Manuscript accepted on :February 23, 2018
Published online on: --
Plagiarism Check: Yes
Rajathilagam T1 , Malathy A. R2, Seethalakshmi S1 and Kothai G2
, Malathy A. R2, Seethalakshmi S1 and Kothai G2
1Department of Pharmacology, ESIC Medical College and PGIMSR, Chennai, Tamilnadu.
2Department of General Medicine, ESIC Medical College and PGIMSR, Chennai, Tamilnadu.
Corresponding Author E-mail: heartthrobe_kg@yahoo.co.in
DOI : https://dx.doi.org/10.13005/bpj/1387
Abstract
Patients who are admitted in ICU’s (Intensive Care Unit) are usually seriously ill, often suffer from multiple chronic illnesses and drug usage is also quite extensive. Due to resource restraints in providing quality healthcare in developing countries, drugs should be prescribed rationally in order to maximise benefit. Thus the ICU represents an important platform for conducting drug utilization studies. To evaluate the prescribing pattern in the medical I.C.U. of a tertiary care teaching hospital in Tamilnadu. A prospective cross sectional study was conducted among patients admitted to the medical ICU for a period of 6 months to establish the prescribing pattern. The collected data was analysed to estimate the WHO core drug prescribing indicators and patient indicators. The prescription data of 130 patients who met the study criteria was analysed. The mean age group of patients admitted was 54.95 ± 8.1 years and average duration of stay in the ICU was 5.5 ± 2.4 days. Cardiovascular (CVS) diseases was involved in the majority of the patients (41.5%, n = 54). Among parenteral drugs, 15 drugs (8 classes) acted on the CVS and 13 drugs (5 classes) were antibiotics while 25 drugs (7 classes) acted on the CVS and 11 drugs (6 classes) acted on the neurological system among oral drugs. Analysis of prescription records for drug utilization pattern in this study revealed that most of the drug classes were prescribed for appropriate indication & all drugs were prescribed as generics.
Keywords
Drug Utilisation; Medical ICU; Prescribing Pattern; Polypharmacy
Download this article as:| Copy the following to cite this article: Rajathilagam T, Malathy A. R, Seethalakshmi S, Kothai G. Prescription Pattern in A Medical Icu of A Tertiary Care Teaching Hospital of South India. Biomed Pharmacol J 2018;11(1). |
| Copy the following to cite this URL: Rajathilagam T, Malathy A. R, Seethalakshmi S, Kothai G. Prescription Pattern in A Medical Icu of A Tertiary Care Teaching Hospital of South India. Biomed Pharmacol J 2018;11(1). Available from: http://biomedpharmajournal.org/?p=19277 |
Introduction
The World Health Organization (WHO) defines drug utilization research as “the marketing, distribution, prescription and use of drugs in a society, with special emphasis on the resulting medical, social, and economic consequences”.1 Thus, inherent in the definition, such studies provide logical background for determining the rationality of drug use as well as providing evidence based guidance for making policy decisions at various levels of healthcare.2,3
The Medical ICU’s (Intensive Care Unit) represent an important platform for conducting drug utilization studies as patients are seriously ill and are often suffering from chronic critical illnesses.3 The Medical ICUs are also the epicenter of antimicrobial resistance which play an important problem influencing patient outcomes4. Incidence of poor treatment response and adverse reactions increase due to critical conditions of patients and use of multiple medications with altered pharmacokinetic and pharmacodynamic conditions.4
Multiple medications from a variety of pharmacological classes are prescribed to these patients and this significantly raises the health care costs and also patient morbidity and mortality.3,5 Due to availability of limited funds in developing countries, drugs should be prescribed rationally so that the available funds can be utilized optimally. Periodic evaluation of drug utilization in Medical ICUs is essential for enabling suitable modifications in prescribing patterns, optimization of health care system, proper use of resources and for making prescription policies.4 Drug utilization research studies conducted in the inpatient settings are effective tools that help in evaluating the drug prescribing trends, efficiency and cost effectiveness of hospital formularies.3 Hence this study was conducted to identify priority areas that need to be targeted for further improvement in patient care in Medical ICUs. The study aimed to evaluate the prescribing pattern in the Medical ICU of a tertiary level teaching hospital in Chennai.
Materials and Methods
After obtaining clearance from the Institutional Ethics Committee, the study was carried forward as a prospective observational cross sectional study for a study period of 6 months. All patients above 18 years of age who were admitted to the medical ICU were eligible to be enrolled in the study after satisfying inclusion and exclusion criteria. Patients whose duration of stay in the ICU was less than 24 hours were not included in the study. Patients who were found to be eligible were invited to take part in the study after providing written informed consent. Basic demographic details about the patients were obtained. Detailed information on the diagnosis, comorbid conditions, duration of stay were obtained. From the medical records, drugs used including name of the drug, dosage schedule (form, route, and frequency) and duration of treatment were obtained. The collected data was analysed to estimate the WHO core drug prescribing indicators and patient indicators.
Prescribing indicators that were noted included number of drugs per patient, proportion of parenteral and oral drugs, proportion of various drug classes and particular drugs used, proportion of drugs prescribed by generic names and proportion of fixed drug combinations. Patient indicators that were noted included indication for admission in ICU and organ systems involved, age in years of all patients, men to women ratio, duration of parenteral therapy and oral therapy.
Results
The prescription data of 130 patients was analysed. 60% of the patients were males and 40% were females. (Table 1). The mean age group of patients admitted was 54.95 ± 8.1 years and their age range varied from 22 – 93 years. (Figure 1). The average stay of patients in the medical ICU was 5.5 ± 2.4 days. The least duration of stay of a patient in the medical ICU was 3 days and the maximum duration was 43 days. (Figure 2)
 |
Figure 1: Age Distribution of the patients
|
 |
Figure 2: Duration of stay of the patients in ICU
|
Diabetes mellitus and Hypertension were the most common co morbid diseases followed by coronary artery disease. (Table 2) The most common system involvement for which patients were admitted in the ICU was the cardiovascular system (CVS) (41.53%, n = 54) followed by central nervous system (CNS) (22.3%, n = 29), respiratory system (13.1%, n= 17) and renal system (4.6%, n = 6). Infections and sepsis were the admitting diagnosis in 11 patients (8.46%). The remaining patients had other causes like malignancies, GIT diseases and poisoning. (Figure 3) Among cardiovascular diseases, acute coronary syndromes accounted for the majority of admissions followed by acute pulmonary edema. Among neurological diseases, metabolic encephalopathy and acute cerebrovascular accidents were the most common diagnoses for admission to ICU.
 |
Figure 3: Organ system involvement
|
Among the drugs administered by the parenteral route, 15 drugs (8 subclasses) acted on the CVS, 13 (5 subclasses) were antibiotics, 10 (5 subclasses) drugs were for CNS. Diuretics (Furosemide, Mannitol), anticoagulants (heparin), proton pump inhibitors (Pantoprazole), beta lactam antibiotics (Ceftriaxone, Amoxicillin + Clavulanic acid), Insulin & antiepileptics (Phenytoin, Levetiracetam) were the commonly prescribed drugs for parenteral administration. All these drugs were administered by intravenous route and the average duration of parenteral therapy was 5.63 ± 1.2 days. (Figure 4)
 |
Figure 4: Drug classes prescribed by route of administration
|
Among the drugs administered by the oral route, 25 drugs (7 subclasses) acted on the CVS, 11 drugs (6 subclasses) acted on the CNS, 5 drugs (3 subclasses) were antibiotics and 8 drugs were of other categories. The average duration of oral therapy was 5.42 ± 2.1 days. (Figure 4) Antihypertensives (ACE inhibitors, calcium channel blockers and beta blockers), hypolipidemic drugs (statins), antiplatelets (aspirin, clopidogrel), sedative hypnotics (benzodiazepines), laxatives & antibiotics (fluoroquinolones, tetracyclines and macrolides) were the commonly prescribed oral drugs. All these drugs were administered concomitantly or sequentially with parenteral therapy.
Table 1: Sex Distribution of the patients
| Sex | N=130 | Percentage |
| Males | 78 | 60% |
| Females | 52 | 40% |
Table 2: Comorbid disease conditions
| Comorbid diseases | Number of patients |
| Diabetes mellitus | 51 |
| Hypertension | 50 |
| Coronary artery disease | 43 |
| Chronic kidney disease | 19 |
| Hypothyroidism | 9 |
| COPD | 7 |
| Bronchial asthma | 3 |
| Malignancy | 3 |
| Rheumatic heart disease | 2 |
| Epilepsy | 1 |
| Cirrhosis | 1 |
The average number of drugs prescribed per patient was 11.8 ± 2.5 drugs.The most commonly prescribed fixed drug combinations (FDC) were amoxicillin with clavulanic acid, cefoperazone with sulbactam and anti-tuberculous drugs. The categories of antibiotics used is shown in Figure 5. The drugs were prescribed only by their generic name in all records.
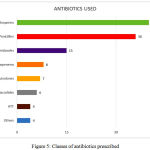 |
Figure 5: Classes of antibiotics prescribed
|
Discussion
This study analysed the prescription pattern of 130 patients admitted in the medical ICU over a period of 6 months. It showed male preponderance (60%) in sex distribution of patients which is similar to the previous studies3–5. The mean age (54.95 ± 8.1 years) of the patients included in this study was slightly higher and also the age range was wider when compared to the previous studies.3,4,6 This difference could be due to the cross sectional study design & geographic variation in disease occurrence. In this study, the admitted patients were kept in medical ICU for an average of 5.5 ± 2.4 days which is similar to the data reported Patel et al and Tavallaee et al.4,7 This indicates that the treatment durations are comparable.
In the study by Kaur et al, the most common target organ systems involved were CVS & CNS which was similar to the findings in the present study. The top diseases for the admission in medical ICU were acute coronary syndrome, acute cerebrovascular accidents, metabolic encephalopathy and acute pulmonary edema3. Diabetes mellitus and systemic hypertension were the most common comorbid conditions and this adds to the existing body of evidence that these diseases are assuming epidemic proportions in developing countries.
The average number of drugs prescribed per patient was 11.8 ± 2.5 drugs which is comparable with previous studies4, 8. Though it is polypharmacy, this cannot be considered irrational practice as there is need for empirical therapy till definitive diagnosis becomes clear and multiple drug usage is essential for management of acute life threatening conditions. Also, patients who are admitted to the ICU may have more than one disease and treating all of them effectively with multiple drugs can lead to better outcomes. Similar to previous studies, drugs acting on CVS were more frequently prescribed for both parenteral & oral routes.3,4,6,8,10
Conclusion
Analysis of case records for drug utilization pattern in this study revealed that most of the drug classes were prescribed for appropriate indication and that all drugs were prescribed as generics. Polypharmacy may be unavoidable in the treatment of patients admitted to the ICU.
Conflict of Interest
There is conflict of interest
References
- Sachdeva P. D., Patel B. .G. Drug utilization studies – Scope and future perspectives. Int J Pharm Biol Res. 2010;1:11‑7.
- WHO Collaborating Centre for Drug Statistics Methodology, Guidelines for ATC classification and DDD assignment 2013. Oslo, 2012. https://www.whocc.no/file archive/publications/1_2013guidelines.pdf. Accessed on January 2nd, 2018.
- Kaur S., Rajagopalan S., Kaur N., Shafiq N., Bhalla A., Pandhi P et al. Drug Utilization Study in Medical Emergency Unit of a Tertiary Care Hospital in North India. Emergency Medicine International. 2014;1-5.
CrossRef - Patel M. K., Barvaliya M. J., Patel T. K., Tripathi C. B. Drug utilization pattern in critical care unit in a tertiary care teaching hospital in India. International Journal of Critical Illness and Injury Science. 2013;3(4):250-5.
CrossRef - Pandiamunian J., Somasundaram G. A study on prescribing pattern of anti-microbial agents in the medical intensive care unit of a tertiary care teaching hospital in Puducherry union territory, South India. International Journal of Pharmacy and Pharmaceutical Sciences. 2014;6(3):235-8.
- Balushi A. K. A., Al‑Shibli S., Al‑Zakwani I. Drug utilization patterns in the emergency department: A retrospective study. Journal of Basic and Clinical Pharmacy. 2014;5(1):1-6.
CrossRef - Tavallaee M., Fahimi F., Kiani S. Drug‑use patterns in an intensive care unit of a hospital in Iran: An observational prospective study. Int J Pharm Pract. 2010;18:370‑6.
CrossRef - Barot P. A., Malhotra S. D., Rana D. A., Patel V. J., Patel K. P. Drug utilization in emergency medicine department at a tertiary care teaching hospital: A prospective study. Journal of Basic and Clinical Pharmacy. 2013;4(4):78-81.
CrossRef - Paudel R., Palaian S., Giri B., Hom K. C., Sah A. K., Poudel A., et al. Clinical profile and drug utilization pattern in an intensive care unit of a teaching hospital in Western Nepal. Arch Pharm Pract. 2011;2:163‑9.
- Biswal S., Mishra P., Malhotra S., Puri G. D., Pandhi P. Drug utilization pattern in the intensive care unit of a tertiary care hospital. J Clin Pharmacol. 2006;46:945‑51.
CrossRef







