Mikhail Valerevich Sinitsyn, Evgeny Mikhailovich Belilovskiy, Lydia Bulatovna Ayusheeva and Armine Sergeevna Galstyan
Moscow Scientific and Clinical Center for TB Control, Moscow, Russian Federation.
Corresponding Author E-mail: msinitsyn@mail.ru
DOI : https://dx.doi.org/10.13005/bpj/1238
Abstract
This research evaluates the effect of human immunodeficiency virus (HIV) prevalence on the tuberculosis (TB) epidemiology in a megalopolis. A comparative analysis for TB patients, co-infected and not co-infected with HIV has been done using registry data of the TB monitoring system for Moscow for 2014-2015. It has been shown that permanent city residents aged from 31 to 40, unemployed and injection drug users are more common among TB patients co-infected with HIV vs. the rest of TB patients. Numbers of those infected with TB and dying of HIV amount to a third of total fatal cases associated with TB, as compared to those dying of TB. Thus, a significant contribution of HIV disease to key figures and dynamics must be recognized, when assessing the TB epidemiology.
Keywords
Tuberculosis; HIV Disease; Co-infection; Tuberculosis (TB); Tuberculosis (TB) and HIV Co-infection; Tuberculosis (TB) Epidemiology
Download this article as:| Copy the following to cite this article: Sinitsyn M. V, Belilovskiy E. M, Ayusheeva L. B, Galstyan A. S. HIV Prevalence Among TB Patients in Moscow. Biomed Pharmacol J 2017;10(3). |
| Copy the following to cite this URL: Sinitsyn M. V, Belilovskiy E. M, Ayusheeva L. B, Galstyan A. S. HIV Prevalence Among TB Patients in Moscow. Biomed Pharmacol J 2017;10(3). Available from: http://biomedpharmajournal.org/?p=15824 |
Introduction
Tuberculosis (TB) epidemiology remains challenging globally, despite vigorous efforts of international medical and public organizations.1 Country-wide spread of HIV disease is the major reason why TB control measures do not produce the desired effect. The World Health Organization (WHO) announced TB and HIV disease to be inter-related globally destructing problems that require immediate attention.1,2 Currently, a clear trend persists in the RF towards improving of basic epidemiological indicators of TB.3 Any further flourishing of the favorable situation is held back by the spread of HIV disease. Rising HIV incidence rates are registered in the majority of the RF regions, and on account of advanced HIV patients. The number of TB patients co-infected with HIV (HIV/TB patients) and their portion among TB patients also increase. A gradual improvement of TB situation has been observed for many years now in Moscow, and reduction of epidemiological indicators gained pace for the last few years. The capital city is currently among most successful subjects in the country. TB incidence and mortality rates in the city have been approaching those in developed European countries and equaled to 28.0 and 2.6 cases per 100,000 population, accordingly, in 2015 vs. cross-national values of 57.7 and 9.2 per 100,000 population. Moscow does not rank highest in terms of the public being affected by HIV; however, it is among 20 subjects of the RF, where this problem is extremely acute, which naturally impacts the epidemiological situation of TB in the city.3-5 The authors are interested in studying the effect HIV disease has on TB epidemiology against current significant reduction in TB rates. This research deals with analysis of HIV prevalence among TB patients in the city of Moscow and its effect on the social and demographic structure of newly diagnosed TB patients, registered TB patients, and mortality rates of TB patients across the city.
Objective of the Research
was to study the effect HIV disease has on the structure of basic epidemiological indicators of TB in the region against favorable TB prevalence.
Materials and Methods
This research involved comparative assessment of the composition of newly diagnosed TB patients and TB patients registered at the Budgetary Public Health Facility ‘Moscow Municipal Research and Practice Tuberculosis Control Center within the Moscow Healthcare Department’ (hereinafter – the Center), based on data from state statistical observation report forms No. 33, No. 8 and No.61, and individual registers of the Moscow tuberculosis monitoring system (MTMS). For this analysis, 6,545 of newly diagnosed TB patients with HIV positive and HIV negative status (newly diagnosed TB/HIV+ and newly diagnosed TB/HIV-) were reviewed according to the registry of newly diagnosed TB patients and TB patients registered in 2014-2015, including 1,309 HIV/TB cases, which were collected from the MTMS registries, covering both permanent and temporary residents of the city. Analysis of HIV co-infection was done in newly diagnosed TB patients according to their status of stay on the territory of Moscow, i.e. for permanent city residents, homeless people, those coming from other RF subjects, and foreign nationals. Records of 709 co-infected patients that are registered at the Center were reviewed, using data form the MTMS and forms No. 33 collected separately at the Center in 2015 for HIV/TB patients. The mortality structure of TB patients dying of HIV disease (B20.0) was assessed, using information from mortality monitoring registries of the MTMS at the Center for TB patient dying of TB and HIV disease (B20.0) for 2012-2015. Mortality monitoring registries comprised data by ‘death foci’ of TB or HIV disease, details about all fatal cases occurring on the territory of the city within a certain period of time, regardless of the RF subject or reporting period, where and when the death record will be filed. Therefore, registry data differ slightly from statistic numbers of deaths published by the Mosgorstat (the territorial body of Federal service of national statistics for the city of Moscow).6 Statistical analysis was done, using Epi-Info 7.1.4.0 software. Statistical confidence was assumed at 95%, unless any other value was indicated.
Results
Newly Diagnosed TB Patients and HIV Disease
HIV disease prevalence among newly diagnosed TB patients in the city of Moscow based on data from state statistical observation forms.
The number of HIV patients that are registered at the Moscow Municipal AIDS Center (AIDS MMC) is on the rise. According to form No. 61, the increment of growth is over 1,000 people p.a. They numbered to 28,678 before 2015 year end, of which 9,386 had clinical manifestation of secondary infections (stages 4А, 4B, 4C and 5).4 To the contrary, the number of newly diagnosed TB patients co-infected with HIV started to drop. The decline has been observed among permanent residents of the city since 2013, from 414 in 2012 down to 319 in 2015. Reduction of the portion of such patients from 20.3% (2014) down to 18.6% has been observed for the first time in 2015 (see Figure 1). Overall, according to the MTMS, the portion of newly diagnosed TB/HIV+ patients was 15.9% for all TB patients, newly diagnosed in 2014-2015, including permanent residents and migrant and homeless patients (17.4% and 14.4% or 565 and 474 patients in 2014 and 2015, respectively).
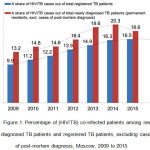 |
Figure 1: Percentage of (HIV/TB) co-infected patients among newly diagnosed TB patients and registered TB patients, excluding cases of post-mortem diagnosis, Moscow, 2009 to 2015.
|
HIV Disease Among Newly Diagnosed TB Patients
Among 628 newly diagnosed TB patients co-infected with HIV in 2014-2015 that were recorded appropriately, 1.9% were at stage 4A of HIV disease, 40.9% at stage 4B and 57.0% at stage 4C. Taking into account form No. 61, which records the number of HIV patients that were registered at the Center in 2014-2015, TB incidence among the patients at above stages of the disease was, accordingly, 135.7% (95% CI: 70.1 – 236.9), 4,787 and 8,485 per 100,000 HIV patients in the corresponding stage. A half of newly diagnosed patients co-infected with HIV had their CD4+ count below 200 cells/uL, and below 350 cells/uL with 72.3% of patients (see Figure 2).
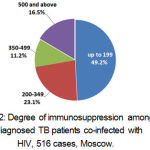 |
Figure 2: Degree of immunosuppression among newly diagnosed TB patients co-infected with HIV, 516 cases, Moscow.
|
Prevalence of Newly Diagnosed TB Co-Infected With HIV Among Various Categories of Moscow Residents According to Their Status of Stay on the Territory of the City
The study of this registry showed that permanent residents of the capital megalopolis constituted the vast majority of newly diagnosed TB/HIV+ patients in 2014-2015, i.e. 69.3% or 720 patients out of 1,039 patients. Accordingly, over a third of TB/HIV+ patients represented temporary residents – 30.7% (319 patients), of which 18.5% (192) came from other RF subjects, 8.0% (83) were homeless, 4.1% (43) were from post-Soviet countries, and one patient came from Vietnam. The majority of 192 newly diagnosed TB/HIV+ patients that came from other RF subjects were residents of the Moscow region (13.5% or 26 people). The percentage of HIV/TB patients was 23.4% among newly diagnosed patients that came from this RF subject (95% CI 15.9% – 32.4%). Also, a great portion of newly diagnosed TB/HIV+ patents was observed among newly diagnosed TB patients that came from the Saratov region: 10 out of 30 or 33.3% (17.3% – 52.8%), the Orenburg region: 9 out of 32 or 28.1% (13.7% – 46.7%), and the Kemerov region: 7 out of 12 or 58.3% (27.7% – 84.8%). With a great number of newly diagnosed TB patients that came from Dagestan, the portion of newly diagnosed TB/HIV+ patients was just 8 out of 132 or 6.1% (2.7% to 11.6%). Ukraine nationals contributed most to newly diagnosed TB/HIV+ cases among post-Soviet countries, i.e. 39.5% (17 people out of 43). The percentage of co-infected patients was 11.9% (7.1% to 18.4%) among TB patients of this nation that were newly diagnosed in Moscow. According to MTMS data, temporary residents affect greatly the epidemiological situation in Moscow. This effect mosty applies to TB patients that are not co-infected with HIV. Thus, among 6,545 newly diagnosed TB patients in 2014-2015, temporary residents constituted 43.5% (2,845 people), among 5,506 newly diagnosed TB/HIV- individuals they constituted 45.9% (2,526 people) and among 1,039 newly diagnosed TB/HIV+ individuals they constituted significantly less – merely 30.7% (319 people), p<0.01. Nevertheless, the stay status impacted greatly the newly diagnosed TB/HIV+ portion among newly diagnosed TB patients (Table 1).
Table 1: A portion of HIV/TB patients among newly diagnosed TB patients, 2014-2015, Moscow
| Population group | Number of newly diagnosed TB patients | ||
| total | of which TB/HIV+ patients | [%] | |
| Total, including | 6,545 | 1,039 | 15.9 |
| Permanent residents | 3,700 | 720 | 19.5 |
| Temporary residents | 2,845 | 319 | 11.2 |
| of which | |||
| Individuals coming from other RF subject | 1,266 | 192 | 15.2 |
| Homeless individuals | 484 | 83 | 17.2 |
| Foreign nationals | 1,095 | 44 | 4.0 |
| including nationals from the post-Soviet countries | 977 | 43 | 4.1 |
This number is significantly higher for patients that are permanent residents of the city (19.5%) vs. other patients in total (11.2%, p<0.01), and for patients that come from other RF subjects (15.2%, p<0.01), and that are foreign nationals (4.0%, p<0.01). The only case with no significant difference were homeless patients (17.2%, p>0.05).
Sex-Age Structural Features of Newly Diagnosed Patients Subject to HIV Exposure
Newly diagnosed TB patients that fell into the category of permanent residents were characterized by a significantly higher TB/HIV+ fraction among males vs. females (2014-2015), i.e. 21.9% and 15.7%, accordingly (p< 0.01). There were not any such differences observed among permanent residents and TB/HIV+ share amounted to 11.9% and 9.8% for males and females, accordingly (Table 2). The distribution of permanent residents by age for TB/HIV+ and TB/HIV- patients varies widely (Figure 3). Specific peak of maximum number of TB/HIV+ cases in the age range of 31 to 40 years can be observed among males, as well as females, i.e. 68.7% and 58.8% of the cases, accordingly. The odds of any patient being TB/HIV+ and belonging to this age group were 7.5 times higher in 2014-2015 (95% CI 6.3 -8.9), as compared to TB/HIV- patients. The HIV disease fraction in these ages among TB patients reaches 43.9% (50% in males and 37% in females). Sex and age differences were not so obvious for TB/HIV+ and TB/HIV- patients among those coming from other RF subjects, foreign nationals or homeless people. Against rather apparent maximum for the TB/HIV- group, which is in the age group of 26 to 30 years, maximum for the TB/HIV- group fell within 31 to 35 years, similar to permanent residents. The portion of patients being 31 to 40 years in age was 52.7% in this group of patients. Thus, the odds of any newly diagnosed TB/HIV+ patient that is a temporary resident falling within this age group are 2.6 times higher (95% CI 2.0 -303) than among TB/HIV patients. The HIV disease fraction among newly diagnosed patients reaches 43.9% in the chosen group aged 31 to 40 years for permanent residents and 18.2% with migrant population and homeless people (Figure 4). Thus, the age and sex structure of TB patients depends largely on whether such patient is TB/HIV+ or not. Maximum number of affected males that are permanent residents is made up for the most part of patients with HIV/TB co-infection, the fact, which is not true for cases of the disease among temporary residents of the city. The analysis showed that presence of HIF infection for permanent residents of Moscow has a controlling influence on the overall correlation between the number of newly diagnosed TB patients and patient’s age and sex.
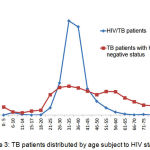 |
Figure 3: TB patients distributed by age subject to HIV status.
|
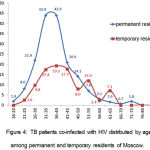 |
Figure 4: TB patients co-infected with HIV distributed by age among permanent and temporary residents of Moscow.
|
Social and Professional Structure of Newly Diagnosed Patients Subject to HIV Exposure
Certain specifics were discovered, when studying the social and professional structure of newly diagnosed TB patients with view to their HIV status. Thus, almost a third of unemployed permanent residents, newly diagnosed with TB, had a HIV co-infection (31.6%) and the number was significantly lower among employed HIV/TB patients (14.0%) (p<0.01). With regard to permanent residents, the co-infection was observed merely in 13.7% of unemployed individuals and 10.6% with employed individuals. The share of HIV/TB co-infected patients was predictively high among newly diagnosed TB patients, who are injection drug users, i.e. 75.6%, which determines a high odd ratio (OR) of HIV disease present for this category of permanent residents: OR = 13.9 (95% CI 8.4-23.2). A large portion of TB patients co-infected with HIV was observed among formerly imprisoned permanent residents: 46.5%, OR = 3.8 (2.4-6.2). Homeless patients were analyzed separately, and higher prevalence of HIV disease was observed among females rather than males falling into this population group, i.e. 24.8% and 15.0%, accordingly (p<0.05), which is presumably linked to their sexual behavior. At the same time, the group age of 31 to 40 years did not differ by a larger portion of co-infected patients, as was the case with other population groups, which is due to the specifics of HIV infecting homeless people. Details of HIV prevalence among various strata in the capital city are given in Table 2.
Table 2: Prevalence of TB co-infected with HIV among patients of various social and economic and demographic strata. 2013-2014
| Social and professional and demographic factors in patient’s profile | Among TBHIV- | Among TBHIV+ | TB/HIV+ share | TBHIV+ odd ratio with the factor present or absent (95% СI) |
p | |||
| abs. value | [%] | abs. value | [%] | with the factor present | with the factor absent | |||
| Permanent residents | ||||||||
| Total | 3,700 | 100.0 | 720 | 100.0 | 19.5 | – | – | |
| Males (vs. females) | 1,769 | 59.4 | 495 | 68.8 | 21.9 | 15.7 | 1.5 (1.3-1.8) | <0.0001 |
| 31 to 40 years of age | 601 | 20.2 | 471 | 65.4 | 43.9 | 9.5 | 7.15 (6.3-8.9) | <0.0001 |
| Unemployed | 1,126 | 37.8 | 519 | 72.1 | 31.6 | 9.8 | 4.3 (3.6-5.1) | <0.0001 |
| Employed | 907 | 30.4 | 148 | 20.6 | 14.0 | 21.6 | 0.6 (0.5-0.7) | <0.0001 |
| Psychoactive drug users | 20 | 0.7 | 62 | 8.6 | 75.6 | 18.2 | 13.9 (8.4-23.2) | <0.0001 |
| Formerly imprisoned | 38 | 1.3 | 33 | 4.6 | 46.5 | 18.9 | 3.8 (2.4-6.2) | <0.0001 |
| Temporary residents | ||||||||
| 2,526 | 2,526 | 100 | 319 | 100 | 11.2 | – | – | |
| Males (vs. females) | 1,637 | 64.8 | 222 | 69.6 | 11.9 | 9.8 | – | > 0.05 |
| 31 to 40 years of age | 753 | 29.8 | 168 | 52.7 | 18.2 | 7.8 | 2.6 (2.1-3.3) | <0.0001 |
| Unemployed | 1,611 | 63.8 | 256 | 80.3 | 13.7 | 6.4 | 2.3 (1.7-3.1) | <0.0001 |
| Retired | 84 | 3.3 | 4 | 1.3 | 4.5 | 11.4 | 0.4 (0.13-0.99) | <0.05 |
| out of which homeless | ||||||||
| Total | 401 | 100 | 83 | 100 | 17.1 | – | – | |
| Males (vs. females) | 322 | 80.3 | 57 | 68.7 | 15.0 | 24.8 | 0.5 (0.3-0.9) | <0.05 |
| 31 to 40 years of age | 135 | 33.7 | 36 | 43.4 | 21.1 | 15.0 | – | > 0.05 |
| Unemployed | 324 | 80.8 | 77 | 92.8 | 19.2 | 7.2 | 3.0 (1.3-7.3) | <0.01 |
HIV Disease Among TB Patients Registered In the City of Moscow
Along with newly diagnosed patients, a drop in the number of TB patients co-infected with HIV disease and registered in the city of Moscow (at institutions and divisions of the Center) and their percentage of total registered patients has been observed for the last years (see Figure 1). Starting from 2013, annual decrease in the number of such patients from 891 (2012) down to 709 (2015) has been observed. This is due to the dramatic drop in total number of registered TB patients. Thus, the portion of HIV co-infected patients has not started its decline yet, but has practically stopped its growth and stabilized at 16.3% to 16.5% (see Figure 1). Among HIV/TB patients that were registered in 2015, according to data of the MTMS registry, 40.0% are at the age of 25 to 34 and another 48.7% are at the age of 35 to 44. In terms of social and professional composition, registered HIV/TB patients are unemployed for the most part, despite their economically active age – 73.0%, and another 21.1% of the patients have a job. Almost a fifth (19.0%) of the patients were referred to the 2nd registration group of chronic TB patients. 70.8% of the analyzed patients were newly diagnosed and registered in 2014-2015.
Mortality Rates in TB Patient Dying of HIV Disease
It was shown before that advanced HIV cases prevail in Moscow among TB patients co-infected with HIV. Thus, any deaths of HIV/TB in the city that are associated with TB are caused exclusively by B20.0 (death of HIV disease resulting in mycobacterial infection), whereas deaths of tuberculosis (А15-А20) are not registered. A gradual fall in the number of TB patients dying of HIV disease has been observed for the last three years, i.e. from 288 (2012) down to 193 (2015). The number of deaths caused by B20.0 among permanent residents increased from 162 to 175 over 2012-2014, but decreased to 129 fatal cases in 2015. Numbers of those infected with TB and dying of HIV amounted to 37-42% of total fatal cases associated with TB in 2012-2015, as compared to those dying of TB. Therefore, this annual drop in the number of HIV deaths (B20.0 per ICD-10), along with the decrease in TB mortality rates (A15 to A19 per ICD-10) is a reflection of improved efficiency of TB patient management in Moscow.
Discussion
Epidemiological situation of HIV/TB co-infection is characterized by the ongoing HIV disease prevalence in the city, on the one hand, and significant reduction of new TB cases registered in HIV patients, on the other hand. The above changes are happening against an annual increase in the number of HIV affected people that were examined for TB. At the same time, a decrease in the absolute number of HIV patients getting TB and the portion of newly diagnosed HIV/TB patients has been observed, starting from 2015. This trend is especially evident in the last two years. Our research data showed that HIV/TB prevalence differs markedly in different social and economic and demographic strata of the city population, including age and sex. We may assume with a greater probability that HIV/TB co-infection affects males, 31 to 40 years old, unemployed and permanent residents, psychoactive drug users and former prisoners. This applies to a lesser degree to female permanent residents.7 These relations are not so apparent for temporary residents; however, they characterize in any case the specifics of HIV prevalence in different population groups. Research data also point to the significant effect HIV co-infection has on basic epidemiological indicators of TB, and primarily on incidence rates and the composition of newly diagnosed TB patients. It was shown before that every fifth newly diagnosed TB patient out of permanent residents of Moscow was also co-infected with HIV (TB/HIV co-infection) in 2014-2015. The effect of HIV disease on the age composition of newly diagnosed patients is especially evident. Among permanent residents, ca. 70% of males and 60% of females TB/HIV+ are at the age of 31 to 40, while this fraction is merely 19-21 % for both sexes among those that are TB/HIV-. Almost every second male in the above age range, who was registered as a TB patient, was also co-infected with HIV. The difference is not so great for patients coming from other cities or homeless people; however, the patterns still apply. Thus, information about the contribution of HIV co-infection must be covered in any analysis of changes of the age composition of disease incidence on a certain territory. For example, predicted and alerting shift of incidence maximum to younger ages (from 36-40 to 31-35 years), which was observed in 2015, was linked to the decreased number of co-infected patients mostly at the age of 36 to 40. Overall, the co-infection slows down the process of TB aging and may prevent indicator maximum from shifting to an older age group. Against overall weakened direct influence of the penitentiary system on TB incidence across the country for the last years,3 the ever rising indirect pressure on the epidemiological situation is exerted by HIV prevalence at correctional facilities, and, accordingly, increasing the number of the co-infected among former prisoners. In 2014-2015, the share of formerly imprisoned TB patients co-infected with HIV was 46.5%. According to data collected in Moscow, last few years were marked by the trend towards a drop in the number of registered HIV/TB patients and growth cessation of the portion of such patients among overall TB population. It should be pointed out that the number of TB patients who died of B20.0 currently makes up a third of all cases resulting in death. According to data taken from form No.33, out of total 399 deaths of TB patients who died of various causes in the city in 2015, 35.6% of cases were caused by TB (А15-А19 per ICD-10), 31.3% by HIV disease (B20.0), and the rest 33.1% were of other causes. Therefore, mortality rates caused by B20.0 affect significantly the overall effectiveness of dispensary management of TB patients and such rates dropping in the last years is a positive factor, which reflects the success of TB control measures taken in the city of Moscow.
Conclusion
Based on data collected in the city of Moscow, the number and portion of newly diagnosed TB and HIV co-infection cases impact greatly the figures and characteristics that describe TB prevalence. It was shown that temporary residents of the city contribute much less to the incidence of TB and HIV co-infection vs. TB alone (no co-infection). A great portion of young people of productive age and newly diagnosed with TB constitute those that are HIV-infected. Unemployed city residents suffer more frequently from HIV/TB co-infection, and the co-infection is more readily registered among psychoactive drug users and former prisoners. The improvement of epidemiological situation of TB and HIV co-infection in the city of Moscow, which has been observed for the last two years, indicates adequate and effective measures aiming at TB prevalence reduction in the capital city. The decreased number of newly diagnosed TB patients co-infected with HIV, and decreased mortality rates of such patients can be linked to active measures taken by the municipal TB task force under the umbrella of the Moscow Healthcare Department. Major efforts were directed to increase coverage of HIV patients with TB preventive chemotherapy, early diagnosis of TB in the public engaged in catering and manufacturing workplace foci of TB infection, application of most effective TB treatment regimen, introduction of the latest high-tech treatment approaches, and medical aid optimization. The authors believe that TB control in HIV patients in the region and outcomes may be considered an overall performance indicator of the task force, since these figures allow for assessing outcomes of managing the most vulnerable TB risk groups.
Conflict of Interest
The authors declare no conflict of interest.
The study was approved by the Moscow Scientific Society of Phthisiatricians and was included in the comprehensive science topics of the Moscow Center for Tuberculosis Control.
Acknowledgements
The authors are grateful to the Chairman of the Moscow Scientific Society of Phthisiatricians, the Director of the Moscow Center for Tuberculosis Control, Professor, MD-PhD Elena Bogorodskaya for assistance in research organization and Professor, MD-PhD Sergei Borisov who took part in the discussion of scientific results and editing.
The authors also express their gratitude to their colleagues working at the Moscow Center for Tuberculosis Control and the Moscow AIDS Center for valuable research recommendations and assistance in collecting information and evaluating the results: Professor, MD-PhD Petr Seltsovsky; Professor, MD-PhD Elena Kochetkova, Professor, MD-PhD Alexei Mazus, Professor, MD-PhD Elena Tsyganova; Candidate of Science (Medicine) Egor Serebryakov; Evgenia Kotova; Candidate of Science (Medicine) Olga Chizhova; Marina Levchenko; Lyudmila Kolpakova; MD-PhD Valeria Makieva.
References
- Global tuberculosis report 2015. Geneva: World Health Organization. 2015. http://www.who.int/tb/publications/ru/
- Fact Sheet. Global Statistics-2015. 2016. http://www.unaids.org/sites/default/files/media_asset/20150901_FactSheet_2015_en.pdf
- Tuberculosis in the Russian Federation, 2012/2013/2014. Analytical review of statistic indicators that are used in the Russian Federation and globally. Moscow. 2015.
- Bohorodskaya., Ye M., Litvinov V. I. (Eds.) Addressing the TB in Moscow. 2014 Analytical review of TB statistics. Moscow: MNPTsBT. 2015.
- Bohorodskaya., Ye M., Litvinov V. I. (Eds.) Addressing the TB in Moscow. 2015 Analytical review of TB statistics. Moscow: MNPTsBT. 2016.
- Bohorodskaya., Ye M. Belilovskiy., Ye M., Borisov S. E. et al. Monitoring TB fatalities in Moscow. Tuberculosis and Socially Sensitive Diseases. 2016;1:3-19.
- Bohorodskaya., Ye M., Borisov S. E., Sinitsyn M.V. et al. The effect HIV disease has on the structure of TB prevalence in a megalopolis. Tuberculosis and Socially Sensitive Diseases. 2016;3:3-20.







