Manuscript accepted on :29-07-2024
Published online on: 12-09-2024
Plagiarism Check: Yes
Reviewed by: Dr. Priya Gayathri
Second Review by: Dr. Thirunahari Sravanthy
Final Approval by: Dr. Anton R Keslav
Jayshree Shriram Dawane and Priti Pravin Dhande
and Priti Pravin Dhande
Department of Pharmacology, Bharati Vidyapeeth Deemed To Be University Medical College, Pune, Maharashtra, India.
Corresponding Author E-mail: jayshree.dawane@bharatividyapeeth.edu
DOI : https://dx.doi.org/10.13005/bpj/2967
Abstract
Drakshasava is a formulation used as a general tonic also for anxiety, anaemia in the Ayurveda. Our previous study reports for antidepressant property were very promising. This study aims to elucidate the antidepressant mechanisms of Drakshasava by examining its effects on key neurotransmitters and stress hormones, as well as observing related behavioral changes in Wistar rats under stress models. Methods: Wistar rats weighing 150-200 gms were divided into six groups consisting of 6 rats in each group. Two animal models, acute stress (AS) and unpredictable chronic mild stress (UCMS) were used. Drug treatment was given as per groups orally, Drakshasava in the dose of 2ml & 4ml/kg and Fluoxetine standard comparator 10mg/kg for next 7 days for AS. In UCMS group stress was given for 15 days and drug treatment was given along with the stress from day 15-21. Sucrose preference test (SPT) done on day 0 & 8 in AS and on day 0, 15, 22 in UCMS model rats and at the end Forced Swim test (FST) was performed. Blood withdrawal done for estimation of serum Dopamine, Serotonin and cortisol levels with ELISA kit on day 8 in AS & 22 in UCMS. Data obtained analysed with Graph Pad Prism 6. Result: Decrease in Dopamine (p<0.05) and Serotonin (p<0.01) while increase (p<0.01) in cortisol levels was seen in (depressed) disease control group rats in comparison with control group. Both doses of Drakshasava showed significant reduction in immobility time in FST and improved sucrose preference and was found to be effective in both the models of depression. Increase in serum serotonin (p<0.01) and dopamine (p<0.05) levels was evident while at the same time, (p<0.05) cortisol level reduction was seen in all drug treated rats. Findings observed in the FST and SPT were correlated with the biochemical findings. Effects seen with Drakshasava were comparable with that of Fluoxetine. Conclusion: Drakshasava increased serum serotonin and dopamine levels while decreasing cortisol levels in both acute and chronic animal models of depression. These effects were comparable to those observed with the standard antidepressant drug, Fluoxetine.
Keywords
Cortisol Depression; Dopamine; Serotonin; Unpredictable chronic stress
Download this article as:| Copy the following to cite this article: Dawane J. S, Dhande P. P. Study the Effect of Drakshasava on Dopamine, Serotonin and Cortisol Levels and Behavioural Changes in Acute and Chronic Stress Model in Wistar Rats. Biomed Pharmacol J 2024;17(3). |
| Copy the following to cite this URL: Dawane J. S, Dhande P. P. Study the Effect of Drakshasava on Dopamine, Serotonin and Cortisol Levels and Behavioural Changes in Acute and Chronic Stress Model in Wistar Rats. Biomed Pharmacol J 2024;17(3). Available from: https://bit.ly/3TsBgSx |
Introduction
Both major depression and mania are serious health problems that can profoundly affect an individual’s quality of life if not treated promptly. The modalities used to address these conditions include medication, psychotherapy, and lifestyle modifications, all aimed at managing symptoms and improving overall quality of life. Characteristic symptoms the patient presents with like sad mood, loss of interest in self and surrounding and reduced pleasure in doing the things, reduced initiative and tiredness, worthlessness, guilt, psychomotor retardation or agitation, reduced appetite and sleep, melancholia and suicidal tendency 1. Depression is also associated with substantial impairment of cognitive function, Individuals with depression often experience difficulties with both short-term and long-term memory. They may have trouble recalling recent events or retaining new information. Episodic memory, which is the ability to remember specific events and experiences, is particularly affected.2,3 Mechanism of depression is thought to be an interplay between the three important biochemical substances like Dopamine, Serotonin and cortisol4. Exact mechanism is still uncertain as per recent advances some factors are considered to be responsible for depression are like disturbances in serotonin and norepinephrine neurotransmission. There is interplay between the neurotransmitters norepinephrine, serotonin and dopamine at the nucleus accumbens 5, 6 where decrease in serotonin levels plays a greater role in the occurrence of depression7.
Many mechanisms contributing for the antidepressant effect of the drugs used such as blockade of receptors other than dopamine, monoamine transporters, sleep pattern normalisation, decrease in cortisol levels and increase in neurotrophic growth factors8 At present Antidepressant drugs of first choice are selective serotonin reuptake inhibitors (SSRI), such as fluoxetine, paroxetine, fluvoxamine, citalopram, and sertraline 9. There are many adverse effects but attention required towards the suicidal behaviour and symptoms observed after stopping the drug10,11. The relation between depression and increased cortisol levels is very well understood 12. Currently available drugs like SSRI, Citalopram, Fluoxetine, Fluvoxamine, paroxetine reported to decrease cortisol levels along with having effect on serotonin and dopamine 13.
Drakshasava is prepared from the multiple ingredients, draksha is main along with kumara, dhatkipushpa, kankol, chavak, ranuk, nagpushpa, trijat, lavang, marich, piper, chitrak jatiphal, pipalimoola sugar etc. 14 Our previous research work we evaluated the antidepressant effect of Drakshasava in wistar rats and got very promising results in the unpredictable chronic mild stress model15.Hence, in this study efforts were made to explore the mechanism of action of Drakshasava responsible for reducing the symptoms of depression.
Aim
To investigate the effects of Drakshasava on dopamine, serotonin, and cortisol levels, as well as the associated behavioral changes in Wistar rats under both acute and chronic stress models.
Objectives
To measure the changes in dopamine, serotonin and cortisol levels in Wistar rats subjected to acute and chronic stress after the administration of Drakshasava.
To observe and record behavioral changes in Wistar rats subjected to acute and chronic stress, with and without Drakshasava treatment.
To Investigate the potential mechanisms by which Drakshasava modulates neurotransmitter levels and stress-related behaviors.
Material and Methods
Study was started after obtaining IAEC approval. Wistar rats of weighing 150 – 200 g of both the sex were used for the study. As per the CCSEA guidelines rats were housed in standard cages, temperature and humidity maintained. Food in the form of pellets and aqua guard purified water was given ad libitum. Time for performing the experimental part was maintained same throughout the study.
Six groups of animals were prepared consisting of eight rats in each group. Group 1 was control group treated with saline, Group 2 was disease control exposed to the stress and received saline only, Group 3 &4 were test drug groups received Drakshasava (Low dose) i.e.2ml/kg and (High dose)- 4ml/kg,
Group 5 was standard drug treatment group received Fluoxetine (10 mg/kg) and Group 6 was unpredictable chronic mild stress group received (High dose) – 4ml/kg. All the drugs given orally.
Following tests were carried out for evaluation of antidepressant activity of Drakshasava-
Acute Model of Stress
Forced swim test & Sucrose preference test were done at baseline. Animals received drug treatment as per the groups for 7 days to all the animals of group 3-5, group 1 was control and group 2 was disease control treated with saline. On the day 8 animals were exposed to Forced swim test & Sucrose preference test and blood withdrawal was done for checking the levels of DA, Serotonin & Cortisol.
Sucrose preference was calculated according to the formula:
Sucrose preference = [sucrose intake/ (sucrose intake + water intake)] × 100.
Decrease in the sucrose consumption when given a choice between water and sucrose due to depression and antidepressants reduce anhedonia.
Chronic model of stress
Forced swim test & Sucrose preference test was done at baseline. Animals were exposed to the stress with UCMS for 15 days from group 6. Different stressors were used every day randomly for 3 weeks like: No food for 20 h; No water for 20 h; 24 h crowd (6 rats in one cage) housing, 24 h isolation in separate cages, 45° cage tilt for 17 h, soiled base of the cage for 12 h, constant bright light for 24 h, applying tail clamp for 1 min; and shock from which animal cannot escape. After exposure to every stress rats were returned to the normal conditions until the next stressor was given.
Forced swim test & Sucrose preference test was done on day 15, for next 7 days’ drug treatment given with UCMS. On day 22, animals were exposed to Forced swim test & Sucrose preference test and blood withdrawal was done to estimate dopamine, serotonin & cortisol levels. Blood withdrawal was done after forced swim test by retro orbital method under ketamine anaesthesia for estimation of Dopamine, Serotonin and cortisol levels.
Statistical Analysis
Data collected was analysed with software Graph Pad Prism 6. Results were expressed as mean ± standard error of mean. One-way ANOVA was used to compare the groups followed by post-hoc Tukey’s test was used. P < 0.05 was considered as statistical significance.
Results
Plasma levels of Dopamine, Serotonin and cortisol were estimated in rats of acute and chronic depression. Comparison between the means of serum Dopamine, Serotonin and cortisol levels was done in control, disease control and drug treated rats.
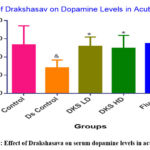 |
Figure 1: Effect of Drakshasava on serum dopamine levels in acute stress |
DS- Disease, DKS LD- Drakshasava low dose, DKS HD- Drakshasava high dose, Fluox- Fluoxetine. Values are represented in the form of mean ± SEM, & p<0.05 data compared with control group findings. *p<0.05 & **p<0.01 in comparison with disease control group.
Dopamine levels were significantly (p<0.05) low in disease control group as compared to control group. In the drug treated groups, dopamine levels were significantly high in DKS LD (p<0.05), DKS HD (p<0.05) as well as Fluoxetine treated group (p<0.01) in comparison with disease control group.
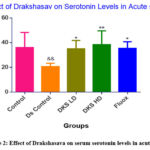 |
Figure 2: Effect of Drakshasava on serum serotonin levels in acute stress |
DS- Disease, DKS LD- Drakshasava low dose, DKS HD- Drakshasava high dose, Fluox- Fluoxetine. Values are represented in the form of mean ± SEM, & p<0.05 data compared with control group findings. *p<0.05 & **p<0.01 in comparison with disease control group.
Serotonin levels in the disease control group were significantly (p<0.01) low in when compared to control group. Increase in serotonin levels was observed in DKS LD (p<0.05) and DKS HD (p<0.01) in comparison with disease control group. Fluoxetine group also showed significant increase (p<0.05) in serotonin level similar to the low dose Drakshasava.
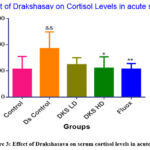 |
Figure 3: Effect of Drakshasava on serum cortisol levels in acute stress |
DS- Disease, DKS LD- Drakshasava low dose, DKS HD- Drakshasava high dose, Fluox- Fluoxetine. Values are represented in the form of mean ± SEM, & p<0.05 data compared with control group findings. *p<0.05 & **p<0.01 in comparison with disease control group.
Significant increase in cortisol levels (p<0.01) was seen in disease control in comparison with control group. Cortisol levels were significantly reduced in comparison in DKS HD (p<0.05). Low dose also showed decrease in the cortisol levels, but it was not statistically significant. Fluoxetine treated group showed (P<0.01) decrease in cortisol levels.
Table 1: Effect of Drakshasava on Immobility Period in Forced Swim Test
|
|
Group |
Dose |
Baseline-Immobility Period (in sec) |
Post treatment- Immobility Period (in sec) |
|
1 |
No stress |
0.5 ml |
51.12 ± 2.08 |
74.87 ±2.29 |
|
2 |
Acute Stress +Saline |
0.5 ml |
50.12 ± 2.75 |
182.87± 3.02&&& |
|
3 |
Acute Stress+ DKS LD |
2ml/kg |
49.00 ±1.73 |
96.00 ± 5.24*** |
|
4 |
Acute Stress+ DKS HD |
4 ml/kg |
48.25 ± 2.61 |
88.37 ± 3.58*** |
|
5 |
Acute Stress+ Fluoxetine |
10 mg/kg |
49.50 ± 2.11 |
92.62 ± 2.78*** |
|
6 |
UCMS (15 d)+ DKS HD with UCMS (7d) |
4 ml/kg |
147.0 ± 4.99*** |
86.87 ± 3.18*** |
DS- Disease, DKS LD- Drakshasava low dose, DKS HD- Drakshasava high dose, Fluox- Fluoxetine.
Values are represented in the form of mean ± SEM, &&& p<0.001 data compared with control group findings. ***p<0.001 in comparison with disease control group.
Significant increase in immobility time (p<0.001) was seen in disease control in comparison with control group. Immobility time was significantly reduced in comparison with disease control in all the drug treated groups.
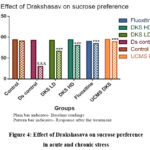 |
Figure 4: Effect of Drakshasava on sucrose preference in acute and chronic stress |
DS- Disease, DKS LD- Drakshasava low dose, DKS HD- Drakshasava high dose, Fluox- Fluoxetine. Values are represented in the form of mean ± SEM, &&& p<0.001 data compared with control group findings. ***p<0.001 in comparison with disease control group.
Significant decrease in sucrose preference (p<0.001) was seen in disease control in comparison with control group. Sucrose preference was significantly increased in comparison with disease control in all the drug treated groups.
Discussion
Many factors are contributing in the pathophysiology of depression like neurotransmitters disturbances and neuroendocrine alterations, genetic factor, real life events 16. Recent research highlights the cause of depression as disturbances in serotonin, dopamine and Norepinephrine neurotransmission17. Dopamine (DA) is found to be involved in the major physiological functions like motivation, psychomotor speed, concentration, and the ability to experience pleasure 18,19 impairment and disturbance of these functions of dopamine is the main features of depression.
Stress in the day to day life in all the age groups has shown the raised levels of blood cortisol and reduces memory and cognitive performance20. Increased levels of cortisol for long duration increases the risk of depression 21. Stress increases corticosteroid levels in circulations and these increased corticosteroids lower the serotonin levels ultimately resulting in depression, aggression and other psychological conditions 22. Interaction between serotonin, dopamine and cortisol is complex, serotonin increases levels of dopamine and reduces cortisol levels showing the beneficial effects23 Cortisol is considered as a culprit resulting increasing in stressful situations and ultimately negatively affecting immune function. Cortisol is a crucial hormone for managing acute stress, but its chronic elevation can have harmful effects, particularly on the immune system. By suppressing immune function and disrupting inflammation regulation, high cortisol levels can increase vulnerability to infections, slow down healing, and contribute to the development of chronic diseases.
There are various models, have been developed to test the antidepressant activity of a new molecule. In our study, to test antidepressant activity, Forced Swim Test that imparts acute stress in animals, and to observe the effect on unpredictable chronic mild stress model of depression was used. Observation showed that there was decrease in the immobility time in forced swim test (Table 1) and sucrose preference was improved significantly (Figure 4) in all drug treated animals proving its efficacy as an antidepressant. The UCMS model encompasses subjecting rodents to a variety of recurrent unpredictable stressors, such as foot shocks, exposure to low temperatures, crowded housing and deprivation of water and food. Stimulate stressful situations to induce behavioural changes in rodents also associated with neuro-inflammation24.Gradual increase in the stress and resultant depression mimics the depression in the human being. Rodents have a natural tendency to drink the weakly sweet solutions of sucrose 25. Animals given sucrose and water in two different bottle and they have choice of selection. Control rats showed a preference for drinking sucrose containing sweet water, but stressed rats lost interest in drinking sucrose water. All drug treated animals showed improved preference to sucrose water. These findings are suggestive of the positive impact of Drakshasava in depression through different mechanism. Here we have showed that it increases the serotonin and dopamine and the cortisol levels are reduced. Since it is a polyherbal preparation consist of various ingredients which may have contributed in reducing stress and ultimately the disturbances in neurotransmitters.
Increase in levels of serotonin and dopamine (Figure-1 & 2) in the drug treated groups, may have resulted in the reduction of immobility time. Drakshasava has different ingredients, few of them have been studied for their use in depression and have been shown to increase the dopamine and serotonin levels. Cardamom oil reduced symptoms of depression in reserpine-injected rats model indicating the positive effect on forced swimming test by reducing immobility and increasing locomotor activities. 26 Linalool present in cardimum which interacts with the monoaminergic system including serotonergic and non-adrenergic system 27. Another ingredient is cinnamon (Cinnamomum burmanii)-cinnamon bark extract improved clinical depression this effect was due to reduction in expression of TNF-alpha in the hippocampus which the viability of serotonin neuronal cells remained optimal and increase in serotonin levels28,29. FST mimics the human symptoms of depression in the form of immobility despair-based behaviour or a stress coping behaviour.
Treatment with Drakshasava decreased cortisol levels significantly (Figure-3) this finding is consistent with our previous study as also by many other studies which report decrease in the cortisol levels with different ingredients of this herbal preparation. Honey is one of the ingredient of Drakshasava and it has been reported in the various studies when honey is used as a vehicle in various preparations it reduces cortisol and ultimately the stress effects, Integrating honey into herbal preparations like Drakshasava may offer a holistic approach to managing stress and promoting overall well-being. 30,31. Similarly, clove ( Syzygium aromaticum ) powder have shown promising antidepressant effects in preclinical studies, and there is emerging evidence suggesting their potential to lower cortisol levels. The antioxidant, anti-inflammatory, and neuroprotective properties of clove compounds, along with their aromatherapeutic effects, may contribute to these beneficial effects. 32,33 and Cardimum also reduces the cortisol levels34.
Considering depression as major health issue and the treatment available is producing insufficient impact due to no response or suboptimal response, sometimes slow response, usually over several weeks of chronic drug treatment; need for new treatment options remains. Due to the resistant depression and limitations of the present drugs, depression research has moved towards the compounds that target non-monoaminergic molecular structures 35. So, in this study, Drakshasava which has shown its efficacy in the experimental models as well as on the biochemical parameters, can prove to be one such promising add on drug in the treatment of depression.
Conclusion
Drakshasava increased serum dopamine, Serotonin levels and decreased cortisol in both the animal models of depression. The biochemical findings show the correlation with the test results. Which was comparable with the standard drug fluoxetine. Drakshasava, through its modulation of key neurotransmitters and reduction of cortisol levels, shows promise in managing stress and its associated symptoms. By increasing serum levels of serotonin, dopamine and decreasing cortisol, Drakshasava may help to alleviate anxiety and depression, improve cognitive function, and enhance overall well-being.
Acknowledgement
Authors are grateful to theBharati Vidyapeeth (DU) Medical College, Pune for providing infrastructure and the help of the animal house staff for this research work.
Conflict of Interest
There is no conflict of interest.
Funding Sources
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Tripathi, K. D. Essentials of medical pharmacology. JP Medical Ltd, 2013, 8th edition,462-480.
CrossRef - Rock, P.L., Roiser, J.P., Riedel, W.J., & Blackwell, A.D. Cognitive impairment in depression: a systematic review and meta-analysis. Psychological Medicine.2014;44(10), 2029-2040.
CrossRef - Snyder, H.R. Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychological Bulletin.2013;139(1), 81-132.
CrossRef - Carneiro, Lara SF, et al. Monoamines and cortisol as potential mediators of the relationship between exercise and depressive symptoms. European archives of psychiatry and clinical neuroscience. 2017; 267:117-121.
CrossRef - Zangen A, Nakash R, Overstreet DH, Yadid G. Association between depressive behavior and absence of serotonin–dopamine interaction in the nucleus accumbens. Psychopharmacology. 2001; 155:434-9.
CrossRef - Nutt, David J. Relationship of neurotransmitters to the symptoms of major depressive disorder. J Clin psychiatry. 2008; 69:4-7.
- Sentari M, Harhap U, Sapiie TW, Ritarwan K. Blood cortisol level and blood serotonin level in depression mice with basil leaf essential oil treatment. Open access Macedonian journal of medical sciences.2019 ;7(16):2652.
CrossRef - Šagud, Marina, et al. Antipsychotics as antidepressants: what is the mechanism? Psychiatria Danubina. 2011;23(3):302-307.
- Masand P.S.; Gupta S. Selective serotonin-reuptake inhibitors: an update. Harvard review of psychiatry. 1999; 7(2): 69-84.
CrossRef - Brent, David A. Selective serotonin reuptake inhibitors and suicidality: a guide for the perplexed. The Canadian Journal of Psychiatry. 2009;54(2): 72-74.
CrossRef - Ebmeier KP, Donaghey C, Steele JD. Recent developments and current controversies in depression. The Lancet. 2006;14;367 (9505):153-67.
CrossRef - Mihaljević-Peleš, Alma, et al. Do we need new therapeutic strategies for depression? Psychiatria Danubina, 2011;23(3):300-301.
- Ronaldson A, Carvalho LA, Kostich K, Lazzarino AI, Urbanova L, Steptoe A. The effects of six-day SSRI administration on diurnal cortisol secretion in healthy volunteers. Psychopharmacology. 2018;235:3415-22.
CrossRef - Tiwari, Preeti. Antimicrobial activity of drakshasava prepared by traditional and modern methods. Research Journal of Pharmacognosy and Phytochemistry.2014;6 (3):126-128.
- Dawane J.S. et al. Evaluation of antidepressant effect of Drakshasava in Wistar rats. International Journal of Green Pharmacy. 2022; 16(4):355-360.
- Pasquini, M B., Isabella B. M. Ethiopathogenesis of depressive disorders. Clinical practice and epidemiology in mental health. 2014;(10): 166.
CrossRef - Zangen, A., Nakash, R., Overstreet, DH, Yadid, G. Association between depressive behavior and absence of serotonin–dopamine interaction in the nucleus accumbens. Psychopharmacology. 2001; 155 :434-439.
CrossRef - Dunlop, B.W., Nemeroff C. B. The role of dopamine in the pathophysiology of depression. Archives of general psychiatry.2007; 64(3): 327-337.
CrossRef - Upthegrove, Rachel; Marwaha, Steven; Birchwood, Max. Depression and schizophrenia: cause, consequence, or trans-diagnostic issue?. Schizophrenia bulletin. 2017; 43(2): 240-244.
CrossRef - Wolf, O.T., et al. The relationship between stress induced cortisol levels and memory differs between men and women. Psychoneuroendocrinology.2001, 26;7: 711-720.
CrossRef - Herbert, J. Cortisol and depression: three questions for psychiatry. Psychological medicine. 2013; 43 ( 3): 449-469.
CrossRef - Pretorius, Ε. Corticosteroids, depression and the role of serotonin. Reviews in the Neurosciences, 2004;15 (2): 109-116.
CrossRef - Field, Tiffany, et al. Cortisol decreases and serotonin and dopamine increase following massage therapy. International Journal of neuroscience. 2005;115(10):1397-1413.
CrossRef - Farooq, Rai Khalid, et al. Is unpredictable chronic mild stress (UCMS) a reliable model to study depression-induced neuroinflammation ?. Behavioural brain research. 2012;231(1):130-137.
CrossRef - Hoffman, Kurt L. New dimensions in the use of rodent behavioral tests for novel drug discovery and development. Expert Opinion on Drug Discovery. 2016;11(4):343-353.
CrossRef - Abdel-Rasoul, Alaa A., et al. Cardamom oil ameliorates behavioral and neuropathological disorders in a rat model of depression induced by reserpine. Journal of Ethnopharmacology. 2023;308 :116254.
CrossRef - Singh, Mansi; Kumar, Sanjesh. Pharmacological screening and effect of Elettaria cardamomum extract on depression-like behaviour in rat model. Pharma Innov. J. 2019; 8( 8):401-404.
- Parisa, Nita, et al. Antidepressant effect of cinnamon (Cinnamomum burmannii) bark extract in chronic stress-induced rats. Open Access Macedonian Journal of Medical Sciences. 2020; 8: 273-277.
CrossRef - Amin, Chris Alberto, et al. The Potential of Cinnamon as Anti-Depressant. Eureka Herba Indonesia.2021; 2(2):95-99.
CrossRef - Kumalasary, Fitri, et al. The Effect of Giving Moringa Honey on Stress and Cortisol Levels in Pregnant Women in Maros Regency. Turkish Journal of Computer and Mathematics Education. 2021; 12(14):2669-2676.
- Usman, Andi Nilawati, et al. Glucocorticoid and cortisol hormone in response to honey and honey propolis supplementation in mild stress women. Enfermería Clínica.2020; (30):1-4.
CrossRef - El-Bouhy, Zeinab, et al. The Immuno-Antioxidant and Anti-bacterial Effects of Clove Powder on Proteus mirabilis Challenge in Oreochromis niloticus: A Comparative Study with Cephalexin Antibiotic. Zagazig Veterinary Journal. 2022;50 (4):335-349.
CrossRef - Mittal, Monika, et al. Phytochemical evaluation and pharmacological activity of Syzygium aromaticum: a comprehensive review. Int J Pharm Pharm Sci.2014; 6( 8): 67-72.
- Isaza, Adrian. Nutraceuticals to decrease cortisol and hyperglycemia. In: Functional Foods and Nutraceuticals in Metabolic and Non-Communicable Diseases . Academic Press, 2022: 771-782.
CrossRef - Ionescu, Df; Papakostas, GI Experimental medication treatment approaches for depression. Translational psychiatry. 2017; 7(3): e1068-e1068.
CrossRef







