Elhashimi E. Hassan1, Ehab A. M. Elagab2, Hassan B. Mohammed1, Ahmed El-basher Abdelgader1, Amar B. Elhussein1 and Mohammed Ayed Huneif3
1Department of Clinical Laboratory Sciences, College of Applied Medical Sciences, Najran University, Najran, Saudi Arabia.
2Department of Pathology, College of Medicine, Najran University, Najran, Saudi Arabia.
3Department of Pediatrics, College of Medicine, Najran University, Najran, Saudi Arabia.
Corresponding Author E-mail: alhashimihassan@hotmail.com
DOI : https://dx.doi.org/10.13005/bpj/1077
Abstract
Associations of subclinical autoimmune thyroiditis with type 1DM were frequently studied, but their role on the glycemic state was not well investigated. Nevertheless, very little data are available from KSA, despite an increase in incidence of disease. This study aimed to investigate the prevalence of subclinical autoimmune thyroiditis in patients with type 1DM and to evaluate their effect on HbA1c (Glycated hemoglobin) level as glycemic marker. The study comprised 132 Saudi children with type 1 diabetes mellitus, and 72 matched healthy control in age and sex. Patients diagnosis based on WHO criteria. The study excluded patients with thyroid disease, renal disease, liver disease, and anemia. HbA1c was measured using chromatography technique. The sera were used to assay the TSH (Thyroid stimulating hormone) concentrations using ELC (Electrochemiluminescent) technology while GAD antibodies (Anti thyroglobulin antibodies), TPO antibodies (Anti-thyroid peroxidase antibodies) & TG antibodies (Anti thyroglobulin antibodies) were measured by ELISA (Enzyme-Linked Immunosorbent Assay) from abcam –UK. The data were analyzed by SPSS. The study showed a higher distribution of anti-GAD, and thyroid autoantibodies (anti-TPO and anti-TG) among type1 DM patients 56.8%, 36.4% and 19.7% in contrast to lower distribution in controls 5.6%, 9.7% and 4.2% respectively. Furthermore a group of patients whom had positive autoimmune thyroid antibodies associated with a significant raising of HbA1c in compare to other patients group with negative auto thyroid antibodies P value ˂0.001 On the other hand, about 9.8% of diabetic patient showed high-level TSH and only 1.4 % in healthy group. Nevertheless, it seemed to be insignificantly associated with HbA1C. This study reported that the distributions of auto thyroid antibodies among type 1 DM patients were high in Saudi children. Perhaps theses autoantibodies may have indirect effect on glycemic control; a subject for further study. Furthermore, according to our finding it recommends to do serial thyroid profile investigation including thyroid auto- antibodies for type 1DM as a subclinical thyroiditis are not very rare.
Keywords
Anti-glutamic acid decarboxylase (Anti GAD); Anti thyroglobulin antibodies (Anti-TG); anti-thyroid peroxidase antibodies (Anti-TPO); Glycated hemoglobin (HbA1c); Thyroid stimulating hormone (TSH)
Download this article as:| Copy the following to cite this article: Hassan E. E, Elagab E. A. M, Mohammed H. B, Abdelgader A. EB, Elhussein A. B, Huneif M. A. Distribution of Thyroid Autoantibodies in Saudi Children with type 1 Dm and their effect on Glycemic Control. Biomed Pharmacol J 2017;10(1) |
| Copy the following to cite this URL: Hassan E. E, Elagab E. A. M, Mohammed H. B, Abdelgader A. EB, Elhussein A. B, Huneif M. A. Distribution of Thyroid Autoantibodies in Saudi Children with type 1 Dm and their effect on Glycemic Control. Biomed Pharmacol J 2017;10(1) Available from: http://biomedpharmajournal.org/?p=13483 |
Introduction
Type1 diabetes mellitus (T1DM) is a chronic autoimmune disease result in destruction of pancreatic beta cells lead to the clinical form of the disease (1). Unfortunately a recent study reported increasing in the incidence of the disease by 2-5% globally (2). However the prevalence in Saudi Arabia is higher in comparison to other communities (3).
Moreover the disease known to be associated with multiple autoimmune diseases worldwide, such as Graves’ disease, Hashimoto’s thyroiditis, Addison’s disease, vitiligo, celiac disease, autoimmune hepatitis, myasthenia gravis, and pernicious anemia . Perhaps the autoimmune thyroid diseases are the commonest (4), estimated about 40% in a cohort study in Germany and Austria (5).
Both autoimmune thyroiditis and type 1 DM are organ specific autoimmune disease mediated by T cells and probably they have same pathogenesis, their accompanied occurrence may explained by sharing some susceptibility genes (6).
The higher prevalence of thyroid autoantibodies as well as abnormal thyroid profiles were detected among type 1 DM children and adolescence, including their first-degree relatives (7) (8).
As far as anti-TPO (Anti-thyroid peroxidase) is a major thyroid autoantibodies (9), and anti-TG (anti-Thyroglobulin antibodies) were most commonly anti-thyroid antibodies associated with anti-pancreatic antibodies Anti-GAD (Anti-glutamic acid decarboxylase). (7). which are mainly linked to females and long standing diabetes (10). Recent studies reported an increase prevalence of thyroid auto antibodies associated with type 1 DM which explained by awareness of doctors about these combinations (10) (11). Hashimoto thyroiditis is commonest clinical presentation among type 1 DM in contrast to Graves’ disease, which is less frequent. Other more still there are contradicted results concerning the distribution of goiter in type1 DM versus non-DM (12). In previous reports low T3 syndrome was detected in the diabetic adolescences group, which were found to be associated with high level of glucose as well as HbA1c, so they recommend to do a serial thyroid function test (T3, T4, TSH) as T3 level may be affected by metabolic control and patient thyroid function (8). On the other hand an increase prevalence of Graves’ disease among type1 DM associated with highly variable ages with patients, lead to a serious illness includes metabolic disturbances as well as adverse pregnancy outcome which results from the association of both diseases in one patient (13).
Although many researches proved the association of auto thyroid antibodies with type1 DM, but there are debates concerning sub clinical thyroiditis and their role in glycemic control as well as disease complication (14) (15)
Saudi children with type1 diabetes known to be have very poor glycemic control that may result in worse diabetic complications (16) other more a new form of diabetes were very common in Saudi adolescence represented about one-third of diabetic patients called double diabetes (T1 DM &T2 DM) ; The patients presented with both features of T1 DM &T2 DM make the glycemic control out of control (17). So the extensive research needed to understand the hidden pathophysiology beyond the problem.
Methods
This is an analytic, hospital based- case control study that was conducted in the Najran University Hospital & the King Khalid Hospital in Najran City- Saudi Arabia from March 2015 to August 2016.
The study samples comprised 132 Saudi children (76Males & 56 females) clinically diagnosed as type 1 diabetes mellitus according to WHO criteria (18); in contrast, 72 healthy volunteers (40 males, 32 females) were involved as a control group. Both groups were age and sex matched and their ages ranged between 2 and 14 years.
Inclusion criteria
Those with other types of diabetes mellitus, thyroid disease, renal disease, liver disease, anaemia and any medication that may be affect the Parameters under study were excluded from this study.
An interview with a questionnaire to obtain the clinical data was done for each participant in this study, clinical history and examination of the test group and the controls were done by physicians working in Najran University Hospital & King Khalid Hospital.
Weight was measured using electronic digital scales. Height was measured using a wall-mounted stadiometer. BMI was subsequently calculated as weight (kg) per height (m2).
In sterile condition and using a local antiseptic for skin following an overnight fast (8-12 hrs), 5mls of venous blood was collected from each participant and separated into 3mls as serum and 2mls as plasma in EDTA tubes. For serum preparation the blood samples were separated after complete clotting by centrifugation at 4000 rpm for 5 minutes and serum was obtained.
From EDTA tubes HbA1c was measured using chromatography technique (boronate affinity chromatography). The sera were used to measure the concentrations of TSH using ELC (Electrochemiluminescen technology) while GAD antibodies, TPO antibodies & TG antibodies were measured by ELISA (Enzyme-Linked Immunosorbent Assay) from abcam –UK.
The results of this study were statistically analyzed using statistical package for social science (SPSS) program. Independent t-test and Persons correlation coefficients were used; significance levels were set at (P < 0.05).
Results
One hundred and thirty two Type 1 diabetic patients and seventy two matched controls were participated in this study. There were no significant differences between the two groups concerning ages & sexes. While children with type 1 diabetes mellitus were found to have significantly lower BMI the healthy control group (17.46 ±1.76 mean ± S.D, versus18.10±1.42, p < 0.009) and HbA1c % was significantly higher in the diabetic group than that of the healthy control group (9.90±1.79 vs. 4.53± 0.46, p < 0.001), which are demonstrated by (table-1).
Table 1: Baseline characteristics of the test group and the control group
| Parameters | Type 1 Diabetic children | Healthy Control children | P value |
| ( mean± SD) | ( mean± SD) | ||
| Age ̸ Year | 10.5 ± 3.92 | 10.6 ± 2.27 | 0.12 |
| BMI Kg ̸ m2 | 17.48 ±1.76 | 18.10 ± 1.42 | 0.009 |
| HbA1c % | 9.90 ± 1.79* | 4.53 ± 0.46 | 0.000 |
BMI: Body Mass Index; HbA1c: Glycated hemoglobin
Data are expressed as means ± S.D.
*Significant p value < 0.05
The study showed a higher distribution of anti-GAD 56.8%, anti-TPO 36.4% and anti-TG 19.7% among patients in contrast to controls 5.6%, 9.7%, and 4.2% respectively. The plasma concentrations of autoantibodies were significantly increased in diabetic patients in compared to controls P value ≤ 0.03 (table -2). Furthermore the plasma concentration of anti-TPO and anti-TG were significantly elevated in anti-GAD positive patients in compare to anti-GAD negative patients (p value ˂ 0.001) (table-3)
Table 2: Distribution of autoantibodies among patients and controls
| Parameters | Type 1 Diabetic children | Healthy Control children | p. value |
| ( mean± SD) | ( mean± SD) | ||
| Anti-GAD (ng/ml) | 7. 30 ± 6.78* | 2.33 ± 1.60 | 0.000 |
| Anti-TPO (U/ml) | 84.92 ± 126.88* | 15.93 ± 31.29 | 0.000 |
| Anti-TG (U/ml) | 16.21 ± 32.51* | 4.48 ± 8.13 | 0.003 |
Anti-GAD: Anti-glutamic acid decarboxylase; Anti-TG: Anti thyroglobulin antibodies; Anti-TPO: anti-thyroid peroxidase antibodies.
Data are expressed as means ± S.D.
*Significant p value < 0.05.
Concerning the association between positive autoantibodies (Anti GAD, anti TPO anti TG) and HbA1C, it made clear that HbA1c is significantly increased, in contrast to negative autoantibodies patients, (P value ˂ 0.001) (table-4).
Table 3: Distribution of thyroid autoantibodies (Anti-TPO & anti-TG) among patients with positive and negative anti-GAD
| Parameters | anti-GAD (ng/ml) | P. value | |
| positive Patients | negative Patients | ||
| N=75 (56.8%) | N= 57(43.2%) | ||
| Anti-TPO (U/ml) | 137.42±145.67* | 15.84±32.76 | 0.000 |
| Anti-TG (U/ml) | 23.22±39.60* | 7.00±15.78 | 0.000 |
Data are expressed as means ± S.D
*Significant p value < 0.05
Table 4: Distribution of HbA1c % among type 1 diabetic patients with positive and negative autoantibodies (Anti-GAD, Anti-TPO, Anti-TG)
| Parameters | Positive | Negative | P Value |
| Anti-GAD (ng/ml) | 10.05± 1.80* | 9.70± 1.78 | 0.000 |
| N=75 (56.8%) | N= 57(43.2%) | ||
| Anti-TPO (U/ml) | 10.36±1.92* | 9.62±1.66 | 0.000 |
| N=48(36.7%) | N=84(63.3%) | ||
| Anti-TG (U/ml) | 10.20±2.03* | 9.82± 1.73 | 0.000 |
| N=26(19.7%) | N=106(80.3%) |
Data are expressed as means ± S.D
*Significant p value < 0.05
The plasma level of TSH concentrations were high in (13/132, 9.8%), low in (2/132, 1.5%) and normal in the remaining patients, in contrast to only (1/72, 1.4%) healthy control who showed high level of TSH. Moreover, there is no significant correlation between HbA1c and TSH in type 1DM (P value =0.808, r = 0.021) (Figure 1)
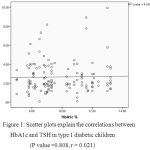 |
Figure 1: Scatter plots explain the correlations between HbA1c and TSH in type 1 diabetic children (P value =0.808, r = 0.021)
|
Discussion
Autoimmune thyroiditis is most common autoimmune condition associated with type1DM. In this work, Auto thyroid antibodies (Anti-TPO, Anti-TG) and anti-GAD were investigated among type1 DM children without any clinical thyroid disorder. Furthermore, HbA1c and TSH were measured in order to investigate the glycemic effect of diabetic patients with autoimmune thyroiditis and to report subclinical thyroid disease respectively. In this study the male children with type1 DM were predominated versus female group, it has been just similar to the previous research from Saudi Arabia(19) and inconsistent with other data from brazil where the female patients were dominant (20). However, gender bias may happen (21). In the present report the prevalence of both autoimmune thyroid antibodies (Anti-TPO, Anti-TG) were (36.4%, 19.7%) among type 1 DM patients, which approximately supported other research findings, where the prevalence of auto thyroid antibodies were about 30% of type1 DM (22). Nevertheless a result of low prevalence was reported in other population, about (17.4%) for anti TPO and (11.1%) for anti-TG (10), reflecting a wide distribution variety of auto antibodies in different populations, that it could be due to different genetic background. While the anti-GAD showed an equal prevalence in many studies from different parts of the globe, (53.2%) (9) (60%), (16), and 56.8% in recent study, indicating the important role of anti-GAD antibodies in type1DM pathogenesis. Other more we demonstrated that the auto thyroid antibodies were strictly positively associated with positive Anti-GAD in compared to negative anti-GAD patients, which were consistent to (Gul et al )(23) and (Shiau et al) reports(24) .
Type1 DM is a chronic autoimmune inflammatory condition, involved induction of beta cells apoptotic gene leads to beta cell destruction , the condition associated with secretion of inflammatory mediators (25). Despite the inflammatory sequences that take place in type1 DM, there were no studies that correlate the association of these auto thyroid antibodies with HbA1c as glycemic marker. On the other hand, inflammatory and infection had been proved to be associated with higher HbA1c of type 2 DM patients (26). IL-6 directly affect hepatocyte insulin receptor to uptake glucose (25). Moreover Th1/Th2 cytokines are highly expressed in type1 diabetic patients, and have been noticing fluctuation in reading across patients age, with high concentration of Th1 cytokines early in disease progression that might be related to type 1DM pathogenesis, while Th2 cytokines considered to be maintained continuous inflammatory conditions as well as it may play roles in disease impactions (27). Furthermore, double diabetes; a new entity, appear to be the state behind uncontrolled blood sugar in young diabetes patients. In the present study, there is significant elevation of HbA1c in positive autoantibodies patients, in contrast to patients with negative autoantibodies. This result could be a breakthrough to link unexplained difficulties to control blood glucose in type 1DM and inflammatory mediators in some children in order to prevent acute and chronic complication of DM. However, more in-depth studies are needed to investigate inflammatory mediators which might be associated with higher HbA1c as well as disease complication. Thyroid dysfunctions are frequently seen among type1 DM, result in horrible impaction on the patients clinical condition, if left untreated (14). Our results revealed about (13/132, 9.8%) subclinical hypothyroid patients with elevated TSH and one subclinical hyperthyroidism with low TSH level. Nevertheless insignificant correlations between HbA1c and TSH were observed in our report. However the HbA1c and TSH were showed to be positively correlated with each other in the previous report, where, subclinical thyroiditis were improved with supplementation of L-thyroxin (28). So multifactorial may share by different way to affect the glycemic controls, for these reasons extensive research needed to subgroup the patients depending on clinical background and laboratory result in order to guide the pediatricians to design an effective management guideline.
Conclusion
Our results state that the distributions of auto thyroid antibodies among type 1 DM patients are high in Saudi children. On the other hand the indirect effect of autoantibodies on glycemic control cannot be excluded; it could be due over expression of inflammatory mediators; an area for further research. Also, according to our finding we recommend to do serial thyroid profile as well as thyroid autoantibodies investigation for type 1DM as a subclinical thyroiditis is not very rare.
Contributors
EEHH concept and design of the study, supervision of the study, analysis and interpretation, manuscript preparation, critical and final revision of the manuscript and literature search. EAME: manuscript preparation and literature search, clinical studies, data acquisition and Laboratory investigations. MAH: concept and design of the study, data collection and clinical studies. HBM: data collection and data acquisition. AEA: data collection, laboratory investigations. ABE: data collection, Laboratory investigations and statistical analysis.
Acknowledgment
This work was funded by a grant from the Deanship of Scientific Research, Najran University, KSA (NU/MID/14/036).
Disclosure
None declared.
Ethical approval
Permission of this study was obtained from research and ethics committee of Najran University, KSA. All patients were assured that all their obtained information will be handled in a confidential atmosphere and it will not affect their life after taking verbal and written consent.
References
- Yoon JW, Jun HS. Autoimmune destruction of pancreatic β cells. American journal of therapeutics. 2005 Nov 1;12(6):580-91.
CorssRef - Mayer-davis EJ. Chapter 1 : Epidemiology of Type 1 Diabetes. Endocrinol Metab Clin North Am . 2010 September ; 39(3): 481–497.
CorssRef - Al-Rubeaan K. National surveillance for type 1, type 2 diabetes and prediabetes among children and adolescents: a population-based study (SAUDI-DM). Journal of epidemiology and community health. 2015 Jun 17:jech-2015.
- Kakleas K, Soldatou A, Karachaliou F, Karavanaki K. Associated autoimmune diseases in children and adolescents with type 1 diabetes mellitus (T1DM). Autoimmunity reviews. 2015 Sep 30;14(9):781-97.
CorssRef - Kordonouri O, Klinghammer A, Lang EB, Grüters-Kieslich A, Grabert M, Holl RW. Thyroid Autoimmunity in Children and Adolescents With Type 1 Diabetes A multicenter survey. Diabetes care. 2002 Aug 1;25(8):1346-50.
CorssRef - Tomer Y, Menconi F. Type 1 diabetes and autoimmune thyroiditis: the genetic connection. Thyroid. 2009 Feb 1;19(2):99-102.
CorssRef - Hanukoglu A, Mizrachi A, Dalal I, Admoni O, Rakover Y, Bistritzer Z, Levine A, Somekh E, Lehmann D, Tuval M, Boaz M. Extrapancreatic Autoimmune Manifestations in Type 1 Diabetes Patients and Their First-Degree Relatives A multicenter study. Diabetes Care. 2003 Apr 1;26(4):1235-40.
CorssRef - Dorchy, H, Bourdoux, P. and Lomiere, B. Subclinical thyroid hormone abnormalities in type 1 diabetic children and adolescents: relationship to metabolic control. Acta Paediatr Scand.1985 May;74(3):386-9.
CorssRef - Chardès T, Chapal N, Bresson D, Bès C, Giudicelli V, Lefranc MP, Péraldi-Roux S. The human anti-thyroid peroxidase autoantibody repertoire in Graves’ and Hashimoto’s autoimmune thyroid diseases. Immunogenetics. 2002 Jun 1;54(3):141-57.
CorssRef - Kakleas K, Paschali E, Kefalas N, Fotinou A, Kanariou M, Karayianni C, Karavanaki K. Factors for thyroid autoimmunity in children and adolescents with type 1 diabetes mellitus. Upsala journal of medical sciences. 2009 Dec 1;114(4):214-20.
CorssRef - Schroner Z, Lazurova I, Petrovicova J. Autoimmune thyroid diseases in patients with diabetes mellitus. Bratislavske lekarske listy. 2007 Dec;109(3):125-9.
- Ardestani SK, Keshteli AH, Khalili N, Hashemipour M, Barekatain R. Thyroid disorders in children and adolescents with type 1 diabetes mellitus in isfahan, iran. Iranian journal of pediatrics. 2011 Dec;21(4):502.
- Greco D, Pisciotta M, Gambina F, Maggio F. Graves’ disease in subjects with type 1 diabetes mellitus: a prevalence study in western Sicily (Italy). Primary care diabetes. 2011 Dec 31;5(4):241-4.
CorssRef - Hage M, Zantout MS, Azar ST. Thyroid disorders and diabetes mellitus. Journal of thyroid research. 2011 Jul 12;2011.
- Al-Rubeaan K. National surveillance for type 1, type 2 diabetes and prediabetes among children and adolescents: a population-based study (SAUDI-DM). Journal of epidemiology and community health. 2015 Jun 17:jech-2015.
- Aljabri KS, Bokhari SA. Glycemic control of patients with type 1 diabetes mellitus in Saudi community. Journal of Diabetes & Metabolism. 2013 May 15;2013.
- Braham R, Robert AA, Mujammami M, Ahmad RA, Zitouni M, Sobki SH, Al Dawish MA. Double diabetes in Saudi Arabia: A new entity or an underestimated condition. World Journal of Diabetes. 2016 Dec 15;7(20):621.
CorssRef - Worled Health Orgnization: Difinition and diagnosis of diabetes mellitus and intermediate hyperglycemia. Report of WHO ̸ IDF consultation, 2006.
- Nasir AM. Al-Jurayyan, Sharifah DA Al Issa, Abdullah NA Al Jurayyan, Hessah MN Al Otaibi and Amir MI Babiker. Thyroid Disorders Associated with Type 1 Diabetes Mellitus in Children and Adolescents from Central Province Saudi Arabia J.Curr.Res.Biosci.Plantbiol.2015.2(1): 45-49.
- Alves C, Santos LS, Toralles MB. Association of type 1 diabetes mellitus and autoimmune disorders in Brazilian children and adolescents. Indian journal of endocrinology and metabolism. 2016 May;20(3):381.
CorssRef - Gale EA, Gillespie KM. Diabetes and gender. Diabetologia. 2001 Jan 1;44(1):3-15.
CorssRef - Prázný M, Skrha J, Limanova Z, Vanickova Z. Screening for associated autoimmunity in type 1 diabetes mellitus with respect to diabetes control. Physiological research. 2005 Jan 1;54(1):41.
- Gul K, Ustun I, Aydin Y, Berker D, Erol HK, Unal M, Barazi AO, Delibasi T, Guler S. Autoimmune thyroid disease in patients with anti-GAD positive type 1 diabetes mellitus. Central European journal of medicine. 2009 Dec 1;4(4):415-22.
CorssRef - Shiau MY, Tsai ST, Hwang J, Wu CY, Chang YH. Relationship between autoantibodies against glutamic acid decarboxylase, thyroglobulin/thyroid microsome and DNA topoisomerase II in the clinical manifestation of patients with type 1 diabetes mellitus in Taiwan. European journal of endocrinology. 2000 Jun 1;142(6):577-85.
CorssRef - Eizirik DL, Mandrup-Poulsen T. A choice of death–the signal-transduction of immune-mediated beta-cell apoptosis. Diabetologia. 2001 Dec 1;44(12):2115-33.
CorssRef - King GL. The role of inflammatory cytokines in diabetes and its complications. Journal of periodontology. 2008 Aug;79(8S):1527-34.
CorssRef - Chatzigeorgiou A, Harokopos V, Mylona-Karagianni C, Tsouvalas E, Aidinis V, Kamper E. The pattern of inflammatory/anti-inflammatory cytokines and chemokines in type 1 diabetic patients over time. Annals of medicine. 2010 Sep 1;42(6):426-38.
CorssRef - Billic-Komarica E, Beciragic A, Junuzovic D. The importance of HbA1c control in patients with subclinical hypothyroidism. Materia socio-medica. 2012;24(4):212.
CorssRef








