Kobra Mohammadi, Elham Keshavarz, Zahra Dehghani and Roya Fallahian
Department of Radiology, Mahdieh Hospital, Shahid Beheshti University of Medical Science, Tehran, Iran.
Corresponding Author E-mail: elhamkeshavarz@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/1134
Abstract
Pyelectasis (a rise in the anteroposterior diameter of renal pelvis more than 4 to 10 mm) can increase the possibility of disorders such as amniotic fluid problems and result in urinary tract abnormalities including ureteropelvic junction obstruction (UPJO). Pyelectasis is also loosely associated with chromosomal syndromes including trisomy 13, 18 and 21. The present research seeks to study the prevalence of renal pyelectasis in the second trimester ultrasound screening in the Mother’s Fetuses resorting to Mahdiye medical center over the period of 2014 to 2016 and their follow up after birth.In this research, all mothers who had resorted to Mahdiyeh Hospital of Tehran for the second trimester ultrasound screening from 2014 to 2016 were studied. Neonatal’s information after their birth in terms of affliction with major trisomy and renal problems and diseases was also studied and recorded. Finally, the prevalence of pyelectasis and its correlation with urinary tract abnormalities including UPJO and chromosomal syndromes was measured.Mothers aged 23 to 37 with an average of 29.67 ± 4.382 years. The prevalence of pyelectasis among the fetuses studied was 3.6% (36 cases) while this number for prevalence of urinary tract abnormalities diagnosed after birth was 0.2% (2 cases of UPJO) and all of them were suffering from pyelectasis and their mothers were older than 35. The level of FPR, PPV, sensitivity and specificity of pyelectasis disorder to be diagnosed with UPJO abnormalities was 3.4, 5.5, 100, and 96.6% respectively. Statistical analyses failed to show any significant difference caused by gender in terms of affliction with UPJO (P-value>0.5). A statistically significant difference was also observed between fetuses with UPJO and normal fetuses in terms of the number of pyelectasis (P-value < 0.5). A review of the results showed a higher frequency of pyelectasis among male fetuses than their female counterparts. Although this research failed to find any correlation between pyelectasis and chromosomal disorders, this complication may increase the possibility of affliction with urinary tract abnormality.
Keywords
Renal Pyelectasis; UPJO; Congenital Renal Anomalies
Download this article as:| Copy the following to cite this article: Mohammadi K, Keshavarz E, Dehghani Z, Fallahian R. Studying The Prevalence of Renal Pyelectasis in the Second Trimester Ultrasound Screening in Iranian Mother’s Fetuses and their follow up after Birth. Biomed Pharmacol J 2017;10(1). |
| Copy the following to cite this URL: Mohammadi K, Keshavarz E, Dehghani Z, Fallahian R. Studying The Prevalence of Renal Pyelectasis in the Second Trimester Ultrasound Screening in Iranian Mother’s Fetuses and their follow up after Birth. Biomed Pharmacol J 2017;10(1). Available from: http://biomedpharmajournal.org/?p=14232 |
Introduction
Genitourinary system is commonly influenced by congenital anomalies and a study of the second trimester sonography can help us measure this complication (1). Fetal pyelectasis is one of the most common fetal anomalies identified in the second trimester ultrasound screening (2). Most pregnancies with pyelectasis have natural Karyotype. As a result, the danger of Aneuploidy among fetuses with pyelectasis is a controversial issue. On the other hand, some researchers have concluded that fetuses with multiple sonographic markers have a higher possibility of Aneuploidy (3-5). Some researchers have pointed to a higher rate of fetal pyelectasis among male fetuses compared to their female counterparts (6), but some studies report conflicting results (7). Renal pyelectasis takes place when the diameter of renal pelvis goes up. 1 to 3% of fetuses studied by sonography in the second trimester of pregnancy exhibited isolated renal pyelectasis. A review of previous researches points to the fact that renal pyelectasis in the presence of other congenital anomalies or sonographic markers may increase the possibility of Aneuploidy and particularly trisomy 13, 18, and 21 (2, 8, 9). According to Pediatric Urological Association (10), renal pyelectasis takes place when anteroposterior diameter of renal pelvis is more than 4-10 mm, depending on the week of pregnancy, whose prevalence is estimated around 1.1 to 3.3% (11-13). Diagnosing renal pyelectasis is very important as it is an aneuploidy marker and a primary symptom of urinary tract pathology. Some scholars consider pyelectasis a physiological state with absolutely no clinical value. Recent discoveries have shown that this result can be very important with respect to important pathological states which may require surgery to prevent renal injuries. As a result, post-delivery examinations may be very important and vary from an intense urological track to physiological analysis of pelvic dilatation less than 15 mm (15). Various studies have highlighted the prevalence of pyelectasis in male fetuses. Presence of pyelectasis in male fetuses shows a physiological variant, while it indicates higher risk of chromosomal disorders in female fetuses (7). There are many sonographic results (including structural or non-structural anomalies or markers) which can help diagnose down syndrome during the embryonic period (4, 16, 17). Sonographic findings which are generally considered to be possible markers for trisomy 21 in the second trimester of pregnancy include nuchal thickening، hyperechoic bowel، echogenic intracardiac focus, femur or shortened humerus, and renal pyelectasis (18-21). These markers are non-exclusive and can be observed in non-problematic fetuses as well. Furthermore, they are usually transitory and can be easily observed in the third trimester. As a result, the further analysis and study of these markers in various races and populations seems necessary. Another important point about fetal pyelectasis diagnosed in the second trimester of pregnancy is the fact that researches point to the fact if renal pyelectasis does not recover during the embryonic period, it can have a significant correlation with fetal renal problems that require surgery (1). A considerable percent of these cases can be considered a natural result mostly observed in male fetuses (7). The present research seeks to determine the prevalence of renal pyelectasis in second trimester ultrasound screening of fetuses resorting to Mahdiyeh medical center from 2014 to 2016 and their follow up after birth in terms of affliction with renal diseases (particularly those requiring surgical intervention) and chromosomal disorders.
Materials and Method
This is a descriptive research conducted on all pregnant mothers resorting to Mahdiye Hospital of Tehran from 2014 to 2016 for second trimester sonography. Following the principles of medical ethics and after gaining their consent, the participants took part in the research voluntarily. According to the previous researches and inclusion criteria, as many as 1000 participants were selected for each group. These mothers were studied in terms of renal pyelectasis and divided into mild, moderate and severe groups. Next, neonatals were studied for major chromosomal disorders such as trisomy 13, 18, and 21 and post-birth renal diseases and problems. Finally, the correlation between renal pyelectasis and its intensity with chromosomal disorders, major anomalies and post-birth neonatal renal problems and diseases was studied. Having obtained this information, IBM SPSS Statistics v.21 was used to analyze the raw data. Further to determining the rate of prevalence, renal pyelectasis was used as a diagonal marker to predict occurrence of ureteropelvic junction obstruction (UPJO) and diagonal parameters such as the sensitivity and exclusiveness of FPR, PPV, NPV, and ACC indicators were also calculated. Non-parametric Chi-Square Test with level of significance of P-value < 0.05 was used to analyze data.
Results
The variables were first defined, then raw data was studied using appropriate statistical tests. Mothers whose fetuses had renal pyelectasis aged 23 to 37 years with an average of 29.67 ± 4.382 years. Out of the whole 36 fetuses with renal pyelectasis, 28 (77.8%) were male while the remaining 8 (22.2%) were female. The fetuses aged 18 to 25.5 weeks (126 to 179 days) with an average age of 20.18 ± 2.053 weeks (141.61 ± 14.439 days). Fetal pyelectasis levels were divided into three categories: mild, moderate and severe. The results indicated 34 mild cases (94.4%) and 2 moderate cases (5.6%). The status of kidneys in fetuses showed a frequency of 66.7% for bilateral complication, while the frequency of this problem in the left and right kidney was 27.8% and 5.6%, respectively. 34 mothers whose fetuses were diagnosed with renal pyelectasis had healthy neonatals after delivery, while 2 mothers with the same age conditions and sonographic results had children with ureteropelvic junction obstruction (UPJO). As many as 20 mothers in their first delivery and 16 in their second delivery had fetuses with renal pyelectasis. An analysis of post-delivery status of fetuses in terms of their gender points to the fact that out of 28 male fetuses with renal pyelectasis, 26 fetuses (26.4%) were normal and 2 were suffering from ureteropelvic junction obstruction (UPJO) complication. All 8 female fetuses were normal. Then, mothers whose fetuses were with renal pyelectasis were divided into two groups: younger than or as old as 35, and older than 35. According to the results, 3 mothers younger than 35 had healthy kids after delivery while 2 mothers with the same age conditions and sonographic results had children with ureteropelvic junction obstruction (UPJO). In the group of mothers older than 35, 4 were diagnosed who had healthy kids after delivery (graph 1).
 |
Graph 1: Neonatal’s status based upon mother’s age with renal pyelectasis in fetus
|
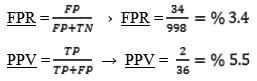
The prevalence of fetuses with renal pyelectasis in this research was 3.6%, while a frequency of 0.2% was reported for UPJO. Considering the number of those with UPJO after birth, sensitivity (TPR) and exclusiveness (TNR) of pyelectasis marker was calculated as a diagonal marker. The sensitivity and exclusiveness of renal pyelectasis to diagnose UPJO was 100% and 96.6% respectively.
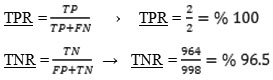
The false positive rate (FPR) for fetuses with pyelectasis for affliction with UPJO after birth was equal to 3.4%. In this research, PPV (Positive Predictive Value) which shows the possibility of having someone with positive test results was equal to 5.5%.
Based on calculations, the prevalence of UPJO among female and male neonatals was 0 and 7.14% respectively. Using an appropriate statistical test, we studied the correlation between postpartum status of neonatals and gender of fetuses with renal pyelectasis. The results of this statistical test failed to show a statistically significant difference between the above-said parameters (P-value > 0.05). This research studied the correlation between postpartum status of neonatals and ureteropelvic junction obstruction (UPJO) using appropriate statistical tests (Table 1). The results of this research point to a statistically significant correlation between renal pyelectasis and UPJO (P-value < 0.05). In the group with renal pyelectasis, 2 fetuses were suffering from UPJO, while none of the neonatals without renal pyelectasis were suffering from UPJO or other abnormalities.
Table 1: Distribution and analysis of correlation between postpartum status of neonatals and renal pyelectasis
| Pyelectasis | Total | P-value | |||
| Yes | No | ||||
| UPJO abnormality | Yes | 2 | 0 | 2 | 0.001 |
| No | 34 | 962 | 998 | ||
Discussion
Various researches have sought to find the cause of renal pyelectasis observed in prenatal period. The researchers have arrived at the conclusion that fetal pyelectasis is caused by temporary dilatation of the collecting system, obstructive urophathy of the upper and lower tract, and non-obstructive processes such as vesicoureteral reflux. Nguyen et al (2010) studied several common and important diseases that may result in pelvis dilation with their rate of prevalence. They claimed that UPJO was responsible for 10 to 30% of all cases of pyelectasis observed in neonatals (22). Considering the results of current research, the frequency rate of UPJO is much less than Nguyen. Several researches have been conducted on the correlation between the gender of fetus and occurrence of pyelectasis and UPJO. Most of these researches have confirmed the fact that these complications are more common among males. A research by Woodward et al (2002) titled “postpartum management of pyelectasis remaining from prenatal period” reported ureteral obstruction in 20 to 25% of all cases with its prevalence among males being 3 times as much as what is observed among females (23). Another research was conducted by Bornstein in 2006 whose results were published. Their studies sought to study the correlation between gender and the possibility of affliction with major trisomies in fetuses with pyelectasis. Although their research was different from ours in terms of genetic abnormalities, but it was in line with our research in terms of the higher rate of pyelectasis among males (2.14 : 1) (7). The results of our research were in line with those researches by Woodward and Bornstein with the number of male fetuses with pyelectasis (77.8%) being 3.5 times as many as female fetuses (22.2%). Tracking the renal status of fetus after it was diagnosed with pyelectasis was another accomplishment of our research. In postpartum phase, it turned out that pyelectasis was gone in 94% of neonatals while UPJO is still observed in 6% of them. A study with a similar goal was conducted by Signorelli in 2005 (1). In his retrospective research conducted on 375 fetuses with complete urological follow-up, it turned out that only 18.6% of all fetuses with pyelectasis had returned to their natural state after their birth. This is a much smaller number compared to what was observed in our research. A quick review points to the fact that sample volume, race, operator and device error are responsible for the difference observed between the results of current research and other studies. A rate of 3.6% was reported for the prevalence of pyelectasis which is in line with most researches carried out in this field. For example, Coco et al conducted a research on many fetuses. They arrived at the conclusion that pyelectasis is observed in 2.9% of all fetuses (2). The present research failed to find any case of chromosomal disorders such as major trisomies. This is not in line with the findings reported by some researchers. Such disagreement is observed in the study of Orzechowski. Orzechowski et al (2013) conducted a large-scale meta-analysis in order to study isolated renal pyelectasis in the second trimester of pregnancy as a marker of trisomy 21. In their research, as many as 10 observational studies including 2148 cases of isolated renal pyelectasis were investigated. In 7 of such researches, isolated fetal pyelectasis was assumed equal to anteroseptal diameter of 4 mm or more. According to their results, diagnosis of isolated renal pyelectasis in second trimester sonography is correlated with the higher possibility of trisomy 21. At the end of their research, they arrived at the conclusion that if findings of isolated renal pyelectasis are used to study the risk of trisomy 21 from maternal serum tests, a possibility rate of 2.78% needs to be considered in calculations (24).
Conclusion
By conducting this research in our country and based upon the calculations used here, considerable results were achieved which urged researchers to draw important conclusions. First, no major difference is observed between Iran and other countries in terms of the global prevalence of this disease. Considering the results of this research, it can be concluded that prevalence of pyelectasis in male fetuses is more than what is observed in their female counterparts. Although it is possible for pyelectasis not to result in chromosomal disorders, it can be a useful marker with high potential to determine prevalence of postpartum renal disorders. Finally, the difference between the results of our research and other studies can be attributed to sample volume, race, operator and device error.
References
- Signorelli M, Cerri V, Taddei F, Groli C, Bianchi UA. Prenatal diagnosis and management of mild fetal pyelectasis: implications for neonatal outcome and follow-up. Eur J Obstet Gynecol Reprod Biol. 2005;118(2):154-9.
- Coco C, Jeanty P. Isolated fetal pyelectasis and chromosomal abnormalities. American journal of obstetrics and gynecology. 2005;193(3 Pt 1):732-8. Epub 2005/09/10.
- Bornstein E, Barnhard Y, Donnenfeld AE, Ferber A, Divon MY. The risk of a major trisomy in fetuses with pyelectasis: the impact of an abnormal maternal serum screen or additional sonographic markers. American journal of obstetrics and gynecology. 2007;196(5):e24-6.
- Nicolaides K, Shawwa L, Brizot M, Snijders R. Ultrasonographically detectable markers of fetal chromosomal defects. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 1993;3(1):56-69. Epub 1993/01/01.
- Benacerraf BR, Neuberg D, Bromley B, Frigoletto FD, Jr. Sonographic scoring index for prenatal detection of chromosomal abnormalities. J Ultrasound Med. 1992;11(9):449-58.
- Wax JR, Cartin A, Pinette MG, Blackstone J. Does the frequency of soft sonographic aneuploidy markers vary by fetal sex? J Ultrasound Med. 2005;24(8):1059-63.
- Bornstein E, Barnhard Y, Donnenfeld A, Ferber A, Divon MY. Fetal pyelectasis: does fetal gender modify the risk of major trisomies? Obstet Gynecol. 2006;107(4):877-9.
- Bromley B, Lieberman E, Shipp TD, Benacerraf BR. The genetic sonogram: a method of risk assessment for Down syndrome in the second trimester. J Ultrasound Med. 2002;21(10):1087-96; quiz 97-8. Epub 2002/10/09.
- Nyberg DA, Souter VL. Sonographic markers of fetal trisomies: second trimester. J Ultrasound Med. 2001;20(6):655-74. Epub 2001/06/13.
- Kent A, Cox D, Downey P, James SL. A study of mild fetal pyelectasia – outcome and proposed strategy of management. Prenat Diagn. 2000;20(3):206-9.
- Chitty L, Winter RM. Congenital malformations. BMJ. 1990;300(6717):121-2.
- Malone PS. Antenatal diagnosis of renal tract anomalies: has it increased the sum of human happiness? J R Soc Med. 1996;89(3):155P-8P.
- Benacerraf BR, Mandell J, Estroff JA, Harlow BL, Frigoletto FD, Jr. Fetal pyelectasis: a possible association with Down syndrome. Obstet Gynecol. 1990;76(1):58-60. Epub 1990/07/01.
- Adra AM, Mejides AA, Dennaoui MS, Beydoun SN. Fetal pyelectasis: is it always “physiologic”? American journal of obstetrics and gynecology. 1995;173(4):1263-6.
- Thomas DF, Madden NP, Irving HC, Arthur RJ, Smith SE. Mild dilatation of the fetal kidney: a follow-up study. Br J Urol. 1994;74(2):236-9.
- Benacerraf BR, Nadel A, Bromley B. Identification of second-trimester fetuses with autosomal trisomy by use of a sonographic scoring index. Radiology. 1994;193(1):135-40. Epub 1994/10/01.
- Nyberg DA, Luthy DA, Resta RG, Nyberg BC, Williams MA. Age-adjusted ultrasound risk assessment for fetal Down’s syndrome during the second trimester: description of the method and analysis of 142 cases. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 1998;12(1):8-14. Epub 1998/08/11.
- Gray DL, Crane JP. Optimal nuchal skin-fold thresholds based on gestational age for prenatal detection of Down syndrome. American journal of obstetrics and gynecology. 1994;171(5):1282-6. Epub 1994/11/01.
- Nyberg DA, Dubinsky T, Resta RG, Mahony BS, Hickok DE, Luthy DA. Echogenic fetal bowel during the second trimester: clinical importance. Radiology. 1993;188(2):527-31. Epub 1993/08/01.
- Bromley B, Lieberman E, Laboda L, Benacerraf BR. Echogenic intracardiac focus: a sonographic sign for fetal Down syndrome. Obstet Gynecol. 1995;86(6):998-1001. Epub 1995/12/01.
- Nyberg DA, Resta RG, Luthy DA, Hickok DE, Williams MA. Humerus and femur length shortening in the detection of Down’s syndrome. American journal of obstetrics and gynecology. 1993;168(2):534-8. Epub 1993/02/01.
- Nguyen HT, Herndon CA, Cooper C, Gatti J, Kirsch A, Kokorowski P, et al. The Society for Fetal Urology consensus statement on the evaluation and management of antenatal hydronephrosis. Journal of pediatric urology. 2010;6(3):212-31.
- Woodward M, Frank D. Postnatal management of antenatal hydronephrosis. BJU international. 2002;89(2):149-56.
- Orzechowski KM, Berghella V. Isolated fetal pyelectasis and the risk of Down syndrome: a meta-analysis. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2013;42(6):615-21. Epub 2013/05/29.







