Kalyana C. P1, Thippeswamy H. M2 and Nanditha K. M2
1Manipal College of Dental Sciences, Manipal University, Manipal.
2Jagadguru Sri Shivarathreeshwara University Dental College and Hospital, Mysore.
Corresponding Author E-mail: drkalyan81@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1196
Abstract
Dental caries is multifactorial disease and is influenced by socio-demographic factors and health beliefs of the individuals. This study aimed to evaluate the relationship of oral health beliefs with caries experience in children of Udupi district. We conducted a cross-sectional survey 13−15 year old school children (n=463). A self-administered kannada version of oral health belief questionnaire was used. Clinical examination was carried out to assess the dental caries among children. Factor analysis revealed a 5 factor structure. Sampling adequacy was also high based on the Kaiser's measure of sampling adequacy (0.813) and communality values of over 0.3 indicated that the variables were reliable. Internal consistency (standardized item alpha) was 0.753. The domains that showed significant higher scores in caries free than carious children were benefits of prevention, barriers, perceived seriousness and seriousness about oral disease (p=0.005, 0.044, 0.018 and 0.019) respectively. The modified version oral health beliefs scale discriminated children with caries from caries free children.
Keywords
Beliefs; caries; dental; health; oral
Download this article as:| Copy the following to cite this article: Kalyana C. P, Thippeswamy H. M, Nanditha K. M. Oral Health Beliefs and Dental Caries Among Children of Udupi District. Biomed Pharmacol J 2017;10(2). |
| Copy the following to cite this URL: Kalyana C. P, Thippeswamy H. M, Nanditha K. M. Oral Health Beliefs and Dental Caries Among Children of Udupi District. Biomed Pharmacol J 2017;10(2). Available from: http://biomedpharmajournal.org/?p=15177 |
Introduction
Oral health is integrated component of general health and wellbeing that has implications on physical and psychological aspects. An optimal and acceptable level of oral health is prerequisite for better quality of life, self-esteem and social confidence which help people to communicate and socialize with confidence.1
The two major dental problems that manifest in early childhood are dental caries and periodontal disease. During the stage of eruption of permanent teeth (7-13 years), maintenance of oral hygiene is quite challenging. This will lead to the increased risk of caries and gingivitis which can manifest as periodontal disease. Such early onset risk factors could be prevented by simple remedial measures like chemical and mechanical plaque control methods, regular dental visits and change in behavior.2
Many behavioral models were proposed to effectively explain health behaviors out of which Health Belief Model (HBM) is most widely used in public health frameworks. Its framework was developed Hochbaum as a model for health educators to plan prevention oriented behavior change models.3 The initial model has evolved over the years with various types of health beliefs. The beliefs in this model were “susceptibility”, “seriousness”, “importance”, “benefits”, “barriers” and “general motivation”.4 Researchers suggested that health behavior could be predicted via perceived barriers and general motivation or self-efficacy which are the main domains.5-7 Studies have reported that the perceived severity was significantly associated with brushing frequency and oral hygiene behavior.2,7-9 Few studies reported that the model predicted oral health behavior,10 while the others reported the usefulness in view of its drawbacks.11 Due to paucity of literature between caries status and HBM, we aimed to evaluate the relationship of oral health beliefs with caries experience in children of Udupi district.
Materials and Methods
We carried out a cross-sectional study among 13−15 year old school children (n=463) of two private and two government schools. The details of the sampling methods and sample size calculation were mentioned in our previous study. The study was approved by the University Ethics Committee, Manipal University, Manipal.
The data collection procedure was done in 3 phases. Firstly, the socio-demographic information like age and gender, oral hygiene practices were recorded. This was followed by self-administered Kannada version of oral health belief questionnaire. Lastly, clinical examination was carried out to assess the dental caries among children by one trained and calibrated investigator as per WHO guidelines (1997).12 Intra-examiner reliability (Cohen’s Kappa) for dental caries was 0.92 (good agreement).
The Oral Health Belief questionnaire included “perceived susceptibility”, “perceived severity”, “perceived benefits”, “perceived barriers” and “perceived self-efficacy” with 18 items rated on 4 point likert scale.4 The questionnaire was translated from English to Kannada by two expert translators. The obtained Kannada version of the questionnaire was back translated to English by two other translators. The validity of the content was evaluated by two experts who also evaluated for word modifications to ensure conceptual and functional equivalence of the questionnaire. A pilot study was carried out on a group of children to check if they could understand the content of the questionnaire. After the pilot study 2 of the 18 items were deleted (“drinking fluoridated water helps prevent tooth decay” and “using fluoride is a harmless way of preventing tooth decay”) due to non-response in pilot study. On personal interviews, lack of awareness and knowledge were the reasons mentioned for non-response of these two items.
Exploratory factor analysis was done to evaluate construct validity and internal consistency was evaluated by Cronbach’s alpha. All the analysis was done using SPSS version 17 (SPSS Inc, Chicago, Ill, USA). A p-value of ≤0.05 was considered as statistically significant. Comparison of oral health belief items and total score was done by independent sample t test. Principal component analysis using Varimax rotation was performed after deletion of 2 items from the questionnaire. Only factors with more than 1 eigenvalues were retained based on the heuristic and practical grounds.
Results
A total of 463 children were completed all the stages of the survey out of which 252 were boys. Twelve children were excluded due to various reasons. Majority of the children (63.5%) were from private schools. The mean age of the participants was 14.11 ± 0.82. A total of 195 (42.1%) have never visited dentist in their life time.
Out of the 16 items of oral health beliefs questionnaire, the mean scores for the items 2, 3, 4, 7, 9, 11, 15 had significantly higher in caries free children than caries group. Overall, total score was also significantly higher in caries free than carious group (Table 1).
Table 1: Comparison of item scores with caries experience
| Items in the questionnaire | Caries free | Caries experienced | P-value |
| Mean±SD | Mean±SD | ||
| 1. Tooth decay can make people look bad. | 3.18±0.70 | 3.13±0.74 | 0.489 |
| 2. Dental problems can be serious. | 3.33±0.59 | 3.18±0.72 | 0.035 |
| 3. Poor teeth will affect people’s work or other aspects of their everyday life. | 3.25±0.61 | 3.06±0.71 | 0.007 |
| 4. Having dental problems can cause other health problems. | 3.14±0.68 | 2.91±0.79 | 0.004 |
| 5. I place great value on my dental health. | 3.45±0.59 | 3.40±0.62 | 0.416 |
| 6. It is important to keep natural teeth. | 3.25±0.67 | 3.17±0.72 | 0.279 |
| 7. Dental disease is as important as other health problems. | 3.13±0.77 | 2.96±0.80 | 0.039 |
| 8. I am not afraid of dental visits because of possible pain. | 3.25±0.66 | 3.24±0.78 | 0.883 |
| 9. Dentists are available when I have dental problems. | 3.15±0.64 | 2.96±0.79 | 0.018 |
| 10. I will visit the dentist when I have dental problems no matter how busy I am. | 3.13±0.64 | 3.04±0.77 | 0.214 |
| 11. Brushing teeth with fluoride toothpaste helps prevent tooth decay. | 3.18±0.68 | 2.98±0.73 | 0.008 |
| 12. Brushing teeth helps prevent gum problems. | 3.20±0.65 | 3.08±0.79 | 0.111 |
| 13. Using dental floss helps prevent gum disease. | 3.17±0.68 | 3.17±0.67 | 0.978 |
| 14. Eating sweet food causes tooth decay. | 3.30±0.67 | 3.29±0.73 | 0.938 |
| 15. Going to the dentist will keep me from having trouble with my teeth, gums, or dentures. | 3.28±0.66 | 3.06±0.80 | 0.006 |
| 16. Dentists are able to cure most dental problems that patients have. | 3.28±0.64 | 3.24±0.70 | 0.53 |
Factor analysis revealed a 5 factor structure based on the eigenvalues rule (>1) (Figure 1). Sampling adequacy was also high based on the Kaiser’s measure of sampling adequacy (0.813) and communality values of over 0.3 indicated that the variables were reliable (Table 2). Internal consistency reliability (standardized item alpha) was 0.753 which reduced when any one of the item was deleted from the questionnaire which suggested that all the items were required. The corrected item total correlation ranged from 0.28 to 0.42 (minimum required ≥ 0.20).
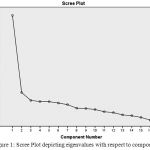 |
Figure 1: Scree Plot depicting eigenvalues with respect to components |
Table 2: Factor loadings of the items in the oral health belief questionnaire (Construct validity)
| Domains | Factor loadings | Cumulative variance | |
| Item 1 | Seriousness about oral disease | 0.563 | 21.399 |
| Item 2 | Perceived seriousness | 0.737 | 29.403 |
| Item 3 | Perceived seriousness | 0.662 | 35.978 |
| Item 4 | Seriousness about oral disease | 0.722 | 42.396 |
| Item 5 | Importance | 0.566 | 48.792 |
| Item 6 | Importance | 0.393 | 54.906 |
| Item 7 | Importance | 0.648 | 60.791 |
| Item 8 | Importance | 0.636 | 66.015 |
| Item 9 | Barriers | 0.621 | 71.133 |
| Item 10 | Barriers | 0.767 | 76.135 |
| Item 11 | Benefits of prevention | 0.558 | 80.736 |
| Item 12 | Benefits of prevention | 0.509 | 85.225 |
| Item 13 | Benefits of prevention | 0.713 | 89.245 |
| Item 14 | Perceived seriousness | 0.409 | 93.180 |
| Item 15 | Benefits of prevention | 0.583 | 96.825 |
| Item 16 | Barriers | 0.527 | 100.000 |
The domains that showed significant higher scores in caries free than carious children were benefits of prevention, barriers, perceived seriousness and seriousness about oral disease (p=0.005, 0.044, 0.018 and 0.019) respectively (Table 3).
Table 3: Comparison of domain and total scores with caries experience
| Domains | Caries free | Caries experienced | P-value |
| Mean±SD | Mean±SD | ||
| Benefits of prevention | 12.82±1.67 | 12.28±1.94 | 0.005 |
| Barriers | 9.56±1.36 | 9.24±1.62 | 0.044 |
| Importance | 13.09±1.57 | 12.78±1.89 | 0.072 |
| Perceived seriousness | 9.88±1.30 | 9.53±1.48 | 0.018 |
| Seriousness about oral disease | 6.32±1.07 | 6.04±1.19 | 0.019 |
| Total | 51.68±4.72 | 49.88±5.47 | <0.001 |
Discussion
This study examined the association of oral health beliefs with the caries experience among children and also evaluated the validity and reliability of modified version of oral health belief scale. Out of the 16 items that were evaluated, seven items showed significantly higher scores in caries free children. Similarly 4 out of 5 constructs showed significantly higher mean score in caries free children. This suggested that oral health belief questionnaire discriminated the caries free from caries experienced children. Also, the study found that participants had acceptable knowledge about oral health beliefs irrespective of their caries status. Very few studies exist on the concept of oral health beliefs and only one studied used oral beliefs scale previously.4 Hence, it was difficult to compare the results of our study with the previous literature.
According to the HBM, health behaviors results from individuals behavior after accounting for the benefits and barriers in performing that behavior. People might be aware of their susceptibility but may not perceive the benefits of engaging in healthy behaviors. Therefore, beneficial behaviors may not be practiced, despite possible unacceptable consequences.2 The HBM helps to explain this difference between caries free and caries experienced children. A recent study evaluated oral health beliefs using dental coping beliefs scale13 showed that subjects with good oral health beliefs had frequent recent visitors for dental Findings from our study highlighted that oral health workers should focus more on these perceptions because increasing these perceptions would change the behaviors which prevent dental caries among children.
The prevalence of the dental caries depends on numerous factors viz., oral hygiene practices, frequency of in between meal sucrose consumption, fluoride usage, regular dental visits which also might affect the oral health beliefs of the children. This study highlights the importance of oral health beliefs in predicting the dental caries. The main limitation of the present study was owing to cross-sectional design due to which temporal association cannot be explained. Previous study reported that people may change their beliefs over time and might vary with each question.14 The modified version oral health beliefs scale discriminated caries free and caries experienced children and further studies are recommended to evaluate long term stability of these beliefs and their relationship with other oral conditions. Evaluation of oral health beliefs in adolescence and young adults would help identify negative perceptions about oral health. Oral health promotion activities can be planned in such group to improve beliefs about oral health.
Conflict of Interest
Nil
Acknowledgements
We thank all the children and school authorities for their active cooperation during this study.
References
- Oral Health Promotion: An Essential Element of a Health-Promoting School. WHO Information Series on School Health Document Eleven. Geneva: WHO; 2003. WHO/NMH/NPH/ORH/School/03.3.
- Stokes E, Ashcroft A, Platt MJ. Determining Liverpool adolescents’ beliefs and attitudes in relation to oral health. Health Educ Res. 2006;21:192-205.
CrossRef - Rosenstock LM. Historical origins of the Health Belief Model. Health Education Behav 1974;2:328-335.
CrossRef - Nakazono TT, Davidson PL, Andersen RM. Oral health beliefs in diverse populations. Adv Dent Res. 1997;11:235-44.
CrossRef - Chen MS, Land KC: Testing the health belief model: LISREL analysis of alternative methods of causal relationships between health beliefs and preventative dental behavior. Soc Psychol Q 1986;49:45–60.
CrossRef - Vakili M, Rahaei Z, Nadrian H, YarMohammadi P: Determinants of oral health behaviors among high school students in Shahrekord, Iran based on Health Promotion Model. J Dent Hyg 2011;1:39–48.
- Solhi M, Shojaei Zadeh D, Seraj B, Faghih Zadeh B: The Application of the Health Belief Model in oral health education. Iranian J Publ Health 2010;39:114–119.
- Anagnostopoulos F, Buchanan H, Frousiounioti S, Niakas D, Potamianos G: Self-efficacy and oral hygiene beliefs about tooth brushing in dental patients: A model-guided study. Behav Med 2011;37:132–139.
CrossRef - Kühner MK, Raetzke PB: The effect of health beliefs on the compliance of periodontal patients with oral hygiene instructions. J Periodontol 1989;60:51–56.
CrossRef - Sharma M, Romas JA: Theoretical Foundations of Health Education and Health Promotion. London: Jones & Bartlett Learning International; 2012.
- Kasmaei P, Amin Shokravi F, Hidarnia A et al. Brushing behavior among young adolescents: does perceived severity matter. BMC Public Health 2014;14:8.
CrossRef - WHO oral health surveys, 4th Edition, 1997; WHO
- Samuel SR, Khatri SG, Acharya S, Patil ST. The Relationship Between Life Course Factors, Parental Demographics, Dental Coping Beliefs and Its Influence on Adolescents Dental Visit: a Cross Sectional Study. Ethiop J Health Sci. 2015;25:243-50.
CrossRef - Broadbent JM, Thomson WM, Poulton R. Oral health beliefs in adolescence and oral health in young adulthood. J Dent Res. 2006;85:339-43.
CrossRef








