Nahla L. Faizo1, Bassem M. Raafat1 , Sultan Alamri1
, Sultan Alamri1 , Ahmad Joman Alghamdi1
, Ahmad Joman Alghamdi1 , Hamid Osman1
, Hamid Osman1 , Rania Mohammed Ahmed1
, Rania Mohammed Ahmed1 , Ashraf Almahwasi2
, Ashraf Almahwasi2 , Abdulhakeem S. Alamri3,4
, Abdulhakeem S. Alamri3,4 and Mukhtar Ansari5*
and Mukhtar Ansari5*
1Department of Radiological Sciences, College of Applied Medical Sciences, Taif University, Taif 21944, Saudi Arabia.
2Medical Physics Unit, Security Forces Hospital, Medical Services, Ministry of Interior, Makkah, The Kingdom of Saudi Arabia.
3Department of Clinical Laboratory Sciences, College of Applied Medical Sciences, Taif University, Taif, Saudi Arabia.
4Centre of Biomedical Sciences Research (CBSR), Deanship of Scientific Research, Taif University, Saudi Arabia
5Department of Clinical Pharmacy, College of Pharmacy, University of Hail, Hail, Saudi Arabia.
Corresponding Author E-mail: m.ansari@uoh.edu.sa
DOI : https://dx.doi.org/10.13005/bpj/2436
Abstract
Background: Breast cancer is the most frequent cancer among women throughout the world. A range of noninvasive techniques have been employed for early prevention. In health-care practice, however, quality and sensitivity remained critical. Objective: The aim of this study is to see how well Breast Magnetic Resonance Imaging (MRIs) and Dynamic Contrast-Enhanced MRI (DCE-MRI) techniques can detect breast cancer and distinguish between malignant and benign lesions. Methods: A retrospective study was conducted at the Taif Hospitals, Saudi Arabia. The Picture Archiving and Communication System was used to acquire medical records and data from 50 individuals with probable breast cancer, and breast MRI pictures were analyzed. Breast Imaging Reporting and Data System (BI-RADS) radiologist reports and DCE-MRI kinetic curves were evaluated. Excel was also used to test the sensitivity and specificity of breast MRI. Results: According to the BI-RADS results, biopsies, and breast MRI data, 52 percent of 50 patients were categorized as benign, 24 percent as malignant, and 24 percent had no abnormalities. Biopsy revealed that 61.5 percent of the malignant lesions were benign, whereas 38.5 percent were appropriately identified as cancerous. The majority of malignant tumors were discovered in patients over the age of 50. The washout curve correctly identified 60% of the malignant lesions and 40% of the benign lesions. Our data demonstrated the usefulness of MRI in detecting breast cancers by analyzing BI-RADS and utilizing DCE-MRI. False-positive, on the other hand, can lead to unnecessary biopsies. Conclusion: Breast cancer is more common among women of their fifties and beyond. Biopsies, breast MRIs, and kinetic curve analysis can all be utilized to differentiate between benign and malignant breast masses with high sensitivity and specificity.
Keywords
Breast Cancer; Magnetic Resonance Imaging; Negative Results; Saudi Arabia; Sensitivity; Specificity
Download this article as:| Copy the following to cite this article: Faizo N. L, Raafat B. M, Alamri S, Alghamdi A. J, Osman H, Ahmed R. M, Almahwasi A, Alamri A. S, Ansari M. Distinction of Breast Masses from Benign to Malignant using Magnetic Resonance Imaging and Dynamic Contrast-Enhanced in Tertiary Care Hospitals of Taif, Saudi Arabia: A Retrospective Study. Biomed Pharmacol J 2022;15(2). |
| Copy the following to cite this URL: Faizo N. L, Raafat B. M, Alamri S, Alghamdi A. J, Osman H, Ahmed R. M, Almahwasi A, Alamri A. S, Ansari M. Distinction of Breast Masses from Benign to Malignant using Magnetic Resonance Imaging and Dynamic Contrast-Enhanced in Tertiary Care Hospitals of Taif, Saudi Arabia: A Retrospective Study. Biomed Pharmacol J 2022;15(2).Available from: https://bit.ly/3Mk4OeV |
Introduction
Breast cancer is the most prevalent malignancy among women worlwide, and it is the second most common cancer among Saudi women, with a prevalence of 21.8 percent.1,2 Breast cancer is the ninth leading cause of death among Saudi Arabian women, according to recent studies on cancer-related mortality.3 Breast cancer has been garnering attention among clinicians, researchers, and communities as a public health concern.4 Breast cancer is the most prevalent newly diagnosed malignancy among women in Saudi Arabia, with an increasing incidence rate.5
According to the Saudi Cancer Registry, about 930 new cases of breast cancer are detected in Saudi Arabia each year.6 Changes in breast shape or size, the presence of a palpable lump, puckering or dimpling indicating abnormal skin texture, redness or rashes on the skin or surrounding the nipple, retracted nipples, spontaneous secretions from the nipple, or swelling in the axial region are all possible sypmptoms.7 These changes, however, are not specific to breast cancer as they can be mimicked by benign breast lesions due to fibrocystic changes and surrounding the nipple, retracted nipples, spontaneous secretions from the nipple, or swelling in the axial region are all possible sypmptoms.7 These changes, however, are not specific to breast cancer as they can be mimicked by benign breast lesions due to fibrocystic changes and mastitis. However, in some circumstances, benign breast tumors may increase the risk of developing breast cancer.8
Breast cancer mortality has been reduced dramatically due to advances in imaging technology.9 Suspicious breast imaging findings may range from malignant, indeterminate-to-high risk, benign, and equivocal anomalies. For breast cancer screening and diagnosis, magnetic resonance imaging (MRI) of the breast is typically utilized in conjunction with mammograms or ultrasounds. Breast MRIs are used for assessing women who have been diagnosed with breast cancer using other diagnostic methods such as biopsies or lumpectomies. These MRIs can be used to determine the size of a tumor, scan for other breast tumors, and disclose tumors in the opposite breast, and aid in disease management.10-12 Breast MRIs have a diagnostic sensitivity range of 93% to 100%. However, since numerous benign lesions show enhancement or other unusual findings on MRI, their main drawback is their low specificity.13
Dynamic contrast-enhanced MRI (DCE-MRI) of the breast is being employed for a number of clinical applications, including evaluating the extent of malignant diseases and improving specificity when characterizing breast lesions.14, 15 DCE-MRI is a perfusion imaging technique that maps new vasculature and has been shown to be a highly sensitive method for detecting breast cancer. However, because it has a wide specificity range of 21% to 100%, it has sparked debate. On DCE-MRIs of the breast, the type of the contrast-enhanced kinetic curve shown can be used to predict malignancy.16 The type of curve is estimated quantitatively for the interpretation of DCE-MRI, with wide variability in the inter and intra-observer.17, 18
The Breast Imaging Reporting and Data System (BI-RADS) is the most commonly utilized interpretation criteria, according to the American College of Radiology.19, 20 The BI-RADS is a standard language for reporting MRI findings from different institutions throughout the world. The purpose of the BI-RADS atlas program is to provide a standard reporting, classification, monitoring, and diagnostic work-up of breast cancer.21, 22 According to the imaging characteristics, BI-RADS classifies breast lesions into groups 2 through 5 based on imaging criteria. Category 4 or 5 lesions are indicated for tissue biopsy. Category 4 is further subdivided into 4A, 4B, and 4C, which reflect the increasing chances of malignancy as low (> 2% but ≤ 10%), moderate (> 10% but ≤ 50%), and high (> 50% but < 95%). These sub-categories have greater therapeutic relevance as discordant radiologic-pathologic correlation directs persistent diagnostic dilemmas.
As breast cancer has become more prevalent, it demands more attention and research. MRI is being utilized as a supplement to other methods of evaluating breast cancers. However, because of their high sensitivity, there is growing interest in employing MRIs for diagnostic purposes. As a result, the goal of this study was to see how efficient breast MRIs and DCE-MRIs are at detecting breast malignancies and distinguishing between benign and malignant lesions.
Materials and Methods
This retrospective study was conducted in the radiology departments of different hospitals of Taif from February to March 2021. The Institutional Review Board of the Armed Forces Hospitals of the Taif region granted ethical approval for this study. The study comprised medical records from 50 patients who were suspected of having breast cancer based on clinical examinations and were referred to the MRI department regardless of comorbidities. All cases, excluding pregnant women, underwent clinical assessment, biopsy, breast MRI, and a DCE-MRI.
Medical records and the Picture Archiving and Communication System program were used to gather patient information. The patient’s age, disease symptoms, and diagnosis, as well as BI-RADS and the MRI kinetic curve were all acquired. According to the American College of Radiology’s BI-RADS-MRI reports, the description of lesion architecture and enhancement characteristics was classified into six categories: 1 (negative result, completely free of cancer); 2 (benign), 3 (likely benign), 4 (suspicion of malignancy), 5 (highly suggestive of malignancy), and 6 (proven malignancy).
Normal, benign, and malignant diagnoses were extracted from the breast MRI data. The DCE-MRI data were assessed based on the visualization of three dynamic contrast-enhancement curves: the enhancing curve (typically showing a continuous increase in signal intensity over time), the plateau curve (considered concerning for malignancy), and the washout curve (strongly suggestive of malignancy). We assessed the positive predictive values (PPVs) and negative predictive values (NPPs) based on confirmed diagnoses obtained through biopsies to evaluate the sensitivity and specificity of the breast MRIs in detecting breast cancer. The data was first entered into an Excel sheet before being imported to IBM SPSS Statistics V21.0 for analysis.
Results
Patients’ ages ranged from 24 to 76 years, and they were categorized into four groups: (18<30, 30–40, 41–50, and >50 years). When the BI-RADS classifications from the breast MRIs were reviewed, the highest percentage of patients (30%) fell into category three, while the lowest percentage slide into category six (2 percent ) (Figure 1).
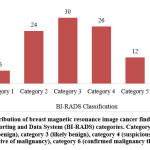 |
Figure 1: Distribution of breast magnetic resonance image cancer findings by Breast Imaging Reporting and Data System (BI-RADS) categories. |
After reviewing the reports of 13 suspected breast cancer cases (category 4 BI-RADS classification) and following their biopsy results, we found that 61.5% (eight patients) had benign lesions and 38.5% (five patients) had cancerous lesions. Following biopsies for all cases, 52% (26 patients) had benign tumors, 24% (12 patients) had cancer, and 24% (12 patients) had no lesions.
Table 1 shows the link between age groups and diagnoses based on MRI findings and biopsies. The 30–40 years age group had the most benign lesions (50%). Those over 50 years old (58.3%), had the most cancerous lesions, followed by women in the 41–50 years age range (33.3%) and those in the 30–40 years age group (8.3%).
Table 1: Relationship between age groups and diagnoses.
| Age group (in years) | Diagnosis | Total percentage | ||
| Normal | Benign | Cancerous | ||
| 18–<30 | 0% | 7.7% | 0% | 4.0% |
| 30–40 | 33.3% | 50.0% | 8.3% | 36.0% |
| 41–50 | 25.0% | 26.9% | 33.3% | 28.0% |
| >50 | 41.7% | 15.4% | 58.3% | 32.0% |
The washout curve identified 60% of the cancerous lesions compared to 40% of the benign lesions when cancer assessments were made using kinetic curve data. The plateau curve identified 57.2% of the benign lesions, 35.7% of the cancerous lesions, and 7.1% of the normal cases. As indicated in Table 2, the persistently enhancing curve revealed a higher percentage of benign lesions (53.8%) than normal patients (42.4%).
Table 2: Kinetic curve assessment for normal, benign, and cancerous lesions.
| Assessment | Kinetic Curve Types | Total | ||
| Persistently Enhancing | Plateau | Washout | ||
| Normal lesions | 42.4% | 7.1% | – | 24.0% |
| Benign lesions | 53.8% | 57.2% | 40.0% | 52.0% |
| Cancerous lesions | 3.8% | 35.7% | 60.0% | 24.0% |
In this study, we looked at the sensitivity and specificity of breast MRIs. Based on the final diagnosis, 38 of the 50 lesions investigated were non-cancerous, while 12 were proven to be malignant. Twenty patients were MRI-diagnosed as having cancer (positive); however, after biopsies, eight were found to be cancer-free (false-positive). All 30 individuals who were rated as negative were, however, appropriately identified as such (true negatives). As indicated in Table 3, the MRI has a high sensitivity of 100% (all 12 patients assessed as positive were true positives) and a low specificity of 78.9% (eight out of 20 patients were wrongly diagnosed as having cancer).
Table 3: The sensitivity and specificity of magnetic resonance imaging (MRI).
|
Diagnosis |
MRI Assessment | Total | |||
| Positive
n (% within outcome) |
Negative
n (% within outcome) |
||||
|
Outcome |
True negative | 8 (21.1%) | 30 (78.9%) | 38 (100%) | |
| True positive | 12 (100%) | 0 (0%) |
12 (100%) |
||
Discussion
This study primarily aimed to evaluate the role of DCE-MRIs in breast cancer detection. We found that the majority of the cancer-free cases were classified as persistently enhancing, with no washout cases. The majority of the cancer cases, on the other hand, were classed as washout, with no cases classified as persistently enhancing. The washout type is more likely to be observed with malignant lesions, whereas the consistently enhancing type is more likely to be observed with benign lesions or normal breasts. Our findings indicate that DCE-MRIs can detect and diagnose malignant lesions independently of other lesions. These findings were consistent with prior research that demonstrated that employing DCE-MRI increased the sensitivity and specificity of breast MRIs.17, 23-24 As a result, our findings suggest that the washout curve is largely linked to malignant tumors.
The BI-RADS was created to minimize the disparity amongst professions when it came to reporting MRI findings.25-26 We noticed that most malignant breast tumors were highly vascular and easily detected in contrast-enhanced MRIs after reviewing the BI-RADS classification. Malignant tumors were identified in 8.3% of cases in category 6, 50% in category 5, and 41.7% in category 4. However, there was a significant overlap between benign and malignant lesions, particularly in category 4, which could be attributed to the fact that many benign lesions are hyper-vascular, which can complicate breast MRI interpretetaion and lead to considerable false-positive results. The existence of non-mass lesions is another cause of false-positive results in category 4.21, 27 Therefore, this finding implies that these MRIs are sensitive but not specific. MRIs, despite their low specificity, remain a significant tool for the identification of breast cancer, according to our findings. However, in these instances, the focus will be on correcting false negatives, which may result in unnecessary biopsies, follow-ups, and anxiety for patients. The tumor cellularity and permeability of the basal membrane may have a considerable influence on the lesion signal seen on DCE-MRI, emphasizing the biological aspects of the lesion.
Previous studies reported that the final assessment should be based on the number of major or minor suspicious findings demonstrated.28,29 Thus, lesions in category 5 were characterized as having two or more major suspicious features, while those in category 4 had only one major suspicious feature, with or without minor suspicious features. Furthermore, these investigations suggested that imaging findings alone should not be used to make a final diagnosis. However, there are no well-established procedure for making final decisions or identifying findings that would lead to a lesion being categorized into a certain category. Clinical information such as age, personal history, multiplicity, symptoms and signs may impact the radiologist’s decisions for categorizing these breast lesions. Several studies like those by Gity et al. and Mahoney et al., concur with our findings, confirming that MRIs have a high sensitivity and low specificity.30-31
The study had several flaws including a limited sample size and the fact that it was only undertaken in one Saudi Arabian city. As a result, a larger prospective study with more participants from various cities across the Kingdom is advised.
Conclusion
Women in their fifties and beyond are more likely to get breast cancer. MRI was found to be the most sensitive method for distinguishing malignant from benign breast masses, with DCE-MRI having the highest specificity. Biopsies, breast MRIs, and DCE-MRI kinetic curve analysis can all be used with high sensitivity and specificity to distinguish between malignant and benign breast masses.
Acknowledgment
The research leading to these results received funding from the Deanship of Scientific Research of Taif University.
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Funding Sources
Contents of this research work was funded by the Deanship of Scientific Research, Taif University [Grant No 1-441-109].
References
- Alotaibi R. M, Rezk H. R, Juliana C. I, Guure C. Breast cancer mortality in Saudi Arabia: Modelling observed and unobserved factors. PLoS One, 2018; 13: e0206148.
CrossRef - Tong C. WS, Wu M, Cho W. CS, To K. KW. Recent advances in the treatment of breast cancer. Front Oncol, 2018; 8:227.
CrossRef - El Bcheraoui C, Basulaiman M, Wilson S, Daoud F, Tuffaha M, AlMazroa M. A,et al. Breast cancer screening in Saudi Arabia: free but almost no takers. PloS one, 2015; 10: e0119051-e.
CrossRef - Polyak K. Heterogeneity in breast cancer. The Journal of clinical investigation, 2011; 121: 3786-3788.
CrossRef - Dandash KF, Al-Mohaimeed A. Knowledge, attitudes, and practices surrounding breast cancer and screening in female teachers of buraidah, saudi arabia. Int J Health Sci (Qassim), 2007; 1: 61-71.
- AlTamimi D. M, Shawarby M. A, Ahmed A, Hassan A. K, AlOdaini A. A. Protein expression profile and prevalence pattern of the molecular classes of breast cancer–a Saudi population based study. BMC Cancer, 2010; 10: 223.
CrossRef - Koo M. M, von Wagner C, Abel G. A, McPhail S, Rubin G. P, Lyratzopoulos G. Typical and atypical presenting symptoms of breast cancer and their associations with diagnostic intervals: Evidence from a national audit of cancer diagnosis. Cancer Epidemiol, 2017; 48: 140-146.
CrossRef - McAlpine J. N, ElHallani S, Lam S. F, Kalloger S. E, Luk M, Huntsman D. G,et al. Autofluorescence imaging can identify preinvasive or clinically occult lesions in fallopian tube epithelium: a promising step towards screening and early detection. Gynecol Oncol, 2011; 120: 385-392.
CrossRef - Pinker K. Advanced imaging for precision medicine in breast cancer: from morphology to function. Breast Care (Basel), 2017; 12: 208-210.
CrossRef - Eccles S. A, Aboagye E. O, Ali S, Anderson A. S, Armes J, Berditchevski F, et al. Critical research gaps and translational priorities for the successful prevention and treatment of breast cancer. Breast Cancer Res 2013; 15: R92.
CrossRef - Radhakrishna S, Agarwal S, Parikh P. M, Kaur K, Panwar S, Sharma S, et al. Role of magnetic resonance imaging in breast cancer management. South Asian J Cancer, 2018; 7: 69-71.
CrossRef - Selvi V, Nori J, Meattini I, Francolini G, Morelli N, DeBenedetto D, et al. Role of magnetic resonance imaging in the preoperative staging and work-up of patients affected by invasive lobular carcinoma or invasive ductolobular carcinoma. Biomed Res Int, 2018; 2018:
CrossRef - Macura K. J, Ouwerkerk R, Jacobs M. A, Bluemke D. A. Patterns of enhancement on breast MR images: interpretation and imaging pitfalls. Radiographics, 2006; 26: 1719-1734.
CrossRef - Lo G. G, Ai V, Chan J. K, Li K. W, Cheung P. S, Wong T. T, et al. Diffusion-weighted magnetic resonance imaging of breast lesions: first experiences at 3 T. J Comput Assist Tomogr, 2009; 33: 63-69.
CrossRef - Salem D. S, Kamal R. M, Mansour S. M, Salah L. A, Wessam R. Breast imaging in the young: the role of magnetic resonance imaging in breast cancer screening, diagnosis and follow-up. J Thorac Dis, 2013; 5 Suppl 1: S9-S
- Jiang X, Xie F, Liu L, Peng Y, Cai H, Li L. Discrimination of malignant and benign breast masses using automatic segmentation and features extracted from dynamic contrast-enhanced and diffusion-weighted MRI. Oncol Lett, 2018; 16: 1521-1528.
CrossRef - ElKhouli R. H, Macura K. J, Jacobs M. A, Khalil T. H, Kamel I. R, Dwyer A, et al. Dynamic contrast-enhanced MRI of the breast: quantitative method for kinetic curve type assessment. AJR Am J Roentgenol, 2009; 193: W295-300.
CrossRef - Maric J, Boban J, Ivkovic-Kapicl T, Djilas D, Vucaj-Cirilovic V, Bogdanovic-Stojanovic D. Differentiation of breast lesions and distinguishing their histological subtypes using diffusion-weighted imaging and ADC values. Front Oncol, 2020; 10: 332.
CrossRef - Grimm L. J, Zhang J, Baker J. A, Soo M. S, Johnson K. S, Mazurowski M. A. Relationships between MRI breast imaging-reporting and data system (BI-RADS) lexicon descriptors and breast cancer molecular subtypes: internal enhancement is associated with luminal B subtype. Breast J, 2017; 23: 579-582.
CrossRef - Kim M. J, Kim D, Jung W, Koo J. S. Histological analysis of benign breast imaging reporting and data system categories 4c and 5 breast lesions in imaging study. Yonsei Med J, 2012; 53: 1203-1210.
CrossRef - Baltzer P. A, Benndorf M, Dietzel M, Gajda M, Runnebaum I. B, Kaiser W. A. False-positive findings at contrast-enhanced breast MRI: a BI-RADS descriptor study. AJR Am J Roentgenol 2010; 194: 1658-1663.
CrossRef - Erguvan-Dogan B, Whitman G. J, Kushwaha A. C, Phelps M. J, Dempsey P. J. BI-RADS-MRI: a primer. AJR Am J Roentgenol, 2006; 187: W152-160.
CrossRef - Yoon J, Kim E. K, Kim M. J, Moon H. J, Yoon J. H, Park V. Y.Preoperative magnetic resonance imaging features associated with positive resection margins in patients with invasive lobular carcinoma. Korean J Radiol, 2020; 21: 946-954.
CrossRef - Dong H, Kang L, Cheng S, Zhang R. Diagnostic performance of dynamic contrast-enhanced magnetic resonance imaging for breast cancer detection: An update meta-analysis. Thorac Cancer, 2021; 12: 3201-3207.
CrossRef - Castro S. M, Tseytlin E, Medvedeva O, Mitchell K, Visweswaran S, Bekhuis T,et al. Automated annotation and classification of BI-RADS assessment from radiology reports. J Biomed Inform, 2017; 69: 177-187.
CrossRef - Ghaemian N, Haji Ghazi. Tehrani. N, Nabahati M. Accuracy of mammography and ultrasonography and their BI-RADS in detection of breast malignancy. Caspian J Intern Med, 2021; 12: 573-579.
- Li Y, Yang Z. L, Lv W. Z, Qin Y. J, Tang C. L, Yan X, et al. Non-mass enhancements on DCE-MRI: development and validation of a radiomics-based signature for breast cancer diagnoses. Front Oncol, 2021; 11: 738330.
CrossRef - Kim E. K, Ko K. H, Oh K. K, Kwak J. Y, You J. K, Kim M. J, et al. Clinical application of the BI-RADS final assessment to breast sonography in conjunction with mammography. AJR Am J Roentgenol, 2008; 190: 1209-1215.
CrossRef - Strigel R. M, Burnside E. S, Elezaby M, Fowler A. M, Kelcz F, Salkowski L. R, et al. Utility of BI-RADS assessment category 4 subdivisions for screening breast MRI. AJR Am J Roentgenol, 2017; 208: 1392-1399.
CrossRef - Gity M, Arabkheradmand A, Taheri E, Shakiba M. Diagnostic investigation of breast magnetic resonance imaging in malignant and benign mass lesions. Arch Med Sci, 2018; 14: 1061-1069.
CrossRef - Mahoney M. C, Gatsonis C, Hanna L, DeMartini W. B, Lehman C. Positive predictive value of BI-RADS MR imaging. Radiology, 2012; 264: 51-58.
CrossRef








