Alireza Kamali1, Alireza Rostami2, Hesamoddin Modir1 and Maryam Shokrpour3
1Department of Anesthesiology, Arak University of Medical Sciences, Arak, Iran.
2Department of Cardiac Surgery, Arak University of Medical Sciences, Arak, Iran.
3Department of Gynecology, Arak University of Medical Sciences, Arak, Iran.
Corresponding Author E-mail: Alirezaros@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/1098
Abstract
Early extubated of open heart surgery patients (T <8hr) benefits for the patient so that led to reduced hospital stay, reduced need for nursing care, reduced length of stay in the ICU and reduce the risk of ventilator-associated pneumonia is. Therefore the effect of BIS monitoring on the patients after open heart surgery are extubated early. This study is a randomized, double blind, randomized clinical trial on patients undergoing elective CABG were done in hospitals Amir. A total of 120 patients were randomized into two groups and monitoring (B) BIS and monitoring (N) BIS groups. The duration of extubated patients after open heart ICU admission were compared between the 2 groups. The mean BIS Monitor blood pressure before induction of anesthesia before surgery, 2.5 - / + 115 and without Monitor 3.6 - / + 121, respectively. The heart rate monitors in group BIS 5/4 - / + 72 and without Monitor 6.4 - / + 70. The mean extubation time in hours at the monitor BIS 6/3 - / + 4/5 hours at no monitor BIS 3/4 - / + 2/6 hours. Given that no significant difference was seen between the two groups P ≤ 0/05. The use of monitoring BIS (Depth of Anesthesia) during CABG surgery resulted in a reduction of patients extubated in the ICU, open heart, reducing the pain score at 12 and 24 hours after the operation.
Keywords
Early Extubation; CABG Patient; BIS Monitoring
Download this article as:| Copy the following to cite this article: Kamali A, Rostami A, Modir H, Shokrpour M. Studying the effects of BIS Monitoring (Depth of Anesthesia) in early Extubation of Patients Candidated for Non-Emergency CABG. Biomed Pharmacol J 2017;10(1). |
| Copy the following to cite this URL: Kamali A, Rostami A, Modir H, Shokrpour M. Studying the effects of BIS Monitoring (Depth of Anesthesia) in early Extubation of Patients Candidated for Non-Emergency CABG. Biomed Pharmacol J 2017;10(1). Available from: http://biomedpharmajournal.org/?p=13631 |
Introduction
The patients undergoing open heart surgery directly enter Open Heart ICU. Thus they skip PACU and their recovery takes place in ICU. These patients enter OHICU in an intubated state and ventilator is connected to them so that they may reach the desirable conditions for extubation (1). Based on the interpretation and analysis of arterial blood gases (ABG) and their level of consciousness and the volume and number of their breathes, the patients are candidate for extubation (2). Recent researches have demonstrated the advantages of early extubation (T < 8 hr) for patients undergoing open heart surgery (3). These studies all point to the fact that extubation of patients in a period of less than 8 hours after entering ICU has considerable advantages compared to their extubation over 12 hours and 24 hours after entering ICU such as reducing the length of hospitalization (staying at hospital), less need for nursing cares, shorter hospitalization in ICU and reduction of problems associated with dependence upon ventilator and reducing the chance of affliction with ventilator-caused pneumonia (4). Long term intubation of these patients (T > 24 h) increases the rate of mortality and morbidity among these patients (5) and this factor has further encouraged heart anesthesiologist to take the necessary measures to extube patients as early as possible (6). Early extubation of patients (8 hours or less after their entry to ICU or even 4 hours after entrance to ICU) reduces the chances of affliction with ventilator-caused pneumonia, depression, and recovery period of patients and increases patients’ satisfaction (3, 4, 5, 7, 8). This fact has attracted a considerable amount of attention particularly over the last 10 years (9, 10). BIS (BisPectral Index) monitoring which is originally a monitor used to measure patients’ depth of anesthesia and measures their level of consciousness through probes connected to patients’ forehead plays a major role in causing an appropriate anesthesia with the correct and expected depth (11, 12). This monitor is graded from 0 to 100 and represents the level of consciousness and depth of anesthesia in patients. Full consciousness is represented by 100 while 40-60 represents a level of consciousness which is appropriate for operation and surgery (13). A BIS level ranging from 40 to 60 results in an appropriate anesthesia with no awareness during operation and balances the level of anesthetic drugs in an appropriate volume. What’s more, it will prevent late awakening and extubation of patients (12, 14, 15, 16). It is necessary to use BIS during general anesthesia, particularly in open heart surgeries. BIS is an EEG parameter which separates the levels of anesthesia into 5 categories:
Awake: 85 – 100, Sedation: 65 – 85, General Anesthesia: 40 – 65, Deep Hypnosis: 30 – 40, Brust Suppression: 0 – 30
The system of depth of anesthesia monitoring was first developed and used as a modern technology in developed countries such as the U.S. The high rate of patients’ awakening during deep anesthesia operations and uncontrolled use of medicine have led the authorities of these countries to recommend utilization of such systems. This technology is entering other countries as well. Due to complexity of the process of anesthesia, the technology and techniques used in this field are quite limited. Based on scientific resources, the main technology known as BIS index is found in nearly 73% of best hospitals and it is installed in 53% of all operation rooms. This technology is currently used in 160 countries all around the world. However, different factors such as its high cost, unfamiliarity with the device and failing to understand its advantages and potentials and low level of health service in developing countries have rendered introduction of this technology a bit slower. There is no doubt that need for this technology will make it imperative to use it in not very distant future. Further to the high level and quality of therapeutic services achieved through appropriate management of anesthesia, it prevents patients from awakening during operation, and wipes out any chances of medical intoxications and uncontrolled consumption of medicines. It will also help personnel separate the sleep caused by anesthetic drugs and sleep caused by state of coma (3). These problems are quite common in Iranian hospitals (2) as this issue may cause Posttraumatic stress disorder (PTSD) and there is currently no data concerning its complexity (1). There are certain extubation protocols for those open heart surgery patients who enter ICU with a trachea tube. According to these protocols, the patient needs to be completely conscious and able to lift his head of the bed (RR < 30, HCo2 – 22-24, 45 > PCo2 > 40 ph > 7.35). The patient is also required to be in a stable hemodynamic state. Using BIS can help prepare these conditions as soon as possible. Thus, keeping in mind the above-said explanations and previous researches, using BIS monitoring in OH-ICU can cause a state of anesthesia with an appropriate depth and prepare the patient for early extubation. Thus, we decided to study BIS monitoring and early extubation among patients applying for open heart surgery.
Materials and Method
The present research is a randomized, double blind clinical trial conducted on non-emergency patients applying for CABG in Amir Almomenin Hospital of Arak. 120 randomized patients of hospital were divided into two categories using the randomized numbers’ table: those with BIS monitoring (B) and those without BIS monitoring (N). All patients took part in the research after they received necessary explanations and were informed of methods of research. After they were assured that the research would have no side effects for them, their written consent was gained. They were randomly divided into B and N groups. The whole ASA belonged to classes II and III who had undergone premade the night preceding surgery using Oxazepam. On the morning of the appointed day of operation, they received 3-5 mg of morphine and 12-25 mg promethazine. Then, they entered the operation room and all of them received 3-5 cc/kg crystalloid liquid to make up for CVE. Having entered the operation room, full monitoring (SPO2, PR, ECG, and thermometer) of them was conducted. Having received 1-2cc sufentanil, the patients were prepared to take their arterial line for IBP (Invasive Blood Pressure) monitoring. Using 18-20 g needle, arterial line was taken from the arteries of patient’s left hand Radian artery. After arterial line preparation and IBP monitoring, the patient was inducted using 5-10 μ/kg sufentanil and 0.1 mg/kg midazolam and 10-12 mg Pavulon. Having placed the tube and fixed the tracheal line, the patients were prepared to receive CVline. An Arrow™ CVP was used to take patients’ CVline through internal jugular. If taking CVline was not possible, internal jugular through right Subclavian was tried. The patients were then prepped and drepped and catheterized and prepared for operation. Before induction and after pre-mode while the patients were lethargic and unconscious, BIS monitoring probes were placed on the foreheads of group B members. BIS monitoring was fixed by a resident who had no interference with completing and analyzing the questionnaires. None of them knew which group they belonged to. They only received information at the beginning of research about the research itself and monitoring. The patients then underwent total IVline anesthesia (TIVA) using Atra and Sufentanil following Propofol (as much as 30-35 cc/h mixture of Atra+Amprazolam+Sufnetanil with a dose of 20-25 cc/h was added to Propofol). The amount and volume of medicines was determined based upon the patient’s Hemodynamics. Based on the patients’ Hemodynamics (no more than 15% rise in PR and BP) and the level of BIS, the level of the maintenance dose for group B during the operation was set between 40 and 50. In the case of too much rise or reduction of BIS or reduction of PR and BP, a higher dose of maintenance medicines will increase or decrease. The dose of maintenance medicines in group N was determined merely based upon patient’s Hemodynamics and this dose was adjusted in accordance with any rise or fall in the level of PR and BP. The patients were then placed on Cardiopulmonary bypass (CPB) in order to conduct the grafts of coronary arteritis. The dose of the drugs was reduced to half. The dose of drugs prescribed for group B was adjusted based upon BIS monitoring and patients’ hemodynamics (MAP), while the doses in group N were fixed only based upon MAP. During the operation and after CPB, the core temperature of patient was measured using Esophageal probe. Just like before placing the patients on CPB, the same doses continued to be used after operation. At the end of the operation, the patients were intubated and sent to ICU-OH while they were still unconscious and had a stable hemodynamics. BIS monitoring in ICU-OH still continued in ICU-OH for group B patients. They were extubated with regards to BIS. In other words, when BIS > 60 and further signs of extubation criteria were observed, the patients were extubated. The following extubation criteria following open heart surgery were defined: 1. The patient must be completely conscious, 2. The patient needs to be able to lift his head off the bed, 3. Ph > 7.35 and 45 > PCo2 > 40, HCo3 – 22 – 24, 4. RR < 30, and 5. The patients must have a constant hemodynamics. After full consciousness and achieving the right respiratory rate and volume and when extubation criteria were fulfilled, the patients were extubated in ICU-OH (in group N). The pain scores of all patients was defined and measured using VAS 4, 12, and 24 hours after operation. During the operation, the intern assistance of this project filled the questionnaires which contained the demographic and hemodynamic information of patients and the average numbers of BIS were recorded. The dose of anesthetics in group B was determined by assistant resident and anesthesiologist based upon BIS and hemodynamics and with regards to hemodynamics (traditional type of anesthesia). The resulting information was then put in SPSS for statistical analysis. The statistical information achieved through this analysis was deduced by a second anesthesiologist. Thus the statistical analyst and anesthesiologist were blind as to how the patients were distributed in these 2 groups. Finally, the average length of patients’ extubation since their entrance to ICU-OH up to their extubation was measured. A simple sampling method was utilized and the sample size was calculated based on the previous studies and the following equations:
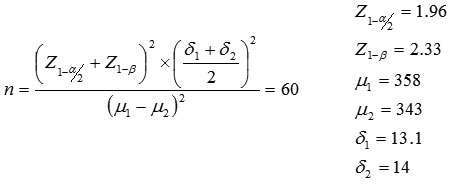
There were as many as 60 patients in each group making a total number of 120 cases. These participants were randomly distributed in two groups with or without BIS.
Table 1: The average length of extubation for non-emergency patients candidated for CABG after entering open heart ICU in BIS monitoring group and the group without BIS monitoring
| Extubation length / groups | With BIS monitoring | Without BIS monitoring | P-value |
| Average extubation length (h) | 5.4 ± 6.3 | 6.2 ± 4.3 | P ≤ 0.05
Significant |
Table 2: Comparing pain score 4, 12, and 24 hours after operation among non-emergency patients candidated for CABG after entering open heart ICU in BIS monitoring group and the group without BIS monitoring
| Pain score / groups | With BIS monitoring | Without BIS monitoring | P-value |
| Pain score 4 hours after operation | 1.2 ± 0.5 | 1.3 ± 0.85 |
P ≤ 0.05 significant |
| Pain score 12 hours after operation | 6.2 ± 1.8 | 7.8 ± 2.5 | |
| Pain score 24 hours after operation | 3.5 ± 1.5 | 3.7 ± 1.7 |
Inclusion Criteria
non-emergency patients aging 40 to 75 years old candidated for CABG who had resorted to Amir-al-Momenin Hospital of Arak who were in class II or III ASA with no past records of ICU hospitalization and long-term intubation before CABG operation. The operation should last 4 to 6 hours and the informed consent of patients needs to be taken.
 |
Figure 1: Average extubation time of non-emergency patients candidated for CABG after entering open heart ICU with and without BIS
|
Table 3: The amount of painkillers taken in the first 24 hours following operation among non-emergency patients candidated for CABG operation
| Painkiller used / groups | With BIS monitoring | Without BIS monitoring | P-vlaue |
| Average amount of painkiller used 24 hours after operation (mg morphine) | 22.8 ± 2.6 | 25.5 ± 3.3 | P ≤ 0.05 Significant |
Exclusion Criteria
emergency candidates of CABG, patients whose operations lasted shorter than 4 hours or longer than 6 hours, patients out of the age range defined (40 – 75), and those patients who were prescribed anesthetic gases such as surgical Sevoflurane further to TIVA. The final results were finally statistically analyzed using SPSS 19 and T-test and Kruskal-Wallis.
 |
Figure 2: Comparing pain score 4, 12, and 24 hours following operation among non-emergency patients candidated for CABG after entering open heart ICU with and without BIS
|
Table 4: The amount of Propofol taken during operation among non-emergency patients candidated for CABG operation with and without BIS
| Propofol used / groups | With BIS monitoring | Without BIS monitoring | P-vlaue |
| Average amount of Propofol used during operation (mg) | 1050 ± 10.8 | 1180 ± 14.4 | P ≤ 0.05 Significant |
Results
The average blood pressures before anesthetics induction and before the operation in the group with BIS and the other group were 115 ± 2.5 and 121 ± 3.6, respectively. The heart rates in BIS group and the other group were 72 ± 4.5 and 70 ± 4.6, respectively. As P ≥ 0.05, no significant difference was observed between the two groups and both groups were nearly the same in terms of pre-induction blood pressure and heart rate (table 5). The average age in BIS group and the other group was 66.8 and 67.6 respectively. 61.2% of the participants in BIS group and 60.8% in the other group were male and as P ≥ 0.05, no significant difference was observed between the two groups in terms of blood pressure (tables 6 and 7). The average length of extubation (hours) in BIS group and the other group was 5.4 ± 3.6 and 6.2 ± 4.3, respectively. As 0.05 ≥ P, a significant difference was observed between the two groups and the length of extubation (after patients’ entrance to open heart ICU)in BIS group was significantly shorter. Concerning the pain score of CABG patients 4 hours after operation the following scores were reported for BIS group and the other group respectively: 1.29 ± 0.5 and 1.39 ± 0.85. As P ≥ 0.05, no significant difference was observed here. The pain score 12 hours after the operation in BIS group and the other group was reported to be 6.2 ± 1.8 and 7.8 ± 2.5 respectively. The same groups had a pain score of 3.5 ± 1.5 and 3.7 ± 1.7 respectively 24 hours after the operation. As 0.05 ≥ P, no significant difference was observed between the two groups. The pain score 12 and 24 hours after operation in BIS group was significantly less (table 2). The amount of painkiller used within 24 hours after operation (mg of morphine) in BIS group and the other group was 22.8 ± 2.6 and 25.5 ± 3.3, respectively. As 0.05 ≥ P, a significant difference was observed between the two groups and more painkiller was used in the group without BIS (table 3). As 0.05 ≥ P, the amount of Propofol used in the BIS group was less than the other group.
Table 5: Blood pressure and heart beat among non-emergency patients candidated for CABG before anesthesia with and without BIS monitoring
| Blood pressure and heart beat / groups | With BIS monitoring | Without BIS monitoring | P-value |
| Average blood pressure | 115 ± 2.5 | 121 ± 3.6 | P ≥ 0.05 Insignificant |
| Average heart rate | 72 ± 5.4 | 70 ± 4.6 |
Table 6: Comparing the non-emergency patients candidated for CABG before anesthesia with and without BIS
| Gender / groups | With BIS | Without BIS | P-value |
| Male | 61.2% | 60.8% | P ≥ 0.05 Insignificant |
| Female | 38.8% | 39.2% |
Table 7: Comparing the non-emergency patients candidated for CABG before anesthesia in terms of age with and without BIS
| Average age / groups | With BIS | Without BIS | P-Value |
| Average age | 66.8 years | 67.6 years | P ≥ 0.05 Insignificant |
Discussion
Identifying the effects of BIS monitoring among the patients candidated for CABG for the early extubation of patients (less than 6 hours) is a major step towards shortening the length of hospitalization in ICU and costs of patient and removes dependence to ventilator and the pneumonia caused as a result of contact with ventilator. According to the results of our research, the average length of extubation (after entering heart ICU) among the patients with BIS monitoring was far less than those without BIS monitoring. In other words, BIS monitor during operation helps enhance post-operation extubation after entering heart ICU. Long intubation of CABG patients (more than 8 hours) results in greater mortality and morbidity among them (5). This issue has encouraged anesthesiologists to extubate patients candidated for CABG as soon as possible (6). Early extubation of patients candidated for CABG (less than 6 hours) results in less affliction with ventilator-caused pneumonia, shorter recovery period and higher levels of satisfaction (4,5,7). The results of this research showed that pain score 12 and 24 hours after operation was significantly less in BIS group compared to the other group. This is another advantage of using BIS monitoring during CABG operation. Reducing the pain score of patients helps reduce the amount of painkiller used within the first 24 hours after operation. The average amount of painkiller taken by BIS group within the first 24 hours following the operation was much less than what was observed in the other group. All these factors contributed to higher patient satisfaction and less pain.
Previous researches yielded quite different results. In a research conducted by Jrnnifer Anderson et al (2010) on 50 CABG patients, it turned out that the effect of BIS monitoring in early extubation of patients is not significant. The patients in this research were randomly divided into two groups with and without BIS monitoring. No difference was observed in terms of early extubation after entering heart ICU (1). In another study conducted by Alan Speir et al (2011) on 50 patients, no significant difference was observed between the two groups in terms of average extubation time with and without BIS monitoring (17). Another study conducted by Olson et al (2005) showed that using BIS monitoring results in using less Propofol during operation (15). A review of the previous researches showed that some of them were in line with our research while others were not. It is thus recommended to increase the number of samples and limit studies and coronary operations so that we may reinforce the results of this research. As the results indicate, using BIS monitoring can benefit patients despite causing extra monitoring costs. It can also shorten the length of extubation in heart ICU and reduce the length of hospitalization in ICU and hospital and decrease the general costs of patients. We would like to recommend a similar research with a greater number of samples and in cases of open heart surgery so that more accurate and generalizable results may be achieved.
Conclusion
Using BIS monitoring during CABG operation reduces the length of patients’ extubation in open heart ICU and decreases pain score of patients within 12 and 24 hours after operation.
Acknowledgement
The author wishes to thank the open heart personnel of Amir-al-Momenin Hospital for their ceaseless efforts and also Ms. Alvandi, Naderi, and Asgari for their great contribution.
References
- Anderson J, Henry L, Hunt S, Ad N. Bispectral index monitoring to facilitate early extubation following cardiovascular surgery. Clin Nurse Spec. 2010;24(3):140-8.
- Gelb.A, leslie K, Stanski . Monitoring the Depth of Anesthesia, 39th of Miller’s Anesthesia text book.7th ed.2010.Churchill Livingstone 2010,vol 1:498
- Hawkes CA, Dhileepan S, Foxcroft D. Early extubation for adult cardiac surgical patients.Cochrane Database Syst Rev.2003:003587.
- Cheng DC, Karski J, Peniston C, et al. Early tracheal extubation after coronary artery bypass graft surgery reduces costs and improves resource use. A prospective, randomized, controlled trial. Anesthesiology. 1996;85:1300–1310.
- Cheng DC, Karski J, Peniston C, et al. Morbidity outcome in early versus conventional tracheal extubation after coronary artery bypass grafting: a prospective randomized controlled trial. J Thorac Cardiovasc Surg. 1996;112:755–764.
- Gelb.A, leslie K, Stanski . Monitoring the Depth of Anesthesia, 39th of Miller’s Anesthesia text book.7th ed.2010.Churchill Livingstone 2010, vol 1:496
- Reis J, Mota JC, Ponce P, Costa-Pereira A, Guerreiro M. Early extubation does not increase complication rates after coronary artery bypass graft surgery with cardiopulmonary bypass. Eur J Cardiothorac Surg. 2002;21:1026–1030
- Silbert BS, Santamaria JD, O’Brien JL, Blyth CM, Kelly WJ,Molnar RR. Early extubation following coronary artery bypass surgery: a prospective randomized controlled trial. The Fast Track Cardiac Care Team. Chest. 1998;113:1481–1488.
- Reyes A, Vega G, Blancas R, Morató B, Moreno JL, Torrecilla C, Cereijo E. Early vs conventional extubation after cardiac surgery with cardiopulmonary bypass. Chest. 1997 Jul;112(1):193-201.
- Silbert BS, Santamaria JD, Kelly WJ, O’brien JL, Blyth CM, Wong MY, Allen NB; Fast Track Cardiac Care Team. Early extubation after cardiac surgery: emotional status in the early postoperative period. J Cardiothorac Vasc Anesth. 2001 Aug;15(4):439-44.
- Olson DM, Thoyre SM, Auyong DB. Perspectives on sedation assessment in critical care. AACN Adv Crit Care. 2007;18:380–395.
- BIS Technology. http://www.aspectmedical.com/AboutBIS.aspx.Accessed March 5, 2010
- BIS Education. http://www.biseducation.com/UploadedFiles/Assets/0000000012.pdf. Accessed January 2, 2009.
- Olson DM, Gambrell M. Balancing sedation with bispectral index monitoring. Nursing. 2005;35:321–322.
- Olson DM, Cheek DJ, Morgenlander JC. The impact of bispectral index monitoring on rates of propofol administration.AACN Clin Issues. 2004;15:63–73.
- Ozcan MS, Gravenstein D. The presence of working memory without explicit recall in a critically ill patient. Anesth Analg.2004;98:469–470.
- Henry L. Use of the bisectral index monitor(bis)when extubating cardiac surgery patients.American association of critical care nurses. 2011.








