Mohamed G. Fathallah1 , Fatina I. Fadel1
, Fatina I. Fadel1 , Gamal Eldin Saadi3
, Gamal Eldin Saadi3 , Mohamed A. Abdel Mawla2
, Mohamed A. Abdel Mawla2  and Doaa M. Salah1
and Doaa M. Salah1
1Department of Pediatrics, Cairo University, Cairo, Egypt
2Departmentof Pediatrics, National Research Center, Giza, Egypt
3Department of Internal Medicine, Cairo University, Cairo, Egypt
Corresponding Author E-mail: mohammad.gamal@hotmail.com
DOI : https://dx.doi.org/10.13005/bpj/2242
Abstract
Objectives To assess the health related quality of life of living related donors after kidney transplantation and to evaluate clinical ,social and psychological condition post donation Study design This is an observational cross sectional study that included fifty living related donors of kidney transplant. All donors were assessed after at least one year of kidney donation. Data of the study was collected between April, 2019 and March, 2020. Methods The study included 50 living related donors;All donors were assessed after at least one year of kidney donation.WHOQOL-bref questionnaire (world health organization quality of life ) was used to assess quality of life of donors. Results The mean age at time of transplantation was 35.4±7.89 years. Eight cases developed hypertension after transplantation. There was no significant difference between serum creatinine before and after transplantation while there was significant decrease in glomerular filtration rate post transplantation. There was significant increase in fasting blood glucose and cholesterol in female donors compared to males.The results of the WHOQOL-bref questionnaire showed significant difference in results of psychological, social and environmental domains pre and post donation. Conclusion Proper selection of donors is very important to avoid complications post transplantation. Follow-up of donors should be maintained after donation.
Keywords
Donor; follow up Transplantation
Download this article as:| Copy the following to cite this article: Fathallah M. G, Fadel F. I, Saadi G. E, Mawla M. A. A, Salah D. M. Renal Outcome and Health Related Quality of Life of Living Related Donors In Pediatric Kidney Transplantation. Biomed Pharmacol J 2021;14(3). |
| Copy the following to cite this URL: Fathallah M. G, Fadel F. I, Saadi G. E, Mawla M. A. A, Salah D. M. Renal Outcome and Health Related Quality of Life of Living Related Donors In Pediatric Kidney Transplantation. Biomed Pharmacol J 2021;14(3). Available from: https://bit.ly/3D46MLY |
Introduction
Renal transplantation provides a better prognosis and long-term benefit to chronic kidney diseases patients 1.Kidney transplantation using grafts from living donors has increased along with the need for renal transplantation. Living-donor transplants provide more satisfyinggraft function and survival compared with deceased-donors2. Many studies have been done to check the risks. The results have showed that risks and benefits are presentin living donation. Kidney donation doesn’t cause physical benefit for the donor, but psychologic benefit are present (a sense of gratification). It isimportant to clarify the risks to make informed andadequate decisions 3,4.The inclusion criteria of the living donation have been extended and older donors and donors with minor problems such as hypertension have been accepted for donation 5. However, it must be noted that live donor nephrectomy is performed on healthypeople who do not need any intervention. So, donor safety andclose follow up remains important point in living kidney donation. It has been found that kidney function might be impaired immediately after donation and recovers within the first year. Previous studies suggest that renal function reached at 1 year postdonation remains stable at least for over the next decade but then impaired with ageing 6.
Previous studies showed that survival and quality of life (Qol) in living kidney donors are nearly similar to the general population 7. However according to recent studies kidney donors suffered from proteinuria, hypertension,and ESRD 8.9
An excellent method for QOL assessment in living donor transplantations has not been agreed upon. There are new studies discussing living donor transplant in different countries, most of them using the Medical OutcomesStudy Questionnaire 36-Item Short-formHealth Survey (SF-36) or, the WHOQOL-bref Questionnaire (World Health Organization Quality of Life-brief) 10, 11
The WHOQOL-brefincludes 26 items; the first two questions evaluate overall quality of life health satisfaction. The other 24 questions represent each of the 24 facets of which the original instrument is composed (WHOQOL-100), divided into four domains: physical, psychological, social relationships and environment. The mean score in each domain measures donor satisfaction with each aspect of their life, relating it with quality of life. The higher the score, the better this is perceived to be 12
Method
This is an observational cross sectional study that included fifty living related donors of kidney transplant for pediatric recipients. Included donors were randomly recruited during follow up of their related pediatric transplant recipients in Kidney Transplantation Outpatient Clinic, Cairo University Children Hospital. All donors were assessed after at least one year of kidney donation. Data of the study was collected between April, 2019 and March, 2020.
The study was ethically reviewed and approved by Pediatric Nephrology Unit, Department of Pediatrics, Faculty of Medicine, Cairo University and medical research ethical committee in the National Research Center. All procedures followed were in accordance with the Helsinki Declaration of 1964.
For all donors, kidney transplantation (KT) operation was performed in Cairo University Children Hospital, in which only living related donor transplants (LRDT) are allowed. Donors were followed up for at least 3 months post-transplant medically and surgically in our unit, then were referred for long-term follow-up in adult Nephrology department, Kasr Al Ainy Hospital.
Pre-transplantation medical data (as diabetes and hypertension), intraoperative details (as time of the operation, side of donor nephrectomy, number of renal transplant vessels) and early post-operative complications (as pneumothorax or chest/wound infection) were obtained by reviewingthe medical records. Late complications (as wound incisional hernia) were also reported.
Donor clinical and laboratory assessment was performed during their recruitment in the study. Blood pressure, fasting blood glucose, serum albumin, uric acid, cholesterol and triglycerides were measured. Kidney function was assessed by serum creatinine and quantitative urine protein assessment. GFR was calculated by modified Schwartz formula. Health Related Quality of Life (HRQOL) was evaluated for all donors using WHOQOL-bref questionnaire pre and post donation.
Statistical Package for Social Sciences version 15 (SPSS, Chicago, Ill) was used to analyze collected data. Nominal data were expressed as frequencies and percentage, parametric data as means and standard deviations (SD) and non-parametric data as median and range or interquartile range (IQR). Associations between the outcome measures and different components were tested for significance by using Chi-square test for categorical variables and the paired student t- test for continuous variables with normally distributed data. P value less than 0.05 was considered statistically significant.
Results
As seen in table 1 The study included Fifty living donors 24 males and 26 females. The mean age at time of transplantation was 35.4±7.89 years. The mean follow up duration post transplantation was 4.9±2.78 years.Rt donor nephrectomy was done in 31 donor while Lt was in 19.Single renal Artery was in 40 cases while double renal artery was found in 9 cases and triple renal artery was found in one donor .The mean systolic blood pressure was 139 and diastolic blood pressure was 77. Five donors were already hypertensive and controlled on Ca channel blockers and remained controlled post transplantation, while 8 cases developed hypertension after transplantation and received treatment . Only one case developed Diabetes mellitus and started treatment.
Table 1: Demographic and clinical data of donors (n= 50)
| Gender (Male/Female) | 24/26 |
| Weight (kg) | 91± 33.874 |
| Duration post-transplantation in years | 4.9±2.78 |
| Mean age at time of transplantation in years | 35.4±7.89 |
| Nephrectomy (Rt/Lt) | 31/19 |
| Smoker | 21 |
| Systolic BP (mm hg) | 139±18.88 |
| Diastolic BP (mm hg) | 77.12±12.15 |
| Fasting blood glucose (mg/dl) | 101±19.8 |
| Serum Cholesterol (mg/dl) | 213±98.8 |
| Serum Albumin (mg/dl) | 4.1±1.1 |
| Mean Hb (g/dl) | 12.8±1.2 |
| Mean Protein in urine | 41.58±12.25 |
| Serum Uric acid (mg/dl) | 5.9± 2.214 |
| Serum Calcium (mg/dl) | 9.5±2.21 |
| Serum Triglycerides (mg/dl) | 115±62.5 |
Four cases developed incisional hernia post transplantation and were treated conservatively.The mean protiens in urine was 41.58 mg ptn/gm creatnine .Three donors developed microalbuminuria due to development of diabetes and hypertension.
There was no significant difference between serum creatinine before and after transplantation (p value 0.1161), while there was significant decrease in glomerular filtration rate post transplantation as seen in figure 1 (p value 0.0001).While comparing results of males and female donors There was significant increase in fasting blood glucose(FBG) and cholesterol in female donors compared to males (Pvalue 0.023, 0.0019) . While there was significant increase in serum uric acid in male donors as seen in table 2.
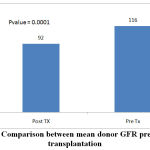 |
Figure 1: Comparison between mean donor GFR pre and post transplantation |
Table 2: Comparison between males and females donors
| M (24) | F (26) | P value | |
| FBG (mg/dl) | 89 ±41.25 | 122 ±54.45 | 0.023 |
| Serum Cholesterol(mg/dl) | 189±85.12 | 288±122.87 | 0.0019 |
| Serum uric acid (mg/dl) | 5.9±1.9 | 4.1±1.5 | 0.0005 |
| Hb (g/dl) | 13.9±7.9 | 11.8±7.5 | 0.3398 |
| Protiens in urine | 56.5±27.9 | 45.125±17.5 | 0.0880 |
| Serum Albumin (mg/dl) | 4.5±1.5 | 4.3± 1.4 | 0.628 |
| Serum Triglycerides (mg/dl) | 142±45 | 160±52 | 0.1985 |
The WHOQOL-bref questionnaire were used and the donors were subjected to the questionnaire before and after the transplantation.
The results of the WHOQOL-bref questionnaire was shown in table 3 and figure 2 . There was significant difference in results of psychological, social and environmental domains of WHOQOL-bref questionnaire.
Table 3: Results of different domains of WHOQOL-bref questionnaire.
| Qol Items | Mean | median |
| Physical domain (before donation) | 27.6±5.334 | 28.5 |
| Physical domain (after donation) | 27.94±6.179 | 30 |
| Psychological domain (before donation) | 18.84±2.985 | 18 |
| Psychological domain (After donation) | 28.7±2.323 | 29 |
| social domain (before donation) | 10.12±1.649 | 10 |
| social domain (after donation) | 14.1±1.669 | 14 |
| Environmental domain (before donation) | 32.48±1.432 | 32 |
| Environmental domain(After donation) | 33.64±1.758 | 36 |
| Overall Qol before Donation | 2.26±0.6642 | 2 |
| Overall Qol after Donation | 4.9±0.4629 | 5 |
| Overall general health before donation | 2.42±0.702 | 2 |
| Overall general health after donation | 4.72±0.5729 | 5 |
 |
Figure 2: Comparison of the quality of life of the living kidney donors before and after transplantation by WHOQOL-bref questionnaires |
Discussion
Donor safety and close follow up remains important point in living kidney donation after transplantation. The study was conducted on 50 living donors with nearly same percentage of males and females . These results were nearly similar to Chatzikyrkou results which showed that male percentage of donors was 35%. 13 .The male percentage was higher in Dienemann et al study on donor hypertension which was 69%.14. The mean age at time of transplantation was 35.4±7.89. The age was younger than age of donors in many studies like Jankietal where the mean age of donors was 53 years 15.
The mean systolic blood pressure was 139 and diastolic blood pressure was 77. While 8 cases developed hypertension after transplantation. These results were higher than study done by Kasiske et al and studing 3 years follow up of donors where mean systolic and diastolic blood pressure were 120.7,74.5 respectively 16.while discussing long term consequences of live kidney donation Gossmann et al found that systolic and diastolic blood pressure were 134 and 81 respectively which was quite similar to our study ,they also noticed increase in the percentage of donors developed hypertension from 7 to 30 % 17.
There was significant decrease in glomerular filtration rate post transplantation ,similar to Gossmann et al where GFR decreased from 119 ± 30 to 99 ± 30 mL/min/1.73 m2 17. These results were also similar to Park et al who were trying to find tools to Predict Chronic Kidney Disease Risk in Living Kidney Donors post transplantation and found decline in GFR <60 mL/min/1.73 m2 1 year post transplantation .This was correlated with old age , hypertension , serum uric acid, and creatinine levels, and lower serum calcium levels.
The results of the multivariate analysis found that olderpatients and those with higher serum creatinine levels andlower serum calcium levels had a significantly greater risk ofdeveloping CKD 18.Chatzikyrkou et al also reported decline in GFR after 1 year donation when compared to that pre donation and found that decline in GFR was correlated with older age 13.
Our results were also similar to janki et al in 5 years follow up of donors where they find that half of donors developed low GFR < 60 ml/min/
1.73 m2. and found that decline may be due to older age at time of donation or having a lower eGFR before transplantation 19.
The WHOQOL-bref questionnaire was used and the donors were subjected to the questionnaire before and after the transplantation.
The results showed no significant changes in the physical domain while there were significant changes and improvement in the social, psychological and environmental domains and in the overall QOL and general health before and after donation. These results were due to the type of donors in our study who are related either mother, father, brother or uncle. These donors were ready to donate and even to loss their lives to keep their children transplanted and stop suffering of their kids that make the donation an altruistic behavior and made them satisfied. Our results was similar to Padra˜o and Sens results which discussed Quality of life of kidneydonors in Brazil by using short form-36 questionnaires and WHO QOL brief questionnaire comparing donors with control group –unlike our study- and found no significant changes regarding physical domain but showed significant increase in remaining domains when compared to control group 20. Our results were also similar to Vemuru Reddy SK et al Where donors showed significant improvement in the QOL in the physical, Psychological and environmental domain before and after organ donationand non-significant improvement in the social relationship 21.
On contrast Lumsdaine et alassessed the donor QOL before, six weeks and one year after donation, and found declined QOL six weeks after the donation , but results improved one year after donation . These results may be due to the early time of assessment after donation. 22.Erim et al also found significant decline in quality of life 3 months post transplantation while assessing quality of life in more than 150 living kidney donors before and after donation and assuming that cause may be due to the early time point of assessment 23.Nejatisafa et al reported low QOL after donation while discussing QOL in unrelated donors post donation and found the reason that most of kidney donors in Iran are unrelated whose main motivation is “a financial gain” 22.
Conclusion
This study has concluded that related living kidney donation does not negatively affect the lives ofdonors and may improves many social, psychological and environmental aspects of their lives. Careful donor selection is very important point to provide good physical quality of life post donation. The majority ofliving related donors would donate again and again to protect their children.
Acknowledgment
To all our heroes who donated for their children to have better life not afraid of having health problems post donation, just scarifying their life for their children .
Conflict of intersest
The authors declare no conflicts of interest
References
- de Fijter JW, Meinders A. [Long live the kidney donor] Lang leve de nierdonor. Ned TijdschrGeneeskd 2014; 158: A8180.
- Cecka JM. The UNOS Scientific Renal Transplant Clin Transplant 2000:1e18.
- Abecassis M, Adams M, Adams P, et al. Consensus statement on the live organ donor. JAMA 2000;284:2919.
CrossRef - Steiner R, Matas AJ. First things first: laying the ethical and factual groundwork for living kidney donor selection standards. Am J Transplant 2008;8:930.
CrossRef - Ahmadi AR, Lafranca JA, Claessens LA, et al. Shifting paradigms in eligibility criteria for live kidney donation: a systematic review. Kidney Int 2014; 87: 31.
CrossRef - von Zur-Muhlen B, Berglund D, Yamamoto S, Wadstrom J. Single-centre long-term follow-up of live kidney donors demonstrates preserved kidney function but the necessity of a structured lifelong follow-up. Ups J Med Sci 2014; 119: 236.
CrossRef - Ibrahim HN, Foley R, Tan L, et al. Long-term consequences of kidney donation. N Engl J Med 2009;360:459e69.
CrossRef - Mjoen G, Hallan S, Hartmann A, et al. Long-term risks for kidney donors. Kidney Int 2014;86:162e7.
- Muzaale AD, Massie AB, Wang MC, et al. Risk of end-stage renal disease following live kidney donation. JAMA 2014;311: 579e86.
CrossRef - Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 1992: 30: 473.
CrossRef - The WHOQOL Group. Development of the World Health Organization WHOQOL-brief quality of life assessment. Psychol Med 1998: 28: 551.
CrossRef - Fleck MPA, Leal OF, Louzada S, Xavier M, Chachamovich E, Vieira G, et al. Desenvolvimento da versãoemportuguês do instrumento de avaliação de qualidade de vida da OMS (WHOQOL-100) Rev Bras Psiquiatr. 1999;21(1):19–28. doi: 10.1590/S1516-44461999000100006. [CrossRef] [Google Scholar] CrossRef
- Chatzikyrkou C, Scurt FG, Clajus C, Roumeliotis S, Mertens PR, Haller H, Blume C, Liakopoulos V: Predictors of Outcomes of Living Kidney Donation: Impact of Sex, Age and Preexistent Hypertension. Transplant Proc. 2019 Mar;51(2):396-404. doi: 10.1016/j.transproceed.2019.01.015. Epub 2019 Jan 4.
CrossRef - Dienemann T, Schellenberg J, HellerK, et al. Association of donor hypertension and recipientrenal function in living donor kidney transplantation: Asingle‐center retrospective study. Clin Transplant.2019;33:e13697.
CrossRef - Shiromani Janki, Leonienke F. C. Dols, ReinierTimman, Evalyn E. A. P. Mulder, Ine M. et al: Five-year follow-up after live donor nephrectomy –cross-sectional and longitudinal analysis of aprospective cohort within the era of extendeddonor eligibility criteriaTransplant International 2017; 30: 266–276
CrossRef - Bertram L. Kasiske, Teresa Anderson-Haag, Ajay K. Israni, Roberto S. Kalil, Paul L. Kimmel ,et al: A Prospective Controlled Study of Living Kidney Donors: Three-Year Follow-up Am J Kidney Dis. 2015 Jul; 66(1): 114–124.
CrossRef - Jan Gossmanna,b,, Albina Wilhelmb, Heinz-Georg Kachela, JochenJordanc, UliSannc, Helmut Geigerb, Wolfgang Kramerd and Ernst-Heinrich Scheuermannb Center Long-Term Consequences of Live Kidney Donation Follow-Up in 93% of Living Kidney Donors in a Single Transplant American Journal of Transplantation 2005; 5: 2417–2424
CrossRef - S. Park, H.K. Ahn, J. Na, H.H. Lee, Y.E. Yoon, M.G. Yoon, and W.K. Han Development of a Screening Tool to Predict Chronic Kidney Disease Risk in Post-nephrectomy Living Kidney Donors Transplantation Proceedings, 50, 993e997 (2018)
CrossRef - Padra˜o MB, Sens YAS. Quality of life of living kidney donors in Brazil: anevaluation by the short form-36 and the WHOQOL-bref questionnaires.Clin Transplant 2009: 23: 621–627.
CrossRef - Lumsdaine JA, Wray A, Power MJ et al. Higher quality of life in living donor kidney transplantation: prospectivecohort study. Transplant Int 2005: 18: 975.
CrossRef - Erim, Y., Kahraman, Y., Vitinius, F. et al. Resilience and quality of life in 161 living kidney donors before nephrectomy and in the aftermath of donation: a naturalistic single center study. BMC Nephrol 16, 164 (2015).
CrossRef - Nejatisafa AA, Mortaz-Hedjri S, Malakoutian T, Arbabi M, Hakemi MS et al : Quality of Life and Life Events of Living Unrelated Kidney Donors in Iran: A Multicenter StudyTransplantation. 2008 Oct 15;86(7):937-40. doi: 10.1097/TP.0b013e318186d945.
CrossRef - Sunil K. Vemuru Reddy, Sandeep Guleria, OkidiOkechukwu, Rajesh Sagar, DipankarBhowmik, Sandeep Mahajan: Live related donors in India: Their quality of life using world health organization quality of life brief questionnaireIndian J Urol. 2011 Jan-Mar; 27(1): 25–29.
CrossRef







