47 (60.3%) patients could be discharge successfully within 3 days after surgery.Complicationsoccurredin5cases(6.4%), all cases were dural tear.Eleven patients (14.1%) had a recurrenceof pain and 8 (10.3%) amongs them occur within 12weeksafter operation. Three patients (3.8%) needed to undergo repeated surgery within 3 months at the same level. Nine patients (11.5%) had to performed convertion to open surgery (Table 2).
Table 2: Operative characteristics of the patients
| Characteristic | Value |
| Average Duration of Surgery (minutes) | 60 ± 17.41 |
| Blood Loss (ml) | 48.49 ± 42.5 |
| Complications | |
| No Complication | 73 (93.6) |
| Dural tear | 5 (6.4%) |
| Ankle/toe dorsiflexion weakness | 0 (0%) |
| Transient paresis | 0 (0%) |
| Day of Mobilization | |
| Within 1 day after surgery | 69 (88.5%) |
| > 1 day after surgery | 9 (11.5%) |
| Length of Stay | |
| Within 3 days after surgery | 47 (60.3%) |
| > 3 days | 31 (39.7%) |
| Recurrence of pain after operation | 11 (14.1%) |
| Onset of recurrence | |
| < 12 weeks | 8 (10.3%) |
| ≥ 12 weeks | 3 (3.8%) |
| Repeated Surgery | 3 (3.8%) |
| Within 12 weeks | 3 (3.8%) |
| After 12 weeks | 0 (0%) |
| At the same level | 3 (3.8%) |
| At diferent level | 0 (0%) |
| Convertion to Open Surgery | 9 (11.5%) |
The mean preoperative VAS and ODI score was 4.88 ± 1.10 and 35.21 ± 8.24 , whereas the mean postoperative score was 1.53 ± 1.14 and 5.16 ± 5.52, revealing statistically significant improvement (p<0.001) (Table 3).
Table 3. Clinical outcome of the treatment
| Characteristic | Value | p value |
| VAS score |
<0.001 |
|
| Before | 4.88 ± 1.10 | |
| After | 1.53 ± 1.14 | |
| ODI score |
<0.001 |
|
| Before | 35.21 ± 8.24 | |
| After | 5.16 ± 5.52 |
Discussion
Lumbar micro-endodiscectomy is one of the recognized spinal surgery procedures.11-13Unfortunately, this method is still not widely used by Indonesian orthopedic spinal surgeons in Indonesia.In addition, the advantages of this method when compared to routine methods are debatable. Some retrospective studies mention the success rate of this method by 90-98%,14,15 while the prospective study only mentions a success rate of 70-80%.16,17
One of the advantages of MED is only requires a minor surgery to be less invasive when compared with conventional methods. As a result, medical expenses can be reduced and the recovery time is shorter, so the patient will be able to move back to normal. Smaller incision created from MED makes less trauma to lumbar muscles. The use of this technique also has other several advantages, such as better lighting and magnification so as to better identify the neural structure for easier manipulation and faster post-operative mobilization. In addition, the duration of surgery using this technique is shorter with fewer bleeding, less intraoperative myoligamentous trauma and faster return to work time.18,19 This procedure also reduce the risks of post-surgery complications such as chronic nerve-root edemadevelopment of venous stasis.20
Some short-term and long-term research that has been done, supports our findings. Six months after surgery, 96% of thepatients treated by MED technique were healedfrom their root pain and 89% were healed from low back pain.20 Ourstudyshowedthatstatisticallysignificant difference in the relief of back disabilities and leg pain (Figure 1). The averageduration of surgery was less or more than 1 hour, and the recurrencerateofmultiple HNPsurgerywas3.8%within 3 months.Our results also show that the number of observed complications (6.4%) was lower than expected.No infection, thrombosis, or hemorrhage were found.The length of hospitalization in our study was 3 days overall, which was similar to other study in which the hospitalization duration was3-5 days.20 Hospitalization period longer than 3 days were typical in patients with dural tears and some medical conditions.
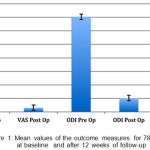 |
Figure 1: Mean values of the outcome measures for 78 patients at baselineand after 12 weeks of follow-up
|
Risk of recurrent symptoms after microdiscectomy in our study is 14.1%. This was the same result with other study that reported the percentage of recurrent symptoms risk between 5-12%, although the risk decreases with time post surgery.21,22
Several studies have examined the incidence of postoperative MED surgery. Overall, the incidence of re-surgery ranged from 7.5-8%, whereas the incidence in teenagers was higher than adults. Besides age, hernia type also affects the incident of re-operation. Patients with protrusion type herniation have higher incidences of re-surgery when compared with extrusion or sequestration types.Prevention of re-surgery is performed with a careful and thorough discectomy, especially in the posterior longitudinal ligament and decompression on the lateral recess.23,24In our study the re-operation rate was 3.8%, it is comparable with other study. With MED, specific complications like dural lesions and excessive bleeding are less frequent because of the better view got from the scope.
Several studies have found no significant difference in perioperative bleeding between MED and traditional surgery. There were also no significant differences in complication variables, length of hospitalization and end result over long term post-treatment. This leads to a decision of using microscope for operation or not submitted to the surgeon.25,26However, our study shows that the use of a microscope is very useful.
Our results also show that in patients with specific criteria, MED is an excellent choice for operative treatment of lumbar disc disc herniation, although both macro and micro-endodiscectomy methods are equally acceptable for treatmet disk herniation.
The use of MED during surgery, in addition to providing excellent illumination and magnification is also able to maintain three-dimensional vision (stereopsis).27-30However, MED also has several disadvantages, including poor perception of depth which causing dural tears incidence,26-28and the restricting confines of the tubular retractor will limits the ability of the surgeon inorientating thedecompression instruments.27,28,30
Several studies have shown that MED is able to reduce the operation time gradually.Research conducted by Perez-Cruet et al,29 reported a reduction in operating time gradually.In the first 30 cases, the average duration of surgery ranged from 110 minutes, while in the last 30 cases the duration of surgery was only 75 minutes. Based on our experience, the length of MED operation ranges from 60 ± 17.41 minutes. This result is lower when compared with previous studies. This difference caused operator that has been quite well experienced with this technique.
Not only does MED appear to be a safe and effective intervention for HNP, it also shows good clinical outcomes, although some complications such as dural tear and recurrency might occur.Despite its safety and good clinical outcomes, high quality randomized controlled trials are still required to study this procedure, especially studying its efficacy and cost effectiveness.
Acknowledgements
Authors are grateful for the supports from Faculty of Medicine, University of Lampung, Indonesia. This project was funded independently.
Conflict of Interest
There is no conflict of interest.
References
- Soliman J, Harvey A, Howes G, Seibly J, Dossey J and Nardone E. Limited microdiscectomy for lumbar disc herniation: a retrospective long-term outcome analysis. J Spinal Disord Tech 2014;27:8-13.
CrossRef - Jacobs W.C, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J. 2011;20:513–5
CrossRef - Gulati Y.Lumbar microdiscectomy. Apollo Medicine. 2004;1:29-32.
CrossRef - Fuentes S, Métellus P, Acosta-Diaz U, Pech-Gourg G, Dufour H, Grisoli F.Minimally invasive transmuscular approach for the treatment of lumbar far lateral disc herniation. Neurochirurgie. 2009;55:70-74.
CrossRef - Caspar W. A new surgical procedure for lumbar disk herniation causing less tissue damage through a microsurgical approach. Adv Neurosurg. 1977;4:74–77.
CrossRef - Toyone T, Tanaka T, Kato D and Kaneyama R. Low-back pain following surgery for lumbar disc herniation. A prospective study. J Bone Joint Surg Am 2004;86:893–6.
CrossRef - Garg B, Nagraja U.P and Jayaswal A:Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. Journal of Orthopaedic Surgery. 2011;19(1):30-4.
CrossRef - Loupasis G.A, Stamos K, Katonis PG, Sapkas G, Korres DS, Hartofilakidis G. Seven- to 20-year outcome of lumbar discectomy. Spine 1999;24:2313-2317.
CrossRef - Rothman R.H, Simeone F. Posterolateral endoscopic lumbar discectomy. In (Herkowitz H, Garfin S, Eismont F, Bell G and Balderston R). The Spine, 6th ed. Philadelphia: Elsevier Saunders, 2011;1041−50.
- Collins S.L, Moore R.A, McQuay H.J. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain 1997; 72:95–9
CrossRef - Wilson D.H, Harbaugh R. Microsurgical and standard removal of the protruded lumbar disc: A comparative study. Neurosurgery1981; 422-427.
CrossRef - Apostolides P.J, Jacobowitz R, Sonntag V. Lumbar discectomy microdiscectomy: the gold standard. Clin Neurosurg 1996;43:228-238.
- Williams R. Lumbar disc disease. Microdiscectomy. Neurosurg Clin N Am 1993; 4:101-108.
CrossRef - Gibson J.N, Grant I.C, Waddell G. Surgery for lumbar disc prolapse. Cochrane Database Syst Rev. 2000;3:13-20.
- Findlay G.F, Hall B.I, Musa B.S, Oliveira M.D, Fear S. A 10-year follow-up of the outcome of lumbar microdiscectomy. Spine. 1998; 23:1168-1171.
CrossRef - Clabeaux D.E, Hyland A. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg. 2002;96:34-44.
- Quigley M.R, Bost J, Maroon J.C, Elrifai A, Panahandeh M. Outcome after microdiscectomy: results of a prospective single institutional study. Surg Neurol. 1998; 49:263-267.
CrossRef - Lorish T.R, Tanabe C.T, Waller F.T, London M.R, Lansky D. Correlation between health outcome and length of hospital stay in lumbar microdiscectomy. Spine. 1998;23: 2195-2200.
CrossRef - Frizzell R.T, Hadley MN. Lumbar microdiscectomy with medial facetectomy. Techniques and analysis of results. Neurosurg Clin N Am. 1993;4:109-115.
CrossRef - McCulloch JA. Focus issue on lumbar disc herniation: macroand microdiscectomy. Spine. 1996;21:45-56.
CrossRef - Williams R.W. Microdiscectomy: a twelve year statistical review. Spine 1986;11:851-2.
CrossRef - Hirabayashi S, Kumano K, Ogawa Y, Aota Y, Maehiro S. Microdiscectomy and second operation for lumbar disc herniation. Spine. 1993;18:2206-2211.
CrossRef - Haglund MM, Moore A.J, Marsh H, Uttley D. Outcome after repeat lumbar microdiscectomy. Br J Neurosurg. 1995;9: 487-489.
CrossRef - Tullberg T, Isacson J, Weidenhielm L. Does microscopic removal of lumbar disc herniation lead to better results than the standard procedure? Results of a one-year randomized study. Spine. 1993;18:
- Mulholland R. Does microdiscectomy have any real advantage? Br J Hosp Med. 1991; 45:196-199.
- Brayda B.M, Cinnella P. Posterior endoscopic discectomy (and other procedures). Eur Spine J.2000;9:24–29.
CrossRef - Nakagawa H, Kamimura M, Uchiyama S et al., Micro endoscopic discectomy (MED) for lumbar disc prolapse. J Clin Neurosci, 2003;10:231–235.
CrossRef - Perez C.M.J, Foley K.T, Isaacs R. Micro endoscopic lumbar discectomy: technical note. Neurosurgery. 2002;51:129–136
- Righesso O, Falavigna A, Avanzi O. Comparison of open discectomy with micro endoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery. 2007;61:545–549.
CrossRef - Schizas C, Tsiridos E, Saksena J. Microendoscopic discectomy compared with standard microsurgical discectomy for treatment of uncontained or large contained disc herniations. Neurosurgery. 2005;57:357–360.








