Adrián Cano-Padilla1 , Jesús Estrada-Hernández1
, Jesús Estrada-Hernández1 , Gilberto Flores-Vargas2
, Gilberto Flores-Vargas2 and Nicolás Padilla-Raygoza2*
and Nicolás Padilla-Raygoza2*
1Service of General Surgery, Hospital General León, Institute of Public Health from Guanajuato State.
2Department of Research and Technological Development, Directorat6e of Teaching and Research, Institute of Public Health from Guanajuato State.
Corresponding Author E-mail: npadillar@guanajuato.gob.mx
DOI : https://dx.doi.org/10.13005/bpj/2766
Abstract
The case is a female 73 years old, with a history of laparoscopic cholecystectomy ten years ago, and is diagnosed with de novo choledocholithiasis. The medical staff conducted two Endoscopic Retrograde CholangioPancreatographies (ERCP). The results of the first one were unresolved choledocholithiasis, endoscopic sphincterotomy, intra and extrahepatic bile duct dilation, and plastic biliary prosthesis placement. In the second one, the results showed an ampulla of Vater with endoprosthesis in situ, which was removed easily. Besides, it was tried to trap the stone with a basket, without success due to dimensions (>45 mm). A Tannenbaum-type biliary stent was placed to ensure biliary drainage. After, the patient was scheduled for a laparoscopic bile duct exploration, and dissection was performed during the surgical procedure until locating a dilated common bile duct of approximately 3 cm. The stone was removed with laparoscopic forceps. Choledochorrhaphy was performed, and a drain was placed.
Keywords
Choledocholithiasis de novo; cholecystectomy; Laparoscopic procedure; Surgery
Download this article as:| Copy the following to cite this article: Padilla A. C, Hernández J. E, Vargas G. F, Raygoza N. P. Large Element De Novo Choledocholithiasis: A Case Report. Biomed Pharmacol J 2023;16(3). |
| Copy the following to cite this URL: Padilla A. C, Hernández J. E, Vargas G. F, Raygoza N. P. Large Element De Novo Choledocholithiasis: A Case Report. Biomed Pharmacol J 2023;16(3). Available from: https://bit.ly/3REZUj0 |
Introduction
Choledocholithiasis is defined by the presence of stones in the main bile duct. It is classified as primary (85%) or secondary, according to the etiology of the stone. The prevalence of choledocholithiasis in patients with lithiasic cholecystitis reported in the American Society for Gastrointestinal Endoscopy (ASGE) and European Society for Gastrointestinal Endoscopy (ESGE) guidelines is 8% to 18% 1,2. In Mexico, the proportion is 5% to 10% 3.
Primary choledocholithiasis is defined by the criteria of Saharia et al. 4, which consists of previous cholecystectomy, absence of signs of bile duct obstruction for two years, presence of an ovoid, soft, or friable calculus, and no long remnant of the cystic duct. The average time for the appearance of primary cholelithiasis after cholecystectomy is between 8 and 12 years 5.
Within the classification of gallstones, there is a precise definition for stones that are difficult to manage with criteria such as diameter greater than 15 mm, stone impaction, and periampullary diverticulum, which influence the difficulty and therapeutic failure for the extraction of stones in the common bile duct 6,7. In 10% to 20% of cases, stone extraction is not achieved using conventional endoscopic techniques, and it requires instrumentation with different ones such as Litotripsy mechanical, extracorporeal, and electro-hydraulic 8.
Finally, if stone extraction is not achieved with the previously described techniques, there is a need for laparoscopic or open surgical exploration of the bile duct 9. The absolute frequency of the need for surgical exploration of the bile duct in patients with giant choledocholithiasis is approximately 10% 1.
Presentation of the case
The case was a 73-year-old female with a history of important laparoscopic cholecystectomy ten years ago. She referred to having been approached in a health center by those who diagnosed choledocholithiasis de novo. It was referred to the endoscopy service of the General Hospital of León, and two Endoscopic Retrograde CholangioPancreatographies (ERCP) were performed in this unit.
ERCP with findings: unresolved choledocholithiasis, endoscopic sphincterotomy, intrahepatic and extrahepatic bile duct dilation; placement of a plastic biliary prosthesis
 |
Figure 1: First ERCP |
ERCP with findings: ampulla of Vater with a stent in situ. It was removed without difficulty. An attempt was made to catch the stone with a basket without success due to dimensions (>45 mm). A Tannenbaum-type biliary stent was placed to ensure biliary drainage.
 |
Figure 2: Second ERCP |
Subsequently, she went to the general surgery clinic, where the patient was diagnosed with a de novo choledocholithiasis of large elements. Therefore, she was sent to the third level unit for electrohydraulic intraductal lithotripsy without obtaining a satisfactory response for administrative reasons. The patient was scheduled for laparoscopic bile duct exploration.
During the surgical procedure, dissection was performed until a dilated common bile duct of approximately 3 cm was located.
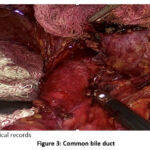 |
Figure 3: Common bile duct |
A 4 cm longitudinal choledochotomy was performed, with abundant biliary debris coming out. Also, a 12 Fr Foley catheter was introduced, and an attempt was made to drag the stone without success.
 |
Figure 4: Foley catheter in choledochotomy for stone removal |
A video-gastroscope was inserted through a 12-mm trocar. As choledochotomy was approached, a 30-mm stone was seen towards the distal common bile duct. The extraction with Dormi failed due to the size of the stone. An extractor balloon was inserted, disimpacted, and brought closer to the supraduodenal portion for subsequent laparoscopic extraction. Proximal and distal vacuity was verified.
 |
Figure 5: Video-gastroscope in choledochotomy |
Finally, the stone was removed with laparoscopic forceps; Choledochorrhaphy was performed, and a drain was placed.
 |
Figure 6: Stone of large elements outside the common bile duct |
Primary large-element choledocholithiasis is a therapeutic challenge for the general surgeon and endoscopist. The biliodigestive bypass should be reserved for select patients 10.
All the guidelines recommend that choledocholithiasis patient management should be adapted to the resources available in each institution 1. In this case, it was decided to perform laparoscopic bile duct exploration with the support of intraoperative choledochoscopy, obtaining the successful extraction of the stone in the common bile duct.
It is important to note that, during the surgical procedure, multiple attempts were made to extract the stone from the bile duct since its size prevented its easy handling for extraction. Finally, it was achieved with the support of the endoscopy service.
The surgeon’s decision to perform laparoscopic bile duct exploration was crucial for managing this case since the stone extraction by ERCP failed on two previous occasions. Therefore, it was decided to perform a laparoscopic procedure.
Conclusion
It is established that endoscopic management should be the first guideline for its treatment without neglecting the possibility of surgical resolution. Laparoscopic management is a feasible option if there is experience and resources for its performance and choosing the surgical procedure having the greatest success described in the literature, currently with lower morbidity and mortality for the patient.
Acknowledgement
The authors thanks to the patient to give us the consent form signed for her to publish her clinic images.
Conflict of interest
All authors declare not to have conflict of interest.
Funding Source
There is no funding sources
References
- ASGE Standards of Practice Committee, Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, et al. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019;89(6):1075-1105.e15. DOI: https://doi.org/10.1016/j.gie.2018.10.001
CrossRef - Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2017;102(8):1781-8. DOI: https://doi.org/10.1111/j.1572-0241-2007.01279.x
CrossRef - Bolivar-Rodríguez MA, Pamanes-Lozano A, Corona-Sapien CF, Fierro-López R, Cázarez-Aguilar MA. Coledocolitiasis. Una revision. Rev Med UAS. 2017; 7 (3): 138-154. DOI: http://dx.doi.org/10.28960/revmeduas.2007-8013.v7.n3.005
CrossRef - Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P et al. Endoscopic management of CBD stones. Endoscopy. 2019; 51: 472-491. DOI: https://doi.org/10.1055/a-0862-0346
CrossRef - Wilkins T, Agabin E, Varghese J, Talukder A. Gallbladder Dysfunction: Cholecystitis, Choledocholithiasis, Cholangitis, and Biliary Dyskinesia. Prim Care. 2017;44(4):575-597. DOI: https://doi.org/10.1016/ j.pop.2017.07.002
CrossRef - Ramírez-Garcia J. Factores Relacionados con la Falla Terapéutica en la Extracción de Cálculos Coledocianos por Pancreatocolangiografía Retrógrada Endoscópica. Revista Peruana de Gastroenterologia. 2011; 31: 330 – 34. DOI: https://doi.org/10.47892/rgp.2011.314.361
- Katanuma A, Maguchi H, Osanai M, Takahashi K. Endoscopic treatment of difficult common bile duct stones. Digestive Endoscopy 2020; 22 (Supl.1): S90–S97. DOI: https://doi.org/10.1111/j.1443-1661.2010.00979.x
CrossRef - Park CH, Jung JH, Nam E, Hye Kim E, Gang Jim M, Hyun Kim J, et al. Comparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: a network meta-analysis. Gastrointest Endosc 2018;87:43-57. DOI: https://doi.org/10-1016/j.gie.2017.07.038
CrossRef - Sun SX, Kulaylat AN, Hollenbeak CS, Soybel DI. Cost-effective decisions in detecting silent common bile duct gallstones during laparoscopic cholecystectomy. Ann Surg 2016; 263:1164-72. DOI: https://doi.org/10.1097/SLA.0000000000001348
CrossRef - He H, Tan C, Wu J, Dai N, Hu W, Zhang Y, et al. Accuracy of ASGE high-risk criteria in evaluation of patients with suspected common bile duct stones. Gastrointest Endosc 2017; 86:525-32. DOI: https://doi.org/10.1016/j.gie.2
CrossRef







