Ketut Suryana1, Wayan Wita2, I. Gde Raka Widiana3, Ketut Suastika4 and I. Wayan Putu Sutirtaya5
1,3,4Department of Internal Medicine, University of Udayana, Bali.
2Department of Cardiology University of Udayana, Bali.
5Department of Clinical Pathology, Faculty of Medicine, University of Udayana, Bali.
Corresponding Author Email: ketutsuryana@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1225
Abstract
The progression of atherosclerosis in acute coronary syndrome (ACS) may depend on balance of inflammatory and anti-inflammatory cytokines. Aim of this study was to investigate association between low IL-10 plasma levels, high MMP-9, IL-6 / IL-10 plasma ratio and risk of cardiovascular events (CVE) in ACS patients.A prospective cohort study was conducted in Intensive Cardiac Care Unit of Sanglah Hospital in Denpasar. Seventy three ACS were selected consecutively, consisting of patients: 12 (16.4%) UAP patients, 11 (15.1%) NSTEMI patients and 50 (68.5%) STEMI patients. During the 6 months follow-up period, 14 (19.2%) patients had CVE; 10 (13.7%) patients with vascular deaths, 3 (4.1%) patients with IMA and 1 (1.4%) with recurrent cardiac ischemia. In Kaplan-Meier survival curve, showed that group with high plasma MMP-9 (median ≥ 23.4 pg/ml), high ratio of IL-6/IL-10 plasma levels (median ≥ 0.95) and low plasma IL-10 (median < 14.11 pg/ml) showed lower cumulative survival than controls. Patients with high plasmaMMP-9 hasashortersurvival by almost1month(27 days) than controls.Cox proportional model showed that high of plasma MMP-9(median ≥ 23.4 pg/ml) had significantassociation with CVE (RR = 6.6; p<0.05), meanwhile, dyslipidemia and hypertension also hadsignificantassociation with CVE (RR 0.2 and 4.1; p-value < 0.001 and 0.04, consecutively). Using path analysis, it was found that effect of IL-10 to CVE is through MMP-9. High MMP-9 mayan independentrisk factor of CVE in ACS.
Keywords
Acute Coronary Syndrome; Cardiovascular eventsInflammatory forces;
Download this article as:| Copy the following to cite this article: Suryana K, Wita W, Widiana I. G. R, Suastika K, Sutirtaya I. W. P. Low II-10 Plasma Levels, High II-6 / II-10 Ratio and Matrix Metalloproteinase-9 (Mmp-9) Associated With High Cardiovascular Events in Acute Coronary Syndrome. Biomed Pharmacol J 2017;10(3). |
| Copy the following to cite this URL: Suryana K, Wita W, Widiana I. G. R, Suastika K, Sutirtaya I. W. P. Low II-10 Plasma Levels, High II-6 / II-10 Ratio and Matrix Metalloproteinase-9 (Mmp-9) Associated With High Cardiovascular Events in Acute Coronary Syndrome. Biomed Pharmacol J 2017;10(3). Available from: http://biomedpharmajournal.org/?p=16367 |
Introduction
Acute Coronary Syndrome (ACS) is a clinical manifestation of coronary atherosclerosis and plaques rupture, followed by thrombus formation in coronary arteries.1-3ACS includesunstable angina (UA), non-ST elevation myocardial infarction (NSTEMI), STelevationmyocardial infarction (STEMI).Despite changes in lifestyle and the use of new pharmacologic approaches, cardiovascular disease continues to be the principal cause of death in the US, Europe and much of Asia. During last decade it was reported that mortality rate of UA is 5-10%, and AMI is 10-20%.2-4,6
Inflammation is a significant component both in progression of atherosclerosis and in the acute thrombotic event in ACS. Recent attention has been focused on the potential role of circulating biomarkers of inflammation such as IL-6 (pro-inflammatory cytokines), IL-10 (anti-inflammatory cytokines),MMP-9(endopeptidasesenzymes) which are shown as predictors or prognostic factors. Vascular risk in ACS leads to cardiovascular events which can be predicted by the balance between pro-inflammatory and anti-inflammatory cytokines or the balance between pro-inflammatory and anti-inflammatory forces. IL-6 is a pro-inflammatory cytokine in ACS.The ratio of pro-inflammatory cytokine (IL-6) to anti-inflammatory cytokine (IL-10) may reflect the intensity of occult plaque inflammation & the vulnerability to rupture. Pro-inflammatory to anti-inflammatory cytokine ratios also acts as a signal of balance between pro-inflammatoryand anti-inflammatory forces, and may predict vascular risk in ACS.3,5,7-9
Matrix metalloproteinases (MMPs) are a group of endopeptidases with capacity to cleave components of extracellular matrix (collagen & elastin).6-10 Xu et al. (2004) has conducted a study in 40 patients with ACS (including 17 with AMI, 23 with UAP).11 It was reported that MMP-9 level are significantly higher in AMI than in UAP. Funayama et al. (2004) has conducted a similar study which recruit 36 myocardial infarction patients. It was reported thatplasma IL-6 concentrations and MMP-9 in the peripheral vein, ascending aorta and infarct-related coronary artery were all significantly greater than in the control subjects.12 Malarstig et al. (2008) has reported that IL-10 reflects a pro-inflammatory state in patients with ACS. This findings are in contrast result with some previous reports which revealed IL-10 as an anti-inflammatory.4,10
The aim of this study was to answer questionwhetherlow plasma levels of IL-10, high ratio of IL-6 / IL-10 plasma levels and high plasma levels of matrix metalloproteinase-9 (MMP-9) is associated with high cardiovascular events in ACS.
Patients and Methods
Patients
This study was performed during January 2012 to January 2013among 73 ACS patients consisted 59 men, 14 women, aged 57.38 (SD 10.95) years included 12 (16.4%) UAP patients, 11 (15.1%) NSTEMI patients and 50 (68.5%) STEMI patients. All of the patients were admitted in the Intensive Cardiac Care Unit of Sanglah Hospital of Denpasar. The ACS diagnostic criteria isbased on American Heart Association (AHA), American College of Cardiology (ACC), 2007 ACC/AHA 2007. Exclusion criteria were; the patients with CABG and/or history of cardiac intervention, rheumatic heart diseases, acute and chronic hepatitis, chronic kidney disease defined as creatinine clearance using CockroftGault formula less than 60 ml/1.73 m2/minutes), infectious diseases, and malignancy.Patients were classified based on positivity of prognostic factor (low IL-10, high IL-6 / IL-10 ratio and high MMP-9 plasma levels) and negativity of prognostic factor (high IL-10, low IL-6/IL-10 ratio and low MMP-9 plasma levels using median values as cut-off values.
Follow up
The patients were follow-up for the end point during the 6 months. The primary end point of the study is cardiovascular events (CVE) which were defined as combination of vascular death, AMI, stroke and recurrent cardiac ischemia. All of the patients were treated with the standard treatment using AHA guidelines. The study was approved by the Ethics committee of Medical Faculty of Udayana University / Sanglah Hospital, and all patients have given written informed consent to participate.
Statistical Analysis
Descriptive test was performed to describe the data of patientscharacteristics. Kolmogorov-Smirnov test was used to test the data distribution. Non parametric test was used to determine the median values of dependent variables. Bivariate analysis was used to determine thecorelation between dependent variables (low IL-10 plasma levels, high MMP-9 and IL-6/IL-10 ratio) and CVE in ACS. Kaplan-Meier survival curve and log rank test to describe the time to event between the group with prognostic factors (IL-10, IL-6/IL-10 ratio and MMP-9) plasma level ≥ median and < median values to cardiovascular events. Cox proportional model to determine odds Ratio (OR) low IL-10 plasma levels, high IL-6 / IL-10 plasma ratio and high MMP-9 plasma levels to cardiovascular events were used. Path analysis was sued to determine the role of MMP-9 variable to the independent variable (IL-6, IL-10) to outcome. Significant level was set on probability (p-value) less than 5%. Statistical software package SPSS 15.0was used for statistical analysis.
Results
Table 1 showed baseline characteristics of thedemographic data,the classicalrisk factors, cardiac biochemicalmarkers, ACS clinical manifestation and cardiovascular events.
Table 1: Characteristic of demographic, traditional risk factors, and cardiac biomarkers, ACS manifestations and cardiovascular events.
| Variable | Mean ± SD or N (%) |
| Age (years) | 57,38 ± 10,95 |
| Male / Female (%) | 59 (80,8%) / 14 (19,2%) |
| Hypertension (%) | 40 (54,8%) |
| Dyslipidemia (%) | 65 (89,0%) |
| LDL-cholesterol (mg/dl) | 131,6 ± 44,8 |
| Total Cholesterol (mg/dl) | 196,8 ± 48,8 |
| Trigliceride (mg/dl) | 140,5 ± 82,0 |
| HDL-cholesterol (mg/dl) | 39,8 ± 10,1 |
| Diabetes Mellitus(%) | 12 (16,4%) |
| Smoking (%) | 38 (52,1%) |
| Obesity (%) | 40 (54,8%) |
| CK-MB | 18,07 ± 16,48 |
| Troponin | 650,63 ± 806,36 |
| IL-6 | 50,2 ± 95,1 |
| IL-10 | 29,2 ± 50,5 |
| MMP-9 | 22,1 ± 4,9 |
| IL-6/IL-10 ratio | 1,9 ±2,7 |
| Clinical Features of ACS :
1. UAP |
12 (16,4 %) |
| 2. NSTEMI | 11 (15,1 %) |
| 3. STEMI | 50 (68,5%) |
| Cardiovascular Event (CVE) | 14 (19,2%) |
| 1. Vascular detah | 10 (13,7%) |
| 2. IMA | 3 (4,1%) |
| 3.Reccurent Cardiac Ischemia | 1 (1,4%) |
Distribution ofoutcome during 6 months of follow-up among patients with ACS (UAP, NSTEMI and STEMI) in this study was presented in Table 2. It was found that the incidence CV during 6 months period was 14 (19.2%).
Tabel 2: Clinical manifestations of ACS and cardiovascular events
| Clinical manifestations of ACS | Total numberof CVE (%) | Distribution of CVE |
| UAP | 1 (1.4%) | Reccurent cardiac ischemia1(1.4%) |
| NSTEMI | 0 | None |
| STEMI | 13 (17.8 %) | Vascular death
10 (13.7 %); AMI3 (4.1%) |
Based on Kolmogorov-Smirnov normality test, the data were not normally distributed, so that cut-off point was determinedusing median values of eachvariable,which were presented inthe following (Table 3)
Table 3: Median values of independent variables
| Variables | Median |
| IL-10 (pg/ml)
MMP-9 (pg/ml) IL-6/IL-10 ratio |
14.10
23.40 0.95 |
Therelationship between dependent variables including low plasma IL-10 levels (lower than median), high MMP-9 (higher than median) and high IL-6/IL-10 ratio (high than median) and CVE in ACS can be seen in Table 4. It was shown that there were no significant relationship between those variables in total population (UAP- NSTEMI-STEMI) also others sub-group (UAP-NSTEMI, NSTEMI-STEMI), however, there was significant relationship between MMP-9 and CVE in ACS in sub-group (UAP-STEMI).
Table 4: Relationship between independent variables (IL-10, MMP-9, IL-6/IL-10 Ratio) and dependent variable (cardiovascular events) in Sub-group (UAP and STEMI)
| Independent variables | Outcome | RR | CI95% | p | |
| CVE(-) | CVE(+) | ||||
| IL-10 < 14,10 (pg/ml) | 24 | 4 | 0,4 | 0,11-1,45 | 0,15 |
| IL-10 ≥ 14,10 (pg/ml) | 24 | 10 | |||
| MMP-9 ≥ 23,40 (pg/ml) | 19 | 10 | 3,8 | 1,04-13,94 | 0,03 |
| MMP-9 < 23,40 (pg/ml) | 29 | 4 | |||
| IL-6/IL-10 ≥ 0,95 | 25 | 8 | 1,2 | 0,37-4.08 | 0.74 |
| IL-6/IL-10 < 0,95 | 23 | 6 | |||
Kaplan-Meier survival curve of ACSpatients with low IL-10 plasma and high IL-10 to CVE and time event was shown in Figure 1. It was revealed thatpatients with low IL-10 plasma levels tend to have lower mean survival than those with high IL-10, although no significant difference found (142,2±111,14 days vs 162.03±8,53 day; p log-rank = 0,11)
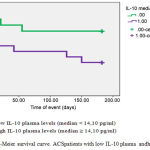 |
Figure 1: Kaplan-Meier survival curve. ACSpatients with low IL-10 plasma andhigh IL-10
|
It was also found that cummulative survival of ACSpatients with high MMP-9 plasma tend to be lower than those with low MMP-9 plasma to CVE and timeevent(138.68±111.73 daysvs 165.11±7.57days; p log-rank = 0.09), see Figure 2.
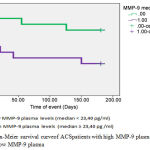 |
Figure 2: Kaplan-Meier survival curveof ACSpatients with high MMP-9 plasma and those with low MMP-9 plasma
|
It was also found that Survival of ACSpatients with high IL-6/IL-10 plasma tend to have lower survival time than those with low IL-6/IL-10 plasma to CVE and time event (147.70± 10.72 days vs 155.83 ± 9.51 days); p log-rank = 0.59), which can be seen in
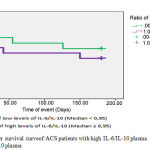 |
Figure 3: Kaplan-Meier survival curveof ACS patients with high IL-6/IL-10 plasma and with low IL-6/IL-10 plasma
|
Cox proportional model was used to assess multivariate relationship between independent variable (IL-10, IL-6 / IL-10 ratio and MMP-9) and the high CVE, controlling by traditional risk factors (age, dyslipidemia, diabetes, hypertension, obesity and smoking). There was a trend toward a strong relationship between low IL-10 plasma levels and CVE after controlling for traditional risk factors (OR 0.3, 95%CI 0.08 to 1.07;p=0.06), however, there was a strong relationshipbetweenhigh MMP-9 plasma levels and CVE (OR 6.6; 95% CI 1.66 to 25.95;p=0.00). On the other hand, there was a strong relationship between hypertension and dyslipidemia on CVE (OR 4.1; 95%CI 1.05 to 16.32), p = 0.04; OR 0.2; 95%CI 0,04-0, 60;p = 0.00 for hypertension and dyslipidemia, consecutively).
Table 5: Multivariate analysis of independent and traditional risk factors, and cardiovascular events
| Sig. | OR | CI 95.0% Exp (B) | ||
| Under | Above | |||
| Age | 0.28 | 0.5 | 0.12 | 1.83 |
| Hypertension | 0.04 | 4.1 | 1.05 | 16.32 |
| Dyslipidemia | 0.00 | 0.2 | 0.04 | 0.60 |
| Diabetes | 0.08 | 3.6 | 0.85 | 15.58 |
| Obese | 0.23 | 2.1 | 0.61 | 7.23 |
| Smoking | 0.49 | 0.6 | 0.18 | 2.29 |
| Low plasma IL 10 | 0.06 | 0.3 | 0.08 | 1.07 |
| High plasma MMP 9 | 0.00 | 6.6 | 1.66 | 25.95 |
| IL-6/IL-10 ratio | 0.70 | 1.3 | 0.30 | 5.62 |
Discussion
Basic pathomechanisms of acute coronary syndrome is an inflammation, which continues to imbalance between O2 supply and demand causing chest pain. Anatomical changes that occur between the three different clinical features: at UAP coronary vasospasm occurs (dynamic and progressive mechanic obstruction) and can also be followed by the formation of thrombus. While the IMA (NSTEMI and STEMI) occurring is partial obstruction in NSTEMI and STEMI total obstruction. Inflammatory markers in ACS is IL-6, IL-10 and MMP-9.1,4,8-13 The effect of classical risk factors to CVE in acute coronary syndrome can be confounded by levels of IL-10, IL-6 / IL-10 ratio and MMP-9. ACS may be caused by coronary vasospasm, atheromatous plaque rupture with various inflammatory mediators. Previous study has reported an increase in pro-inflammatory cytokines (IL-6, IL-1β, TNF-α, MMP-9) and decreased of anti-inflammatory cytokines (IL-10) in ACS. The inflammatory forces (the balance between pro-inflammatory and anti-inflammatory cytokines) may reflect the vulnerability to rupture and may predict vascular risk in ACS.1,14
The classical risk factors play a role in the pathogenesis of atherosclerosis as an initiator of endothelial dysfunction. Endothelial dysfunction is a precursor of the inflammatory processes underlying atherosclerosis. Progression of atherosclerosis, coronary vasospasm, plaque rupture and acute thrombotic event depends on the forces and the inflammatory activity of the enzyme degradation (MMP-9). Inflammatory forces constitute ratio of pro-inflammatory cytokines (IL-6, MMP-9) with anti-inflammatory cytokines (IL-10).5 Malarstiget al (2008) has reported different finding which showed that IL-10 acts as a pro-inflammatory cytokine in the ACS. 9,14-17
In this study, in both the total population and sub-groups itwas found that the low plasma levels of IL-10 did not prove to be an independent risk factor for CVE in ACS, but in ACS patients with CVE, IL-10 plasma below the median value and in patients who did not experience events ACSit was found that IL-10 plasma levels were above the median value. While previous study (Heeschenet al, 2003); reported that IL-10 levels more than 2.5 pg/ml are associated with a lower risk of cardiac observation for 6 months (HR: 0.38; 95% CI = 0.19 to 0.83 p = 0.00). A different report has shown by Malarstiget al (2008) that in a 12-month cohort study involving 3179 patients and 393 volunteers which showed that median values of IL-10: 0.8 (0,5-1,0) pg / ml in volunteers and 1.1 (0, 7 to 1.9) pg / ml in patients (p <0.001), consecutively. Patients with elevated levels of plasma IL-10 predicts increased risk of death and/or myocardial infarction with the highest risk in the 4th quartile with adjusted odds ratio 1.7 (95% CI 1.2 to 2.3).4,7,8,18-20
Activity of MMP-9 in the progression of atherosclerosis in ACS is to facilitate the migration of vascular smooth muscle cells into the intima vascular wall, limit the volume of plaque to degrade the extracellular matrix in the intima. The ability of MMPs to degrade the extracellular matrix and fibrous cup plaque rupture is a predisposing factor.5-8,19-21 This study showed thatamong sub-groups with APTS and STEMI it was found that the high levels of MMP-9 associated with significantly increased risk for CVE in ACS (P <0.05). While Brown et al. (1995) reported that MMP-9 is generally found in atherotomy specimens from patients with coronary plaque rupture. Likewise Kai et al, 1998 which has reported that the levels of plasma MMP-9 increased significantly in the coronary circulation of patients with AMI and UAP.10,21-25
New concept is now developed to explain balance between pro-inflammatory and anti-inflammatory cytokines. This balance can describe the intensity of inflammation in plaque atheromatous, ruptured plaque vulnerability, the vascular risk (the risk of vasospasm and ruptured) on progression of ACS.3,26 Data relating to the role of long-term prognostic factor of the ratio of pro-inflammatory cytokines with anti-inflammatory cytokines in ACS is still limited. In this study, observation of 6 months does not prove high IL-6 / IL-10 plasma ratio as a risk factors of CVE in ACS. However, previous studyshowed that high IL-6 / IL-10 as a risk factor for CVE in ACS after 6 months observation (p = 0.01) and the 1-year observation (p = 0.007).5,26-28
To illustrate relationship of the prognostic factors with CVE in ACS using Kaplan-Meier survival curves.Figure 1. shows that the cumulative survival rate was lower in the group with low IL-10 plasma levels than the group of high IL-10 plasma levels (73.7% vs 88.6%) with a mean survival between the two groups was not significant (142.2 ± 11.14 vs162.03 ± 8.53 days) log rank p = 0.11. While Kilic T et al (2006), reported that the group of patients with ACS (NSTEMI) who experienced CVE tend to have lower IL-10 plasma levelscompared with ACS (NSTEMI) patients who did not experience the CVE have higher IL-10 plasma levels ( 5.6vs 8.7pg/ml, p = 0.08). It was thought that IL-10 is atheroprotective / anti-inflammatory.
Figure 2. shows that the cumulative survival rate was lower in the group with high MMP-9 plasma levels than the group with lower MMP-9 plasma levels (73.0% vs 88.9%) with similar survival between the two groups was not significant (138.68 ± 11.73 vs 165.11 ± 7.57 days, log rank p = 0.09). While previous study Blankenberg S et al, 2003 reported that: MMP-9 plasma levels of CHD patients who experienced fatal CVE / vascular death was significantly higher than CHD patients who did not experience fatal CVE / vascular death (62.2 vs 47.8 pg / ml, p <0.0001).8,10,26-29
Figure 3. shows that the cumulative survival rate was lower in the group with high IL-6 / IL-10 plasma levels ratio than the group of low IL-6/IL-10 plasma levels ratio (78.4% vs 83.3%) with similar survival rate between the two groups (147.70 ± 10.72 vs 155.83 ± 9.51 days, log rank p = 0.59). HoweverKilic T et al. (2006), reported that the ACS (NSTEMI) patients whohad CVE has a higher IL-6 / IL-10 ratio(1.44vs0.75, p = 0.01) than ACS (NSTEMI) patients groups who did not experience CVE.
Cox proportional hazard model showed that after adjusted by control variables, such as age, hypertension, dyslipidemia, diabetes, obesity and smoking, it was shown that low IL-10 plasma levels tend to associate with lower risk ofCVE risk in ACS patients (RR: 0.3; 95%CI: 0.08 to 1.07; p = 0.06). Another study by Kilicet al (2006) also found similar results, that IL-10 plasma levels in ACS patients (NSTEMI) did not differ significantly between the group with and without experiencing CVE(p = 0.08). Also, after adjusted by the same control variables, it was found that high MMP-9 plasma levels associated with higher CVE risk factor in ACS patients (RR: 6.6; 95%CI: 1.66 to 25.95, p = 0,00). Another study by Kai et al., 1998; found that levels of MMP-9 and MMP-2 in circulation increased significantly in patients with AMI and UAP. Inokuboet al., 2001; reported that MMP-9 plasma levels in patients with ACS increased 2-3 fold compared to the normal subjects. While, after adjusted by the same control variables, it was found that high of IL-6 / IL-10 plasma ratio did not revealed to be a CVE risk factor in patients with ACS (p = 0.70). While Kilicet al (2006), reported that during 6 months observations, IL-6/IL-10 plasma ratio was significantly higher in patients with ACS (NSTEMI) who are CVE compared with ACS patients (NSTEMI) who are not experiencing CVE (p = 0.01) and after 1-year observation with a (p = 0.007).
This is a study includes all types of ACS clinical features (UAP, NSTEMI and STEMI) which may explain that in ACS patients with CVE, MMP-9 plasma levels were high. MMP-9 collagenase activity degrades the collagen component of plaques atheromatous and basal endothelial membrane that results in plaque rupture atheromatus. Atheromatus plaque rupture is the basic of CVE pathogenesis. Thus meanhigh MMP-9 plasma levels is a strong risk factor for the occurrence of CVE in ACS patients.
On the other hand also found that the group with low IL-10 plasma levels, high MMP-9 and IL-6/IL-10 plasma ratio indicates cumulative survival is shorter compared to the high IL-10 plasma levels, low MMP- 9 and IL-6 / IL-10 plasma ratio. Thus, subgroups of patients with ACS who undergo CVE (UAP and STEMI) showed inflammatory picture with proinflammatory activitiesforce greater than the ACS sub-group who did not experience CVE.
Limitation of the study is that up to now,there is no standard cut-off point of inflammatory markers of IL-10, IL-6 and MMP-9. In this study, because the data are not normally distributed the cut-off point areset by median value. While other researchers such as Heeschen, et al (2003) in a cohort study set a cut-off point of IL-10 levels are set based on ROC analysis.Kilicet al (2006) on the 6 months cohort observational to 1 year in 80 patients with NSTEMI, the cut-off point, was also defined by ROC analysis. Alwiet al (2007) in a cross-sectional study in RSCM Jakarta, PersahabatanHospital, MMC Hospital and Medistra Hospital involving 62 patients with CHD (out patients) and 84 patients with ACS, the cut-off point of IL-6 levels were set based on the average. Malarstig et al (2008) at 1-year cohort study involving 3.179 patients with ACS and 39 volunteers, cut off point IL-10 plasma levels are set based on the median value.
Conclusions
High MMP-9 plasma levels was associated with almost 7 times increased risk of CVE in ACS patients.ACS patients with CVE risk factors (low IL-10 plasma levels or high MMP-9 or high IL-6/IL-10 plasma ratio) showed shorter survival rate than the ACS group without CVE risk factors (high IL-10 plasma levels or low MMP-9 or low IL-6/IL-10 plasma ratio). The high MMP-9 plasma levels has a shorter survival rate, almost 1 month (27 days) compared with low MMP-9 plasma levels. In addition, hypertension anddyslipidemiaare also shown to be a CVE risk factor in ACS patients.
Acknowledgment
Authors of the current article take this opportunity to thanks to patients who warmly co-operated in this research program. This research was financially by KetutSuryana, MD. PhD
Conflict of Interests
The authors declare that there is no conflict of interest regarding the publication of this paper.
Funding Source
by Ketut Suryana, MD. PhD (Private).
References
- Ozben B and Erdogan O. The Role of Inflammation and Allergy in Acute Coronary Syndromes. Inflammation & Allergy – Drug Targest. 2008;7:136-144.
CrossRef - Buffon A., Biasucci L. M., Liuzzo G., D’onofrio G., Crea F and Maseri A. Widespread coronary inflammation in unstable angina. N Eng J Med. 2002;347:5-12.
CrossRef - Avanzas P., Espliguero A., Sales J. C., Aldama G., Pizzi C., Quiles P and Kaski J. C. Markers of inflammation and multiple complex stenoses (pancoronary plaque vulnerability) in patients with non-ST segment elevation acute coronary syndromes. Heart. 2004;90:847-852.
CrossRef - Malarstig A., Eriksson P., Hamsten A., Lindahl B., Wallentin L and Siegbahn A. Raised interleukin-10 is an indicator of poor outcome and enhanced systemic inflammation in patients with acute coronary syndrome. Heart. 2008;94:742-729.
CrossRef - Prasad A., Mathew V., Holmes D. R., Gersh B. J. Current management of non-ST-segment-elevation acute coronary syndrome reconciling the results of randomized controlled trials. European Heart Journal. 2003;24:1544-1553.
CrossRef - Anwar T. B. Dislpidemiasebagai faktorresi kopenya kitjantung koroner. E-USU Repository; Universitas Sumatera Utara. 2004;1-10.
- Hansson G. K. Inflammation, Atherosclerosis abd Coronary Artery Disease. N Engl J Med. 2005;352:1685-95.
CrossRef - Rodriguez A., Gonzales P. A and Kaski J. C. Inflammatory Systemic Bomarkers in Setting Acute Coronary Syncromes Effects of the Diurnal Variation. Current Drug Targets. 2009;10:1001-1008.
CrossRef - Ross R. Atherosclerosis-An Inflammation Disease. N Eng J Med. 1999;340:115-126.
CrossRef - Killic T., Ural D., Ural E., Yumuk Z., Agacdiken A., Sahin T. Relation between proinflammtory to anti-inflammatory cytokine ratios and long-term prognosis in patients with non-ST elevation acute coronary syndrome. Heart. 2006;92:1041-1046.
CrossRef - Xu Z., Zhao S., Zhou H., Ye H and Li J. Atorvastatin Lowers Plasma Matrix Metalloproteinase-9 in Patients With Acute Coronary Syndrome. Clinical Chemistry. 2004;4:750-753.
CrossRef - Funayama H., Ishikawa S. E.,Kubo N., Katayama T., Yasu T., Saito M., Kawakami M. Increases in Interleukin-6 and Matrix Metalloproteinase-9 in the Infarct-Related Coronary Artery of Acute Myocardial Infarction. Circ J. 2004;68:451-454.
CrossRef - Libby P and Theroux P. Patho physiology of Coronary Artery Disease. Circulation. 2005;111:3481-3488.
CrossRef - Welsh P., Whincup P. H., Papacosta O., Wannamethee S. G., Lennon L., Thomson A. Serum matrix metalloproteinase-9 and coronary heart disease a prospective study in middle-aged men. Q J Med. 2008;101:785-791.
CrossRef - Girndt M and Kohler . Interleukin-10 (IL-10) an update on its relevance for cardiovascular risk. Nephrol Dial Transplant. 2003;18:1976-1979.
CrossRef - Moe K. T and Wong T. Current Trends in Diagnostic Biomarkers of Acute Coronary Syndrome. Ann Acad Med Singapore. 201;39:210-5.
CrossRef - Smith D. A., Irving S. D., Shledon J., Cole D and Kaski J. C. Serum Levels of the Antiinflammatory Cytokine Interleukin-10 Are Decreased in Patients With Unstable Angina. Circulation. 2001;104:746-749.
CrossRef - Tedgui A and Mallat Z. Anti-inflammtory Mechanisms in the Vascular Wall. Circ. Res. 2001;88:87-887.
CrossRef - Tedgui A and Mallat Z. Cytokines in Atherosclerosis Pathogenic and Regulatory Pathways. Physiol Rev. 2006;86:515-581.
CrossRef - Kleemann R., Zadellar S and Kooistra T. Cytokine and atherosclerosis a comprehensive review of studies in mice. Cardiovascular Reasearch. 79:360-376.
- Heeschen C., Dimmeler S., Hamm C. W., Fichtscherer S., Boersma E., Simmons M. L. Serum level of the Antiinflammatory Cytokine Interleukin-10 Is an Important Prognostic Determinant in Patients With Acute Coronary Syndrome. Circulation. 2003;107:1-6.
CrossRef - Jones C. B., Sane D. C., Herrington D. M. Matric metalloproteinases: A review of their structure and role in acute coronary syndrome. Caradiovascular Research. 2003;59:812-823.
CrossRef - Apple F. S., Wu A. H. B., Mair J., Ravkilde J., Panteghini M., Tate J. Future Biomarkers for Detection of Ischemia and Risk Stratification in Acute Coronary Syndrome. Clinical Chemistry. 2005;51;1-15.
- Agewall S. Matrix metalloproteinase and cardiovascular disease. European Heart Journal. 2006;27:121-122.
CrossRef - Kelly D., Cockerill G., Ng L. L., Thompson M., Khan S., Samani N. J and Squire B. Plasma matrix metalloproteinase-9 and left ventricular remodeling after acute myocardial infarction in man a prospective cohort study. European Heart Journal. 2007;28:711-718.
CrossRef - Garvin P., Nilsson L., Carstensen J., Jonasson L and Kristenson M. Circulating Matrix Metalloproteinase-9 Is Associated with Cardiovascular Risk Factors in a Middle-Aged Normal Population. Plos ONE. 2008,3:1-7.
- Brown. Identification of 92-kD Gelatinase in Human Coronary Atherosclerotic Lesions. C. 1995;91:2125-2131.
CrossRef - Kai H., Ikeda H., Yasukawa H., Kai M.,Seki Y. Peripheral blood levels of matrix metalloproteases-2 and -9 are elevated in patients with acute coronary syndromes. J Am Coll Cardiol. 1998;32:368-72.
CrossRef - Gori A. M., Cesari F., Marcucci R., Giusti B., Paniccia R., Antonucci E. The balance between pro and anti inflammatory cytokines is associated with platelet aggregability in acute coronary syndrome patients. Atherosclerosis. 2009;202:255-262.
CrossRef








