Srikanth G1, Komal S2, Jyotsna R1 and Kalyana C. P.3
1Department of Oral and Maxillofacial surgery, Manipal College of Dental Sciences, Manipal university, Manipal.
2Department of Oral Medicine and Radiology, Manipal College of Dental Sciences, Manipal university, Manipal.
3Department of Public Health Dentistry, Manipal College of Dental Sciences, Manipal university, Manipal.
Corresponding Author: E-mail: komalmds1@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1198
Abstract
Formation of bilateral buccal sterile abscess following intralesional corticosteroid injection for the management of oral submucous fibrosis (OSMF) has not been reported in the literature. The main aim of this case report is to highlight the unusual complication of intralesional steroid in the form of abscess formation in a patient with oral submucous fibrosis Patient was a diagnosed case of OSMF, with restricted mouth opening and burning sensation in the oral cavity. He received intralesional betamethasone injection (4mg/ml) in buccal mucosa biweekly at a private dental clinic. Two weeks after commencement of the treatment, he developed pain along with swelling in relation to bilateral cheek region. The condition worsened after the third week(6 injections). An ultrasound scan was done which suggested the presence of an abscess. Following aspiration, incision and drainage was done, and empirical antibiotic therapy was initiated. The pus aspirated during the surgical procedure was sent for culture but did not show the presence of any organism, prompting a diagnosis of a sterile abscess. The patient recovered well without any further recurrence. Although steroids are most popular and frequently used drug used for the treatment of OSMF, however, it is important to keep in mind that it is a “double-edged sword”. When used in proper dosage at regular intervals, it will give excellent beneficial results, but a clinician must be aware of its rare complication as manifested in this case. Intralesional steroid injection is one of the commonly used modalities for the symptomatic relief of burning in OSMF. Hence, awareness of any complications associated with the same, whether common or rare, is essential for the early identification and management.
Keywords
Abscess; intralesional steroid; Oral submucous fibrosis.
Download this article as:| Copy the following to cite this article: Srikanth G, Komal S, Jyotsna R, Kalyana C. P. Unusual Complication of Intralesional Corticosteroid in Oral Submucous Fibrosis Patient. Biomed Pharmacol J 2017;10(2). |
| Copy the following to cite this URL: Srikanth G, Komal S, Jyotsna R, Kalyana C. P. Unusual Complication of Intralesional Corticosteroid in Oral Submucous Fibrosis Patient. Biomed Pharmacol J 2017;10(2). Available from: http://biomedpharmajournal.org/?p=15368 |
Background
Space infection is not an uncommon phenomenon in the orofacial region. The most prevalent causes being dental caries and its sequelae, infected root stumps, peri-coronal infection etc., if left untreated subsequently results in space infection of the respective area. Primary spaces first get involved, most frequent being buccal space. Occasionally presence of oral mucosal lesions such as oral submucous fibrosis (OSMF) as reported here, alters the presentation of the space infection. Oral submucous fibrosis is a chronic, progressive, potentially malignant oral disorder which results in rigidity and stiffness of the oral mucosa with loss of tissue mobility and eventual inability to open the mouth.1 Various treatment modalities are being used for the management of OSMF, which include either medical and surgical management or a combination of both. An enormous number of medications are being employed in the treatment of this disease. Nevertheless, no single medication could control the signs and symptoms in all the patients. Intralesional steroid injection is one of the modalities for the symptomatic relief of burning and may also be combined with hyaluronidase and placental extract intralesional injections to improve mouth opening.2
The main aim of this case report is to highlight the unusual complication of intralesional steroid in the form of abscess formation in a patient with oral submucous fibrosis. This is the first case reported in the literature, where bilateral buccal space infection developed following steroid injection, given for the symptomatic treatment of burning sensation in a 22-year young patient suffering from oral submucous fibrosis.
Case Description
A 22-year-old otherwise healthy male, with a habit of chewing gutkha for past three years, presented with pain and swelling in the bilateral cheek region of two weeks duration(Fig1). The pain was dull, aching and continuous in nature, which posed difficulty in chewing. His past dental history revealed that he had reduced mouth opening since six months and burning sensation in oral cavity while eating hot and spicy food. He had consulted with a private dental clinic for the same complaint and was diagnosed with oral submucous fibrosis. He was advised intralesional steroid injections (Betamethasone 4mg/ml) which were given twice weekly for two weeks on the bilateral buccal mucosa. Following which, he developed swelling associated with dull, aching continuous pain.
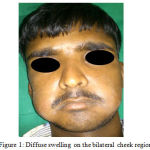 |
Figure 1: Diffuse swelling on the bilateral cheek region
|
Extraoral examination revealed a diffuse swelling on the bilateral cheek region measuring 4X4.5cm in dimension with obliteration of nasolabial fold. The swelling was soft, fluctuant and compressible, associated with tenderness. Mouth opening was reduced with interincisal distance measuring 13mm(Fig2) due to oral submucous fibrosis. Intraoral examination exhibited blanching of bilateral buccal mucosa(Fig3) and soft palate with shrunken uvula. Fibrous bands on the bilateral buccal mucosa and in the circumoral region were palpable. Movements of the tongue were restricted.
 |
Figure 2: Restricted mouth opening-13 mm
|
 |
Figure 3: Blanching of bilateral buccal mucosa and soft palate
|
Hard tissue examination exhibited full complement of teeth in the maxillary and mandibular arch. Routine radiographic examination by taking orthopantomogram and vitality test of all the teeth ruled out any odontogenic cause for the swelling. Correlating history, clinical and radiographic examination, a provisional diagnosis of bilateral buccal space infection due to intralesional corticosteroid injections in buccal mucosa was hypothesized. To confirm the diagnosis, ultrasonography of the bilateral cheek area was done using a 7.5MHz linear transducer which disclosed large anechoic, lobulated region with peripheral increased vascularity in the bilateral buccal space measuring 5x2x4 cm on the left and 5.5×2.5 x4.4cm on right side of the cheeks(Fig4). The area demonstrated ‘squish sign’ on compression suggestive of an abscess. Hence abscess in bilateral buccal space was considered as a final diagnosis. CT is the gold standard for soft tissue infection but due to its high cost, time taking scanning procedure and radiation hazards, ultrasound has emerged as the next most suitable and cost-effective imaging modality.
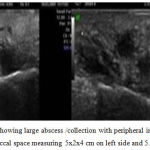 |
Figure 4: USG cheek showing large abscess /collection with peripheral increased vascularity seen in the bilateral buccal space measuring 5x2x4 cm on left side and 5.5×2.5 x4.4cm on right
|
With aseptic precautions, aspiration of the swelling was carried out intraorally for decompression under local anesthesia(Fig5). Thereafter intraoral incision was given in bilateral buccal mucosa and the abscess was drained. The patient was empirically recommended antibiotic amoxicillin in combination with clavulanic acid (625 mg) and metronidazole (400mg). The pus was sent for a culture which had no growth of microorganisms even after 72 hours. The extraoral swelling completely resolved within one week and no recurrence has been reported in last six months
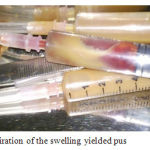 |
Figure 5: Aspiration of the swelling yielded pus
|
Discussion
Oral submucous fibrosis is a potentially malignant disorder of oral mucosa that has received considerable debate in the recent years because of its progressive incapacitating and resistant nature.
Burning sensation of the oral cavity and mucosal ulcerations are the initial symptoms of OSMF. As the disease progresses, the manifestations include blanching and stiffening of the oral mucosa leading to restricted mouth opening, along with palpable fibrous bands in the buccal mucosa, circumoral bands in upper and lower labial mucosa, shrunken uvula along with restricted tongue movements.3
Numerous treatment modalities are currently employed for OSMF, ranging from medical and surgical interventions, physiotherapy after cessation of the habit, and usually, a combination of these are used in clinical practice. With multiple treatment options being used, no single modality can provide complete cure of the disease.4 However for symptomatic relief of burning sensation, intralesional steroid treatment for 6-8 weeks is most commonly practiced.
According to the systematic review of medical interventions for OSMF by Kerr et al., 16 studies had predominantly used intralesional injections of corticosteroids4 and none of these studies had mentioned complications due to the same in OSMF patients.
In many centers, intralesional injection of corticosteroids is being implemented as the first line therapy for patients (stage II and III OSMF) with mouth opening less than 20mm. The primary mechanism of action of corticosteroids is through immune modulation. Corticosteroids suppress inflammation, decelerate fibrosis and upregulate immune-mediated fibrinolytic pathways.5
Many studies have shown that intralesional steroid therapy due to its anti-inflammatory property is useful in controlling burning sensation and improving mouth opening.5,6,7,8 This local treatment is based on the principle that a high activity could be produced at the site of administration and, at the same time, the systemic side-effects can be minimized.9
The side effects of intralesional steroids for the management of OSMF are rarely reported. In the present case, abscess formation occurred in bilateral buccal space which may be due to the inoculation of the oral flora to the deep tissues during the injections. However the contents, after aspiration of the abscess, was sent for culture demonstrated no growth of microorganisms, prompting a diagnosis of a sterile abscess. Rare instances of abscess formation after corticosteroid injections have been reported in other sites of the body such as spinal epidural and foot region.10-12 In certain instances, few drugs persist in the tissue spaces following injection and can cause irritation, which leads to granuloma formation and gets walled off forming a sterile abscess. Several authors have attempted to clarify the mechanism of abscess formation and found similar incidences of sterile pus collection.13The other rare complication of steroid therapy in OSMF reported was central serous chorioretinopathy which resolved after discontinuation of the steroid therapy.14 It is hypothesized that treatment using intralesional injections of various drugs leads to increased fibrosis and marked trismus.15 Few authors have advocated deterioration in mouth opening due to needle stick injury at multiple sites while administering submucosal injections.
Clinical Significance
The main purpose of reporting this case is to convey to the clinicians about the importance of detailed history and higher imaging in obtaining a correct diagnosis. Furthermore, this case also alerts us about the unusual complication of most commonly used modality i.e. intralesional steroid for the treatment of burning sensation and to improve the mouth opening in OSMF patients.
Conclusion
Although steroids are most popular and frequently used drug used for the treatment of OSMF, however, it is important to keep in mind that it is a “double-edged sword”. When used in proper dosage at regular intervals, it will give excellent beneficial results, but a clinician must be aware of its rare complication as manifested in this case. Varied presentation or an idiosyncratic reaction unique to an individual patient can occur by frequently used drugs and should be noticed early. The treatment should be discontinued immediately. The crux in the management of OSMF should be to diagnose the condition at the earliest and arrest the disease progression.
Acknowldegement: We sincerely thank the participant for his active co-operation and participation.
Conflict of Interest Statement
The authors report no conflict of interest.
References
- Warnakulasuriya S, Johnson NW, Waal I. Nomenclature and classification of Potentially malignant disorders of the oral mucosa. J Oral Pathol Med 2007;36:575–80.
CrossRef - Angadi PV, Rao S. Management of oral submucous fibrosis: an overview. Oral Maxillofac Surg. 2010;14:133-142.
CrossRef - Trivedy CR, Craig G, Warnakulasuriya S. The oral health consequences of chewing areca nut. Addiction Biology 2002;7:115-125.
CrossRef - Kerr AR, Warnakulasuriya S, Mighell AJ, et al. A systematic review of medical interventions for oral submucous fibrosis and future research opportunities. Oral Dis. 2011;17:42-57.
CrossRef - Tilakaratne et al. Intralesional corticosteroids as a treatment for restricted mouth opening in oral submucous fibrosis Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:224-231
CrossRef - Singh M, Niranjan HS, Mehrotra R, Sharma D, Gupta SC. Efficacy of hydrocortisone acetate/hyaluronidase vs. triamcinolone acetonide/hyaluronidase in the treatment of oral submucous fibrosis. Indian J Med Res. 2010;131:665-669.
- Ariyawardana A, Nawagamuwa T, Ranasinghe AJ, Sitheeque M, Vithanaarachchi N. Conservative management of oral submucous fibrosis. Asian J Oral Maxillofac Surg. 2005:26-30.
- Kumar A, Bagewadi A, Keluskar V, Singh M. Efficacy of lycopene in the management of oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:207-213.
CrossRef - Gilman AG, Rall TW, Nies AS, Taylor P. The pharmacological basis of therapeutics: 8th Edition, New York: Pergamon Pres. 1994; pp 1431-1462, 1572-1591.
- Vijay KK, Potti A: Spinal epidural abscess after corticosteroid injections. South Med J 957:772–774, 2002.
- Olson RK, Voorhees RE, Eitzen HE, Rolka H, Sewell CM. Cluster of postinjection abscesses related to corticosteroid injections and the use of benzalkonium chloride. West J Med 170:143–147, 1999.
- Theodore A. Buccilli Jr, Hugh Ryan Hall, James D. Solmen, Sterile Abscess Formation Following a Corticosteroid Injection for the Treatment of Plantar Fasciitis. The Journal of Foot & Ankle Surgery 2005;44:466–468.
CrossRef - Sawyer RG, Pruett TL. Cellular mechanisms of abscess formation: macrophage procoagulant activity and major histocompatibility complex recognition. Surgery 1996;1203:488 – 495.
CrossRef - Indu Bhushan Kar and Alok Kumar Sethi. A rare ocular complication following treatment of oral submucous fibrosis with steroids. Natl J Maxillofac Surg. 2011;2:93–95.
CrossRef - Borle RM, Borle SR. Management of oral submucous fibrosis: a conservative approach. J Oral Maxillofac Surg 1991;49:788-91.
CrossRef








