Effect of Sub-Gingival Margins Influencing Periodontal Health–A Systematic Review and Meta Analysis.
Dhanraj. M1, Benita. P. B. D. S1, Acu. Varma2 and Ashish. R. Jain2
1Department of Prosthodontics, Saveetha Dental College and Hospitals, Saveetha University, Chennai, India.
2Department of Prosthodontics, Saveetha Dental College and Hospital, Chennai, India.
Corresponding Author E-mail: dr.ashishjain_r@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/1163
Abstract
It is widely believed supra gingival restoration margins are more desirable than sub gingival margins with respect to periodontal health. Nevertheless sub gingival margins do have many indications and improved restorative materials with superior bio-compatibility has promoted placement of sub gingival margins . The long term effects of sub gingivally placed crown margins needs to be studied further in detail.To evaluate and compare the difference between supra gingival and sub gingival margins influencing periodontal health.An electronic search was conducted for scholarly articles about sub gingival margins influencing periodontal health. written in English or translated into English listed with Pubmed, Cochrane library, Science Direct, Wiley online library, Google scholar data bases, The NewYork Academy of Medicine Grey literature Report and Ingenta Connect till march 31st 2016. Research strategy identified 150 potential articles after reading the title and abstract 15 articles were selected and 4 articles satisfied the inclusion and exclusion criteria and 11 articles were excluded. The data was extracted , tabulated and subjected to meta analysis. A random effects model was chosen at 95% confidence interval. There was no statistically significant difference between the supra and subgingival margins with respect to plaque and gingival indices[ ( Z = 1.12, p = 0.26) ( Z = 0.22, p = 0.83 ) ] . However pocket depth showed a statistically significant difference ( Z = 0.86, p = 0.001). Both supra and sub gingival margins influence the periodontal health in a similar manner with respect to plaque accumulation and gingival health status,but an increase inpocket depth was observed with subgingival margins.
Keywords
Sub gingival margins; supra gingival margins; periodontal health
Download this article as:| Copy the following to cite this article: Dhanraj M, Benita P. B. D. S, Varma A, Jain A. R.Effect of Sub-Gingival Margins Influencing Periodontal Health–A Systematic Review and Meta Analysis. Biomed Pharmacol J 2017;10(2). |
| Copy the following to cite this URL: Dhanraj M, Benita P. B. D. S, Varma A, Jain A. R.Effect of Sub-Gingival Margins Influencing Periodontal Health–A Systematic Review and Meta Analysis. Biomed Pharmacol J 2017;10(2). Available from: http://biomedpharmajournal.org/?p=14578 |
Introduction
Insertion of fixed partial dentures may influence the periodontal conditions and the risk for caries. Clinical observations show that the gingiva supporting prosthodontically treated teeth often is inflamed and that pocket formation and recession of gingiva may occur. The potentially injurious effect of dental restorations on the gingiva has been the subject of several histological and clinical investigations.1,2,3,4 In histological studies in dogs, Marcum5 observed the best gingival response when the crown margins were located at the gingival crest compared to either sub-gingival or supragingival placement, while Karlsen1 in dogs as well observed this in supra-gingival cases. In clinical studies in human an unfavorable reaction in the gingival tissue and a slight increase in loss of attachment have primarily been observed when the margin of the restoration have been located subgingivally.2,6 Regular oral health maintenance programmes for patients receiving fixed prosthodontics has in clinical studies, been documented to reduce gingival inflammation and recession.7,8 Caries have also been observed to be one of the main reasons for crown and bridge failure.1,9,10 However, the protective effect against caries of sub-gingivally located crown margins has been questioned.2 Therefore, to observe the long term effect of the location of crown margins to the gingival margin concerning periodontal reaction, caries in crowned teeth as well as alveolar bone-loss is of great clinical value in crown and bridge therapy. The location of the apical extent of the cast fixed partial denture retainer margin has been discussed at great length In the dental literature. Along with cast restoration margins in general, many authors have suggested the extension of these margins to a subgingival location. The rationale for subgingival marginal placement has included the enhancement of esthetics and tooth preparation retention form, and the notion of the gingival sulcus as a caries free zone. There has not, however, been agreement as to the degree of subgingival extension. Various investigators have suggested that the margins should be placed at the base of the gingival sulcus, 3mm from the alveolar crest, 0.5mm from the coronal extent of the junctional epithelial attachment, half the distance between the base of the sulcus and the gingival margin or at the crest of the gingival margin.
The theory of a caries free zone was originally disputed by Orban in 1941 and by data from later clinical trials. Additionally there is considerable evidence that the subgingival retainer margin was often associated with an undesirable periodontal response. Bacterial plaque retained on relatively rough restoration surfaces and on the exposed dental cement between the tooth and the restoration is difficult for the patient and the dentist to remove, and is responsible for the inflammatory changes seen in the periodontium adjacent to subgingival restoration margins. In recent times, this evidence has led to increasingly popular notion that restoration margins should be placed supra gingivally whenever possible. Additionally from this evidence one might hypothesize that the more apical the subgingival marginal placement, the more apical the observed inflammatory changes. At present only one source of evidence supports the hypothesis. The configuration of the FPD retainer margin has also been of concern to clinicians. A horizontal over extension of this margin has commonly been referred as an overhang. Data from a number of studies have shown the detrimental periodontal effects of the over hangs, or horizontally over extended margins, but there are no data demonstrating the effects of the short or horizontally under extended restoration margin. There is evidence that the horizontally under extended and over extended retainer margin tooth configuration occurs quite frequently in clinical practice. Therefore the periodontal effects associated with both of these types of retainer configuration are of clinical interest.
The purpose of this systematic review is to assess the periodontal response to subgingivally placed retainers.
Aim
To evaluate periodontal health in complete veneer crowns with supra gingival margins.
To evaluate periodontal health in complete veneer crowns with sub gingival margins.
To compare the difference between supra gingival and sub gingival margins influencing periodontal health.
Null Hypothesis
These is no difference between supra gingival and sub gingival margins influencing periodontal health.
Alternative Hypothesis
These is difference between supra gingival and sub gingival margins influencing periodontal health.
PICO Analysis
Population: Teeth receiving complete veneer restorations.
Intervention: Sub gingival margins / finish lines for complete veneer crowns.
Comparison: Supra gingival margins
Outcome: Periodontal health measured by plaque index, gingival index, bleeding index, pocket depth, periodontal index and tooth mobility index.
Variables of Interest
Periodontal health, 2. Outcome measures ohi index ,bleeding index,gingival index,periodontal index, 3. Bone loss around the abutment, 4. Type of finish lines, 5. Materials used for complete veneer crowns, 6. Location of the abutment, 7. Occlusal forces acting over the complete veneer crowns, 8. Brushing techniques used, 9. Type of tooth brush and dentifrices, 10. Frequency of dental visits and oral prophylaxis.
Materials and Methods
Search Methodology
The search methodology applied was a combination of MESH terms and suitable keywords. The terms sub gingival margins influencing periodontal health and other relevant keywords were not enlisted in the MeSH database and hence discrete keyword search was initiated based on PICO cluster.
Population
Complete veneer crowns, full coverage crowns, full crowns, full retainers, metal crowns, metal ceramic crowns, acrylic crowns, all ceramic crowns, PFM crowns, complete veneer retainers, cantilevered abutment, pier abutments.
Intervention
Crevicular margins, cemental margins, subgingival margins, extended margins, root margins, margins for periodontally compromised teeth, dentinal margins, esthetic margins, shoulder margins, heavy chamfer margins, knife edged margins, radial shoulder, feather edged margins, chisel margins, retention fractures, sloped shoulder.
Comparison
Supra gingival margins, self cleaning margins, shoulder margins, chamfer margins, sloped margins, feather margins, chiselled margins.
Outcome
Gingival health, gingival hygiene, oral health status, plaque index, calculus index, debris index, OHI simplex index, bleeding index, silness and hoe index, bone loss, loe and silness index, periodontal index, russels index, periodontitis, gingivitis, gingival enlargement, periodontal health, periodontal disease, angular bone loss, vertical bone loss, chronic periodontitis, horizontal bone loss, gingival recession.
Selection of studies
The review process consist of two phases. In the first phase titles and abstract of the search were initially screened for relevance and the full text of relevant abstract were obtained and accessed. The hand search of selected journals as well as search of references in the selected studies were also done. The articles that were obtained after first step of review process using the following inclusion and exclusion criteria were screened in second phase and relevant and suitable articles were isolated for further processing and data extraction.
Inclusion Criteria
Randomised control trials comparing sub gingival and supra gingival margins for periodontal health.
Randomised control trials comparing metal crowns with sub gingival and supra gingival margins for periodontal health.
Randomised control trials comparing all ceramic crowns with sub gingival and supra gingival margins for periodontal health.
Randomised control trials comparing metal ceramic crowns with sub gingival and supra gingival margins for periodontal health.
Controlled clinical trials comparing sub gingival and supra gingival margins for periodontal health.
Longitudinal study comparing sub gingival and supra gingival margins for periodontal health.
Exclusion Criteria
Randomised control trials comparing sub gingival and supra gingival margins with partial veneer crowns.
Randomised control trials comparing sub gingival and supra gingival margins with acrylic crowns.
Randomised control trials comparing sub gingival and supra gingival margins with long term provisional crowns.
Studies dealing Periodontal health over fractured margins.
Studies dealing Restorations luted with temporary cements.
Prospective study comparing sub gingival and supra gingival margins.
Studies dealing with implant abutment margins.
Result
Research strategy identified 150 potential articles after reading the title and abstract 15 articles were selected and 4 articles satisfied the inclusion and exclusion criteria and 11 articles were excluded. The data was extracted,summated and tabulated (Table 1,Table 2). Homogeneity was observed with plaque index scores in all the articles and 3 articles for gingival index and pocket depth and hence the results from these articles were subjected to meta analysis and Forest plots were generated for all the outcome measures. The effect size was determined to be the difference in means of the outcome measures and a random effects modem was chosen at 95% confidence interval. With respect to plaque index the overall effect was Z = 1.12, p = 0.26 indicating there was no statistically significant difference between sub gingival and supra gingival margins (Fig 1). With respect to gingival index the overall effect was Z = 0.22, p = 0.83 indicating there was no statistically significant difference between sub gingival and supra gingival margins (Fig 2). With respect to pocket depth, the overall effect was Z = 0.86, p = 0.001 indicating a statistically significant difference between sub gingival and supra gingival margins. However the magnitude of the effect size is low (Fig 3).The funnel plots for all outcome measures showed no publication bias.(Fig. 4,5,6).
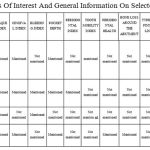 |
Table 1: Variables Of Interest And General Information On Selected Articles.
|
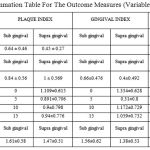 |
Table 2: Summation Table For The Outcome Measures (Variables Of Interest)
|
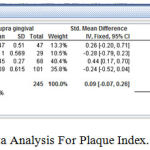 |
Figure 1: Meta Analysis For Plaque Index. (Forest Plot)
|
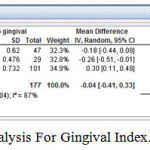 |
Figure 2: Meta Analysis For Gingival Index. (Forest Plot)
|
 |
Figure 3: Meta Analysis For Pocket Depth. (Forest Plot)
|
 |
Figure 4: Funnel Plot For Studies Included For Pocket Depth
|
 |
Figure 5: Funnel Plot For Studies Included For Gingival Index
|
 |
Figure 6: Funnel Plot For Studies Included For Plaque Index
|
Discussion
A longitudinal study, was carried out by Valderhaug et al1 in a group of 102 patients who received 108 bridges and it was inferred the amount of plaque did not differ between the crowned teeth and the control teeth during the observation period, while GI score 2 and 3 was more frequent in crowned teeth than in the control teeth during 10 year period. This was mainly observed when the crown margins were located sub-gingivally. A slight increase in mean pocket depth was recorded in the crowned teeth while the mean pocket depth for the control teeth remained at the same level during the 15 years. No statistical differences in bone loss could be detected between the control teeth and the crowned teeth.10 The reports after 5 and 10 years concluded that the patients had maintained healthy periodontal conditions and relatively low caries incidence on the abutment teeth over many years. The authors attributed this result to the regularly professional prophylaxis received every 6 months. These 6-month controls ended after 10 years. Although a slightly higher prevalence of periodontal index was seen at the 15-year examination, there were no changes of pattern of the patients’ gingival or periodontal conditions. This may show that the patients after receiving professional oral prophylaxis twice a year during the first 10 years themselves had adopted a high standard of dental care. A further result of the relatively good oral hygiene exerted by the patients is that the periodontal conditions of the abutments and the control teeth were more similar than it would have been if the oral hygiene had been poor.11 A survey was conducted of 423 crown margins that were divided into 355 subgingival margins and 68 supragingival margins. The plaque index, gingival bleeding, and recession surrounding the artificial crown were recorded and compared to the unprepared contralateral tooth. Gingival tissues tended to bleed 2.42 times more frequently with subgingival margins and have a 2.65 times higher chance of gingival recession. Crowns with supragingival margins did not differ significantly compared with the contralateral tooth, but crowns with subgingival margins had greater bleeding and recession compared with the contralateral tooth. It is recommended that supragingival margins become standard clinical procedures when feasible. A further analysis will be instituted to determine whether different crown materials affect the gingiva.12 The author in his study firmly established that subgingival crown margins were associated with gingival bleeding and recession in a significant number of patients and supports other studies. Supra gingival margins of crowns are recommended as a standard clinical practice, provided there is sufficient tooth structure for resistance and retention form. It is possible in many patients for gingivitis to lead to periodontitis. However, the rate of progression of periodontitis is a complex process and affected by many variables. Nevertheless, subgingival crown margins can initiate gingivitis and eventually periodontitis with loss of attachment of teeth. The effect of subgingival electronic pressure sensitive probe and the determination of Periodontal Index (PI) and Gingival Index(GI) scores. Statistical analysis showed that both the horizontally under extended and over extended retainers had significantly greater GI scores than had their own matched unrestored teeth at the first, or long term, examination. The retainers that were under extended and those that were both subgingival and overextended also had a significantly greater GI score than their matched unrestored teeth at the second, or short term, examination. In addition the under extended retainers were associated with significantly greater GI scores than the over extended retainers at the second examination. The variation in the retainer configuration had no effect on BP scores or PD measurement.13,14 No long term periodontal effects resulted from differences in retainer marginal location, but some short term differences were observed at the second examination, which occurred 2-3 weeks after scaling and reinforcement of patient home care. Despite the observation that retainer margins located at or coronal to the gingival crest were associated with significantly greater PI scores than subgingivally located retainer margins, the subgingival margins were associated with higher GI scores at the second examination there was no statistically significant difference in BP scores detected between the retainer marginal location groups, but some difference in PD were seen. Specifically, retainer margins located 2 to 3 mm apical to the gingival crest exhibited significantly increased mean PD measurements than either those retainer margins that were located 1mm apical to the crest or those in the at-crest supragingival group. These effects however were absent over long term observation periods. These results suggest that the effects of retainer margin location were “cancelled out” by the long term presence of plaque.15
Freilich et al16 studied the periodontal response to posterior fixed partial denture (FPD) retainers with distinct marginal configurations and locations. One posterior proximal site restored with a clinically acceptable FPD and one matched, unrestored posterior proximal site were examined in 60 subjects. Assessments were made of the FPD retainers and the periodontal responses to both the long-term and short-term use of these retainers. Periodontal examination included assessment of probing depth and bleeding on probing and determination of plaque index and the gingival index scores. Statistical analysis showed that clinically acceptable FPDs, which had clinically detectable deviations from an ideal retainer/tooth configuration, were not associated with increased probing depth or bleeding on probing when compared to the matched, unrestored teeth at both examinations. As a group, sites adjacent to subgingival retainer margins were not associated with greater probing depths than sites adjacent to supragingival retainer margins. These findings suggest that long-term exposure to variations of FPD margin configuration and location, within clinically acceptable but less than ideal parameters, are not associated with the destruction of the supporting periodontal tissues.
Al-Sinadi A et al17 in their study aimed to assess the periodontal status of Saudi adult females who had received regular oral prophylaxis following the insertion of fixed partial dentures. The effects of sub- and supra-gingivally placed crown margins were also assessed. The study sample included 78 females who had fixed partial dentures made by senior students at the College of Dentistry of King Saud University in Riyadh, Saudi Arabia.
The study results showed an increase in the plaque and gingival indices in majority of the study subjects (>94%). In addition, the abutment teeth scored significantly higher mean scores of plaque and gingival indices than the non-abutment teeth. These findings are consistent with several other studies reporting more plaque accumulation and gingival inflammation on the crowned teeth, and there is a general acceptance of high correlations between the dental plaque and presence of gingivitis.
The probing pocket depth increased in all study participants and the abutment teeth presented significantly greater mean values of probing pocket depth compared to the non-abutments. This observation can be considered as an outcome of increased plaque accumulation and gingival inflammation. Valderhaug and Birkeland suggested that factors related to crown fabrication could contribute to increased attachment loss. Although Silness and Bader et al18 reported similar results, Ericsson and Marken,19 however, found no significant differences in the probing pocket depth between the abutment and non-abutment teeth.
The highest scores of all clinical parameters were recorded in the study subjects who were 46 year-old or older and those who had their functioning FPDs for more than 5 years. Similar observations were reported previously by Holm-Pedersen et al.20 Grossi et al. and Kinane who found that periodontal diseases were more prevalent in older age groups and they considered ageing as one of the identified risk factors for periodontitis. However, Wennström et al.21 reported that periodontal diseases were more prevalent and severe in the elderly because of the cumulative destruction over a lifetime period rather than an age–related intrinsic deficiency or abnormality that affects susceptibility to periodontal infection.
Considering the location of the crown margins, the present meta analysis showed that teeth with sub-gingivally placed crown margins had higher mean scores of plaque and gingival indices, however no statistically significant difference in effect size was observed between the supragingival and subgingival margins. Greater mean values probing pocket depth was observed in teeth with supra-gingival crown margins. A similar observation was reported previously. It can be concluded that the sub-gingival crown margins can contribute to localized periodontal inflammation because these margins can provide a protected environment in which the indigenous microbes mature into a more periodontopathic flora.
There could be several other factors (Periodontal health, OHI index , bleeding index, gingival index, periodontal index, bone loss around the abutment, type of finish lines, materials used for complete veneer crowns, location of the abutment, occlusal forces acting over the complete veneer crowns, brushing techniques used, type of tooth brush and dentifrices, frequency of dental visits and oral prophylaxis contributing to this observation and literature has insufficient volume involving the corroboration of all these factors. Hence randomized control trials taking into consideration all these factors should be initiated to understand this phenomenon more discreetly.
Conclusion
Both supra and sub gingival margins influence the periodontal health in a similar manner with respect to plaque accumulation and gingival health status. However there was a mild increase in pocket depth with respect to sub gingival margins. This difference may not be clinically significant and more randomised controlled trials with high statistical power and increase sample size needs to be conducted for a better understanding of this phenomenon.
Reference
- Karlsen K. Gingival reactions to dental restorations. Acta Odontologica Scandinavica. 1970;28(6):895-904.
CrossRef - Valderhaug J. Periodontal conditions and carious lesions following the insertion of fixed prostheses a 10-year follow-up study. International dental journal. 1980;30(4):296-304.
- Mörmann W., Regolati B., Renggli H. H. Gingival reaction to well‐fitted subgingival proximal gold inlays. Journal of clinical periodontology. 1974;1(2):120-5.
CrossRef - Bader J. D., Rozier R. G., McFall W. T., Ramsey D. L. Effect of crown margins on periodontal conditions in regularly attending patients. The Journal of prosthetic dentistry. 1991;65(1):75-9.
CrossRef - Marcum J. S. The effect of crown marginal depth upon gingival tissue. The Journal of prosthetic dentistry. 1967;17(5):479-87.
CrossRef - Silness J. Periodontal conditions in patients treated with dental bridges. Journal of periodontal research. 1970;5(1):60-8.
CrossRef - Suomi J. D., Greene J. C., Vermillion J. R., Doyle J., Change J. J., Leatherwood E. C. The effect of controlled oral hygiene procedures on the progression of periodontal disease in adults results after third and final year. Journal of periodontology. 1971;42(3):152-60.
CrossRef - Nyman S., Lindhe J. A longitudinal study of combined periodontal and prosthetic treatment of patients with advanced periodontal disease. Journal of Periodontology. 1979;50(4):163-9.
CrossRef - Valderhaug J. A 15-year clinical evaluation of fixed prosthodontics. Acta Odontologica Scandinavica. 1991;49(1):35-40.
CrossRef - VALDERHAUG J., KARLSEN K. Frequency and location of artificial crowns and fixed partial dentures constructed at a dental school. Journal of Oral Rehabilitation. 1976;3(1):75-81.
CrossRef - Silness J., Ohm E. Periodontal conditions in patients treated with dental bridges. Journal of periodontal research. 1974;9(2):121-6.
CrossRef - Orkin D. A., Reddy J., Bradshaw D. The relationship of the position of crown margins to gingival health. The Journal of prosthetic dentistry. 1987;57(4):421-4.
CrossRef - Valderhaug J., Ellingsen J. E., Jokstad A. Oral hygiene, periodontal conditions and carious lesions in patients treated with dental bridges. Journal of Clinical Periodontology. 1993;20(7):482-9.
CrossRef - Valderhaug J., Heløe L. A. Oral hygiene in a group of supervised patients with fixed prostheses. Journal of periodontology. 1977;48(4):221-4.
CrossRef - Kandelman D., Nally J. N., Meyer J. M. Clinical and radiographic control in 112 cases of fixed prosthesis. Schweizerische Monatsschrift fur Zahnheilkunde= Revue mensuelle suisse d’odonto-stomatologie. 1974;84(11):1248.
- Freilich M. A., Niekrash C. E., Katz R. V., Simonsen R. J. Periodontal effects of fixed partial denture retainer margins: configuration and location. The Journal of prosthetic dentistry. 1992 Feb 1;67(2):184-90.
CrossRef - Al-Sinaidi A., Preethanath R. S. The effect of fixed partial dentures on periodontal status of abutment teeth. The Saudi Journal for Dental Research. 2014;5(2):104-8.
CrossRef - Silness J., Hegdahl T. Area of the exposed zinc phosphate cement surfaces in fixed restorations. European Journal of Oral Sciences. 1970;78(1‐4):163-77.
CrossRef - Ericsson S. G., Markén K. E. Effect of fixed partial dentures on surrounding tissues. The Journal of prosthetic dentistry. 1968;20(6):517-25.
CrossRef - Holm‐Pedersen P., Agerbæk N., Theilade E. Experimental gingivitis in young and elderly individuals. Journal of clinical periodontology. 1975 Mar 1;2(1):14-24.
CrossRef - Gottlow J., Nyman S., Lindhe J., Karring T., Wennström J. New attachment formation in the human periodontium by guided tissue regeneration Case reports. Journal of clinical periodontology. 1986;13(6):604-16.
CrossRef








