Enas Abdel Hamid1 , Walaa Ali1
, Walaa Ali1 , Hanaa Ahmed2
, Hanaa Ahmed2 , Amre Megawer3
, Amre Megawer3 and Wafaa Osman4
and Wafaa Osman4
1Department of Child health, Child Health, National Research Centre, Giza, Egypt
2Department of Hormones, Professor of biochemistry, National Research Centre, Dokki, Giza, Egypt.
3Department of pediatrics , Pediatric, Institute of ophthalmology, Giza, Egypt.
4Department of Pediatrics, Pediatric, Faculyt of Medicine, Ain Shams University, Abassia, Cairo, Egypt.
Corresponding Author E-mail: wafaaosman83@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2232
Abstract
Community acquired pneumonia (CAP) is a major contributing cause for the increased rate of childhood mortalities and morbidities in the developing countries. Thus, we aimed in this study to appraise the significance of acute phase reactant proteins in correlation with the modified pneumonia prognostic score to assess the disease severity and outcome in children.This study included 40 children with pneumonia ( age between 6 months 2 years ) and other 40 healthy controls ( age and sex matched). They were enrolled in the study and a detailedhistory’s obtained, full clinical examination and assessment of AGP, CRP and ferritin in serum in addition to CBC.AGP, CRP and ferritin showed significant higher levels in children with pneumonia than healthy controls. Also, their values were significantly higher in nonsuvivors than survivors.The present investigation provides a distinct evidence for the prominence of acute phase reactants (ferritin, CRP and AGP) in comparison with the clinical scores in predicting early high risk prognosis of pneumonia in children.
Keywords
Acute phase reactant proteins; Clinical score; Children; Pneumonia; Prognosis
Download this article as:| Copy the following to cite this article: Hamid E. A, Ali W, Ahmed H, Megawer A, Osman W. Significance of Acute Phase Reactants as Prognostic Biomarkers for Pneumonia in Children. Biomed Pharmacol J 2021;14(3). |
| Copy the following to cite this URL: Hamid E. A, Ali W, Ahmed H, Megawer A, Osman W. Significance of Acute Phase Reactants as Prognostic Biomarkers for Pneumonia in Children. Biomed Pharmacol J 2021;14(3). Available from: https://bit.ly/38HnmEz |
Introduction
Respiratory tract infections include croup syndromes, bronchitis, bronchiolitis and pneumonia. Pneumonia is an infection that affects the air sacs in one or both lungs. It had been reported that, pneumonia is the single major cause for children mortality in the developing countries 1. In particular, the Community Acquired Pneumonia (CAP) is the major contributorfor the high annual mortalities and morbidities in childhood age2. Proper diagnosis and earlytreatment of CAP are vital for reduction of antibiotic resistance,long-term morbidities, life-threatening health problems and consequently the economical burden 3. In Egypt, children under 5 years represent nearly 13.4% of the total population. The incidence of pneumonia in Egypt has been established at 0.11–0.20 pneumonia episodes per year 4.
Clinical signs such as intercostal retraction, desaturation, younger age, immune compromise and low socioeconomic circumstancesinvolving, malnutrition, young mothers low education level and the presence of household air pollutantsare considered as risk factors for increased mortality among children diagnosed with CAP 5. On the other side, adequate antenatal care and regular immunizations have reduced the risk of mortality. A presumptive clinical diagnosis of pneumonia is usually done when new radiological infiltrates develop in patients with fever, leukocytosis, tracheal secretions as well as the separation of microorganisms from patients airways 6. Whatever, the microbiologic diagnostic procedure chosen, extra laboratory processing and delaying of about 48-72 hours are required for accurate quantitative microbial culture results. In parallel, physicians often feel uncomfortable about the diagnosis and may give unwanted antibiotics during waiting for laboratory data.
In the past, predictors of treatment failure includedvery young age, high respiratory rate in correlation for age in addition tosevere chest retractions and they could predict increased liability to death. So, there was an urgent need for implementing clinical diagnostic and prognostic tools commonly named as risk scores, severity of disease indices, or high mortality predictive scores that can utilize these risk factors for further segregation of high-risk category for implementing adequate management in order to inhibit adverse outcomes. No universal predictive tools have been broadly adopted for application in children with pneumonia, especially in low resources countries 7. Clinicians have endorsed several scoring systems for predicting pneumonia outcome and serving as guidelines for admission to intensive care units, like pneumonia severity index (PSI) 8and predisposition, insult, response, and organ dysfunction score (PIRO) 9. Because there is no prognostic score without limitations, there has been an urgencyfor incorporating these scores in combination of diagnostic and prognostic biomarkers as they are less liable for bias and could provide a reliable diagnostic and predictor tools for disease severity and outcome 10. Therefore, various biological markers have been investigated in order to improve pneumonia management 11.
Inflammation has been shown to be associated with the alteration in the micronutrient-relevant markers such as ferritin, and retinol 12. This inflammatory condition also leads to changes in blood concentration of acute phase proteins (APP) like c-reactive protein (CRP) and α1-acid glycoprotein (AGP) which occurs concurrently with the variation in the micronutrient levels 13.
AGP is one of lipocalin family which is also called orosomucoid. It is mainly a plasma protein with different physiological, metabolic regulatingand immune modulating actions via binding and transport of basic compounds, including drugs14.
CRP is a major APPs that increases in bacterial pneumonia although, it can be also increased slightly in severe viral acute respiratory syndromes 15. The concentrations of CRP increase rapidly in acute insult, reaches peak level with in 48 hours and decreases again within a week with a mean half life around 19 hours 13 , 16.
Recently, The World Health organization (WHO) recommends the assessment of the levels of both AGP and CRP in addition to micronutrient biomarkers as iron and vitamin A in large scale periodic population surveys and various researches 17.
Consequently, the current study was intended to appraise the significant share of acute phase reactant proteins in correlation with the modified pneumonia prognostic score to assess the disease severity and outcome in the children.
Subjects and Methods
This case control study was conducted in the Pediatric Department, Ain Shams University Hospital during period from November, 2020 to January, 2021.
Subjects
The study group included forty children having pneumonia (aged between 6 months and 2 years) who were diagnosed according to WHO criteria 18 “children with fever (≥ 38.5⁰C), paroxysmal dry cough, difficulty of respiration with at least one of the following signs : respiratory rate ≥ 50 breaths / minute in an infant of 2 – 11 months age, ≥ 40/ minute in age of 12 – 58 months, or a lower chest retraction ” in addition to radiological findings that indicate pneumonia (opacity, hyperinflation, exaggerated broncho vascular markings). Children with other systemic illness including congenital cardiac anomalies, chronic specific lung infection, protein energy malnutrition and those who had already had been treated withantimicrobials or corticosteroids were rolled out from the study.There were also forty apparently healthy children age and sex matched who were involved in the study as controls . This study was approved by Medical Research Ethical Committee of the National Research Centre, Egypt, with registration No 20 /179. A written informed consent for all participants was collected from their parents after clarifying the aim and methodology of the study.
Methods
All children in the study were enrolled and a detailed history was obtainedwith further local and general examination. chest x-ray and modified PIRO score were done for children with pneumonia only. Local chest examination included inspection for ( retractions, chest movement, localized bulge or localized retraction and signs of respiratory distress) and auscultation for ( breaths sounds and adventurous sounds). Modified PIRO score is a simple scoring system for predicting pneumonia outcome. It involved the following parameters: predisposition (age <6 months, comorbidity), insult (hypoxia [O2 saturation <90%], hypotension [according to age] and bacteremia), response (multilobar or complicated pneumonia) and organ dysfunction (kidney failure, liver failure and acute respiratory distress syndrome). Each criterion is given one point (range: 0–10 points). The predictive value of the modified PIRO score of death was assessed by dividingsick children into four risk levels: low (0–2 points), moderate (3–4 points), high (5–6 points) and very high risk (7–10 points) according to Araya et al.9. A venous blood samples (3ml) wereobtained from each child under complete aseptic conditions. An amount of (1.5 ml) was collected in EDTA containing tubes,freezed for 3 hours. The remaining half was collected in 2 tubes without EDTA and further centrifuged using cooling centrifugation for 10 min at 4 °C and thenthe serum samples were further stored at -20°C till the analysis time.
Blood samples were withdrawn to children with pneumonia on the first day of admission. The endpoint variable was death within 30 days of admission.
The laboratory investigations included
Complete blood count including hemoglobin, RBC, WBC, platelets counts was determined by using an automated analyzer (Cel-dyn.3500; Abbott Diagnostics, Abbott park; IL).
Serum iron level was measured using the colorimetric ferrozine method without deprotinization by using iron assay kit obtained from Japan Institute for the Control of Aging (JaICA) Nikken SEIL Co., Ltd. Japan according to protocol ofmanufacturer and serum iron stores (ferritin) was estimated by Immunoradiometric assay according to the method of Addison et al. 19. Serum α-1AGP was assessed by using enzyme linked immunosorbent assay (ELISA) kit purchased from Sunlong Biotech Co., LTD, China according to manufacturer manual.
Semi quantitative CRP was analyzed by latex agglutination. (Omega Diagnositic, Ltd, Alva, UK) following the manufacturer’s instructions.
Statistical analysis
The obtained data were manipulated and tabulated by using SPSS software program version 20.0. Data were further analyzed in the form of mean and standard deviation regarding the quantitative data as mean family and room number, crowding index and age in sociodemographic data, weight and laboratory results, while qualitative data as sex, residence, type of feeding within first year, mother education, birth order, family and room numbers in sociodemographic data and scores of risk and treatment among cases were presented by number and percent. Comparisons between cases and controls, also between level of risk among cases were done. Comparison between the quantitative data using t test or ANOVA and Post Hoc tests with calculation of p value to determine the statistically significant difference between groups. Chi-square was used to determine if the association between two qualitative variables is statistically significant. Correlations of clinical data and inflammatory markers among cases and correlation coefficient and p value were computed. A value of p<0.05 is considered statistically significant and a value of p<0.01is considered statistically highly significant. ROC curve and area under curve were done between cases and controls also, survivors and nonsuvivors regarding serum ferritin, CRP and AGP. Accordingly coordinates of the curve were done to calculate the cut off values with specificity and sensitivity
Results
A total number of 80 children were involved in the current study, then were subdivided into two equal groups: case group( children with pneumonia) and control group ( healthy children). The characteristics of the all studied children and their mothers are depicted in Table (1)
There was no significant difference between cases and controls as regards sex and age. The cases were 62.5% males and 37.5% females and the controls were 42.5% females and 57.5% males (p=0.648). The mean age of the two studied groups were 13.85±3.4 months and 15.83±4.4 months respectively (p=0.095) so both groups were sex and age matched .A highly significant difference between both studied groups regarding the residence; as most of the cases were from rural areas (65%), while most of the control group were from the urban areas (80%), (p<0.001). A statisticallysignificant difference was demonstrated between the case and control groups regarding the type of feeding within the first year of life; where the artificial feeding was more in the cases (52.5%) than the control patients (32.5%), (p=0.023). It was observed that 55% of the control group received breast feeding, while 25% of cases received breast feeding .The mothers of the case group had significantly lower level of education than the control group (p=0.009). There was a significant statistical difference between cases and controls as regards family number, crowding index, birth order and weight (p<0.001).
Table 1: Comparison between the case and control studied groups regarding sociodemographic characteristics.
| Variable | Cases
[N=40 (%)] |
Controls
[N=40 (%)] |
p value | |
| Sex | ● Male | 25 (62.5) | 23 (57.5) | 0.648 |
| ● Female | 15 (37.5) | 17 (42.5) | ||
| Residence | ● Rural | 26 (65.0) | 8 (20.0) | <0.001** |
| ● Urban | 14 (35.0) | 32 (80.0) | ||
| Feeding within first year | ● Breast feeding | 10 (25.0) | 22 (55.0) | 0.023* |
| ● Artificial | 21 (52.5) | 13 (32.5) | ||
| ● Both | 9 (22.5) | 5 (12.5) | ||
| Mother education | ● Illiterate or Read &Write | 9 (22.5) | 0 | 0.003** |
| ● Secondary | 16 (40.0) | 15 (37.5) | ||
| ● University | 15 (37.50) | 25 (62.5) | ||
| Birth order | ● First | 4 (10.0) | 23 (57.5) | <0.001** |
| ● Second | 18 (45.0) | 17 (42.5) | ||
| ● Third or more | 18(45.0) | 0 | ||
| (mean±SD) | 2.43±0.8 | 1.43±0.5 | <0.001** | |
| Family number | ● 3 | 0 | 21 (32.5) | <0.001** |
| ● 4 | 12 (30.0) | 11 (27.5) | ||
| ● 5 | 21 (52.5) | 8 (20.0) | ||
| ● 6 or more | 7 (17.5) | 0 | ||
| (mean±SD) | 4.93±0.8 | 3.68±0.8 | <0.001** | |
| Room number | ● 2 | 35 (87.5) | 20 (50.0) | <0.001** |
| ● 3 | 5 (12.5) | 20 (50.0) | ||
| (mean±SD) | 2.13±0.3 | 2.5±0.5 | <0.001** | |
| Crowding index | (mean±SD) | 2.08±0.3 | 1.47±0.3 | <0.001** |
| Age (months) | (mean±SD) | 13.85±3.4 | 15.83±4.4 | 0.095 |
| Weight (Kg) | (mean±SD) | 10.63±1.6 | 12.08±1.8 | <0.001** |
**p < 0.01 highly significant. *p< 0.05 significant
The results in Table (2) represented the levels of AGP, CRP and ferritin which displayed significant elevation in cases versus healthy controls (p< 0.001). Also, TLC had statistically significant higher value in cases than the healthycontrols (p=0.024) . On the contrary, platelets, iron and Hb% had a statistically higher values in healthy controls than in cases (p<0.001).
Table 2: Comparison between the case and control studied groups regarding the laboratory investigations.
| Variable | Cases
(N=40) mean±SD |
Controls
(N=40) mean±SD |
p value |
| Hemoglobin (g /dl) | 11.64±0.8 | 12.85±1.3 | <0.001** |
| Serum iron ( ug/d) | 82.48±33.3 | 114.57±2.5 | <0.001** |
| Serum ferritin (ng/ ml) | 159.85±102.7 | 64.73±35.6 | <0.001** |
| TLC | 10.59±3.0 | 9.44±0.8 | 0.024* |
| Platelets | 191.58±53.1 | 264.88±72.3 | <0.001** |
| CRP (mg/ dl) | 14.78±11.2 | 3.15±1.3 | <0.001** |
| AGP (ng/ ml) | 14.2±9.2 | 7.6±3.0 | <0.001** |
* p < 0.05 significant **p < 0.01 highly significant
The modified PIRO scoremean value was 3.46±1.4 and the total deaths were 6 cases (15%).Among patients with modified PIRO score of 0 (n=0), 1 (n=0), 2 (n=11), 3 (n=12), no deaths were observed. Meanwhile, in children with score 4 (n=10) one death occured, 5 (n=2) one death occured, 6 (n=1) one death occured, 7(n=3) three deaths occurred with percentage of mortality 2.5%, 2.5%, 2.5% and 7.5% respectively).There were no cases having scores from 8 to ten within our study. The predictive value of the modified PIRO score of mortality was assessed by stratifying patients into four levels of risk: low (0–2 points), moderate (3–4 points), high (5–6 points) and very high risk (7–10 points). In our study, 11 (27.5%) and 22 (55%) of our studied patients were divided in low and moderate risk groups respectively while the high and very high risk categories were comprised by 3 patients each ( 7.5%). The mortality was one child ( 2.5%), two children ( 5%), three children (7.5%) within the moderate, high and very high risk categories respectively ( Table 3).
Table 3: Descriptive data of modified PIRO score points and risk categories among cases.
| Modified
PIRO score points (mean±SD) 3.64 ±1.4 |
Cases
N=40 No (%) |
Deaths
N= 6 (15%) No.(%) |
| zero
1 2 3 4 5 6 7 8 9 10 |
–
– 11 (27.5) 12 (30.0) 10 (25.0) 2 (5.0) 1 (2.5) 3 (7.5) – – – |
–
– – – 1(2.5) 1(2.5) 1(2.5) 3 (7.5) – – – |
| Risk categories | ||
| ● Low risk
● Moderate risk ● High risk ● Very high risk |
11 (27.5)
22 (55.0) 3 (7.5) 3 (7.5) |
–
1(2.5) 2(5) 3(7.5) |
Table (4) illustrated the results of ferritin, AGP ,CRP that revealed significant difference between the four risk groups with the highest level in very high risk group (p<0.001). Also, iron, Hb% and platelets were significantly different between the four risk groups but, with the highest level in low risk group (p =0.036, =0.002, <0.001 respectively). TLC showed insignificant difference between the four risk groups (p =0.19).
Table 4: Comparison between 4 risk categories regarding laboratory investigations
| Variable | Low risk
11 (%27.5) mean±SD |
Moderate risk
22 (55.0%) mean±SD |
High risk
3 (%7.5) mean±SD |
Very high risk
3 (7.5%) mean±SD |
p value |
| Hemoglobin (g/ dl) | 12.14±0.9 | 11.68±0.7 | 11.27±0.4 | 10.23±0.6 | 0.002** |
| Serum iron (ug/ dl) | 78.0±26.7 | 74.88±32.4 | 108.1±12.9 | 126.43±47.7 | 0.036* |
| Serum ferritin ng/ ml | 100.27±67.3 | 150.36±89.0 | 234.0±59.8 | 372.0±3.5 | <0.001** |
| TLC | 9.87±3.3 | 11.05±2.5 | 9.4±3.2 | 13.47±0.5 | 0.19 |
| Platelets | 247.45±50.5 | 179.73±34.7 | 140.67±11.0 | 128.33±30.1 | <0.001** |
| CRP ( mg/ dl) | 6.73±1.7 | 13.66±5.6 | 18.77±4.6 | 48.03±5.9 | <0.001** |
| AGP ( ng/ ml) | 7.18±1.2 | 13.18±5.7 | 21.33±3.1 | 39.0±0 | <0.001** |
**p <0.01 highly significant, *p< 0.05 significant
The results presented in table (5) displayed that six cases have died (15%) within 30 days of admission. The mean values of AGP, CRP, ferritin and modified PIRO score were significantly different between survivors and non survivors (higher values in non survivors) (p<0.001).While, Hb% and platelets had higher significant values in survivors than non survivors (p =0.008, 0.01 respectively).
Table 5: Comparison between survivors and non survivors regarding laboratory investigations and modified PIRO score.
| Variables | Non survivor patients N=6 (%15) mean±SD |
Survivor patients N=34(%85) mean±SD |
p value |
| Hemoglobin (g/ dl) | 10.82±0.8 | 11.78±0.8 | 0.008** |
| Serum iron (ug/ dl) | 103.18±54.3 | 78.83±27.9 | 0.328 |
| Serum ferritin (ng/ ml) | 303.33±83.9 | 134.53±83.7 | <0.001** |
| TLC | 10.78±4.0 | 10.56±2.9 | 0.869 |
| Platelets | 141.17±30.7 | 200.47±51.5 | 0.01* |
| CRP ( mg/dl) | 34.53±15.4 | 11.29±5.4 | <0.001** |
| AGP (ng / ml) | 31.17±8.6 | 11.21±5.2 | <0.001** |
| PIRO score | 6.0±1.3 | 3.0±0.9 | <0.001** |
** p < 0.01 highly significant *p < 0.05 significant
As regard to correlations, AGP showed significant positive correlation with CRP, ferritin, modified PIRO score (p<0.001). On the opposite hand, there was significant negative correlation with iron, Hb, platelets (p = 0.011 and< 0.001, < 0.001 respectively). CRP showed significant positive correlation with AGP, ferritin and modified PIRO score (p<0.001). Meanwhile, it showed significant negative correlation with iron, Hb and platelets (p=0.042, < 0.001, < 0.001 respectively). Ferritin showed significant positive correlation with AGP, CRP and modified PIRO score (p<0.001), whereas, there was significant negative correlation with platelets (p=0.004), as depicted in Table (6).
Table 6: Correlations of clinical data and laboratory investigations in cases group (n=40).
| Variable | Hb %
g/dl |
Serum iron | Serum ferritin | TLC | platelets | CRP | AGP | PIRO | Crowding index | |
| Serum iron ug / dl |
r | .187 | 1 | |||||||
| p | .249 | |||||||||
| Serum ferritin ng/ ml | r | -.260 | .092 | 1 | ||||||
| p | .106 | .570 | ||||||||
| TLC | r | -.123 | .041 | .080 | 1 | |||||
| p | .448 | .803 | .622 | |||||||
| Platelets | r | .466** | .249 | -.441** | -.194 | 1 | ||||
| p | .002 | .121 | .004 | .229 | ||||||
| CRP mg/d | r | -.587** | -.323* | .655** | .177 | -.558** | 1 | |||
| p | .000 | .042 | .000 | .274 | .000 | |||||
| AGP ng/ ml | r | -.600** | -.396* | .633** | .137 | -.594** | .954** | 1 | ||
| p | .000 | .011 | .000 | .398 | .000 | .000 | ||||
| PIRO score | r | -.586** | -.378* | .639** | .246 | -.631** | .839** | .859** | 1 | |
| p | .000 | .018 | .000 | .131 | .000 | .000 | .000 | |||
| Crowding index | r | .118 | -.082 | .022 | .120 | .083 | -.111 | -.127 | -.117 | 1 |
| P | .469 | .616 | .895 | .462 | .609 | .495 | .433 | .478 | ||
| Age | r | .115 | .227 | .128 | -.403** | .170 | .040 | .051 | .144 | -.160 |
| p | .479 | .158 | .432 | .010 | .294 | .807 | .753 | .383 | .325 | |
*. Correlation is significant at the 0.05 level (2-tailed),**. Correlation is significant at the 0.01 level (2-tailed).
ROC curve analysis for using AGP in detection of pneumonia clarifiedthat the area under the curve is 0.801 with cutoff level equal to 7.0 (P=0.000), with sensitivity 85% and specificity 65% .While, ROC curve for CRP in pneumonia detection proved that the area under the curve is 0.981 with cutoff level equal to 6.10 (P= 0.000) with sensitivity 92.5% and specificity 95%. ROC curve analysis of ferritin for pneumonia diagnosis proved that the area under the curve is 0.891 with cutoff level equal to 58.10 (P=0.000) with sensitivity 100% and specificity 72.5% (Fig. 1).
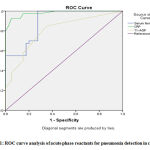 |
Figure 1: ROC curve analysis of acute phase reactants for pneumonia detection in children. |
| Test Result Variable(s) | AUC | SE | p | Asymptotic 95% CI | Positive if Greater Than or Equal Toa | Sensitivity% | Specificity % | |
| Lower Bound | Upper Bound | |||||||
| Serum ferritin | .891 | .035 | .000 | .822 | .960 | 58.10 | 100.0 | 72.5 |
| CRP | .981 | .012 | .000 | .957 | 1.000 | 6.10 | 92.5 | 95.0 |
| AGP | .801 | .050 | .000 | .703 | .898 | 7.0 | 85.0 | 65.0 |
ROC curve analysis of AGP for mortality prediction in children with pneumonia proved that the area under the curve is 0.980 with cutoff level equal to 20.50 (P=0.000) with sensitivity 100% and specificity 94.1%. ROC curve analysis of CRP for predicting mortality in pneumonia proved that the area under the curve is 0.973 with cutoff level equal 16.4 (P= 0.000) with sensitivity 100 % and specificity 88.2%. ROC curve analysis of ferritin for pneumonia mortalitiy prediction proved that the area under the curve is 0.941 with cutoff level equal to 264.0 (P=0.001) with sensitivity 83.3% and specificity 88.2 % (Fig. 2).
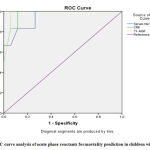 |
Figure 2: ROC curve analysis of acute phase reactants for mortality prediction in children with pneumonia. |
| Test Result Variable(s) | AUC | SE | p | Asymptotic 95% CI | Positive if Greater Than or Equal Toa | Sensitivity% | Specificity% | |
| Lower Bound | Upper Bound | |||||||
| Serum ferritin | .941 | .046 | .001 | .852 | 1.000 | 264.0 | 83.3 | 88.2 |
| CRP | .973 | .024 | .000 | .926 | 1.000 | 16.4 | 100.0 | 88.2 |
| AGP | .980 | .019 | .000 | .944 | 1.000 | 20.50 | 100.0 | 94.1 |
Discussion
This study was undertaken to clarify the significant role of acute phase reactant proteins in correlation with the modified pneumonia prognostic score to assess the disease severity and outcome in children. To fulfill this purpose, a total of eighty infants were enrolled in this study, 37 males and 43 females with male to female ratio 1:1.16. They further were categorised into two groups: control group (n= 40) and case group (n=40) according to diagnostic criteria of pneumonia. Non survivor patients were representing 6/40 (15%) showing the severity and the morbidity of CAP among Egyptian children. In our study, the cases were 62.5% males and 37.5% females and the controls were 57.5% males and 42.5% females reflecting more affection of males by pneumonia but with no significant difference between the two groups (p= 0.648). A previous meta analysis study recorded that male children are more prone to acquire pneumonia than female children. This could be due to by a stronger immune defense mechanisms in girls and narrower peripheral airways in boys during the first years of life ²⁰. No significant difference between age of cases and controls, where; mean age of the cases and controls were 13.85±3.4 months and 15.83±4.4 months respectively, so both groups were age matched (p=0.09). The mothers of case group in our research had a significant lower level of education than those of control group (p=0.009). Similar findings were confirmed by Abdel Maksoud et al. ⁶, while another study by Jackson et al. ²⁰ showed that the association between low mother education level and severe respiratory infection is not proved. They considered that risk factors rather than mothers’ education such as having past history of illness can affect their behavior and reduce the risk of acquiring pneumonia.
A highly significant difference between the two studied groups regarding the residence; as most of the cases were from rural areas (65%), while most of the control group were from urban areas (80%), (p<0.001). The predominance of pneumonia in rural areas could be explained by poor sanitation, increased family number and overcrowding that increase the risk of exposure to infection 21. This finding doesn’t match with the study by Fadl et al. 22 who found no significant difference between the under five children with pneumonia and healthy controls as regarding residence. There was a significant statistical difference between the cases and controls regarding the type of feeding within the first year of life; where the artificial feeding was more in the cases (52.5%) than in the control group (32.5%), (p=0.023). As 55% of the control group received breast feeding, while 25% of cases received breast feeding . Lack of breast feeding is a golden risk factor for acquiring pneumonia and increasing mortality among children younger than five years in the developing countries 23. The breast milk contains several immune protective and nutritive substances that protect babies as their own immune systems have not developed yet 24. There was a significant statistical difference between the cases group and control group regarding family number, crowding index and birth order (p<0.001) . These results match with those of Fadl et al. 22, but they are in contradictory to the study done by Jackson et al. 20. This reflects the strong and combined association between socioeconomic risk factors and health. Overcrowding and bad home ventilation are strongly linked with higher incidence of pneumonia among children 25 . Having higher birth order (third child or more) increases the likelihood of having pneumonia. Large number of children is associated with maternal inattention to her kids and facilitates the spreading of infection 26. The present study showed that weight is significantly more in the healthy controls than in the cases (p<0.001). Having smaller weights may predispose to increasing risk of pneumonia due to lower immunity and impaired lung functions 27.
TLC was significantly higher in the case group when compared with the control group (p=0.024). These results come in concordance with those of Abdel Maksoud et al. 6 wherease, in the study of Hussain et al. 28 there was no significant difference between the cases and controls regarding TLC.
In the current study, hemoglobin level showed a significant decrease in the cases when compared to the controls reflecting that anemia may be a predisposing factor to infection susceptibility in this young age. These findings paralleled with those of Mourad et al. 29. A study done by Malla et al. 30 found that reduced hemoglobin is the main cause of acute lower respiratory tract infection. Serum iron also revealed significant depletion in children with pneumonia than controls. Similar findings were recorded by Hussain et al. 28. Iron seems to share in immunity components causing lung injury 28.
The mean ferritin level in our research displayed significant increase in the cases in comparison to the controls. The same findings were registered by Choi et al. 31. However, Abdel Maksoud et al. 6 observed that ferritin level is significantly lower in children with pneumonia than in controls. This could be attributed to that 70% of their cases had iron deficiency anemia.
Serum ferritin level was negatively correlated with the mean platelets count (p=0.004), while there was positive correlation with CRP, AGP and modified PIRO score (P<0.001). It didn’t correlate with sex and age. This was confirmed by Thurnham et al. 12 who reported that age and sex don’t affect the ferritin level associated with the inflammatory status. This indicated that the increase in ferritin in association with inflammation is proportional to the baseline ferritin concentration within the group of participants. Also, Thurnham et al. 32 supported the correlation among ferritin, CRP and AGP and confirmed that at least two acute phase proteins must be measured during inflammation to cover the whole phase of the disease. These investigators found that in patients with covert infection as indicated by elevated CRP and/or AGP, an increase in ferritin concentration is recorded as ferritin increased rapidly at the onset of inflammation 33. Also as recommended by the WHO working group; the measurement of ferritin must be accompanied by the analysis of one or more acute phase reactants to detect the presence of infection or inflammation, because high ferritin thresholds in the presence of inflammation may mask underlying iron deficiency anemia 34.
In the present study, CRP achieved a significant statistical difference between the cases and the control groups being higher among the patients. Joeng et al. 35 stated that children affected by pneumonia have higher CRP level than the healthy controls. A study conducted by Xiao et al. 36 concluded that serum CRP is higher in children with pneumonia than healthy subjects denoting that the elevated CRP levels may be an essential risk factor for pneumonia occurence in children. On the opposite side, other studies didn’t support the significant difference regarding the CRP measurement between the two studied groups (P > 0.05) although it was higher in the cases than controls 37. It has been found that CRP level is constantlyhigh in bacterial pneumonia, but only slightly increases in severe acute respiratory syndrome 38. Koster et al. ⁴¹ demonstrated that serum CRP levels are positively correlated with pneumonia and also the study of Mintegi et al. 40 that was done on 188 children lower than three years presented to hospital emergency roomsproved that CRP serum levels may be useful in prediction of the risk of pneumonia in children with high fever.
CRP was positively correlated with iron, ferritin, AGP and modified PIRO score (p<0.001) while it was negatively correlated with Hb and platelets (p<0.001) .In concordance with our results, CRP was positively correlated with AGP 37 and ferritin 32.
AGP, is a 41–43 kDa protein of immunoglobin family and is considered an important acute-phase proteins 41. It has the ability to bind and transfer several inflammatory ligands. AGP is considered to be a sensitive diagnostic of inflammaton or acute infection42. In the current research, the mean value of AGP in children with pneumonia was statistically higher than the healthy controls ( p<0.001) . This finding comes in line with a recent study by Huanying et al. 37 . Our study also showed that as a risk factor of pneumonia, AGP has a diagnostic value whereasa combination of AGP with other phase reactants could improve the efficiency of differential diagnosis.
As regarding AGP in the present study, it correlated positively with ferritin and CRP (p<0.001). On the contrary, it correlated negatively with Hb, iron and platelets (p<0.001, p=0.011, p<0.001 respectively) and it did not correlate with TLC. Huanying et al. 37 recorded significant positive correlation between AGP and CRP levels but, no significant correlation between AGP concentrations, gender distribution and WBC.
In the current approach, AGP is positively correlated with the modified PIRO severity score. To the best of our knowledge, our study is the first one to correlate clinical severity score with AGP. Modified PIRO score, a simple scoring system for predicting pneumonia outcome, was also used to evaluate our patients. In our study, 11 and 22 of our cases were stratified into low and moderate risk groups respectively while the high and very high risk categories were comprised by 3 patients each. The mortality was 3 children (7.5%) from the very high modified PIRO, 2 children (5%) from the high score and one child (2.5%) from the moderate risk score. A study of Araya et al. 9documented mortality rateof 0% for a low PIRO score (0/708 patients), 18% (20/112 patients) for a moderate score, 83% (25/30 patients) for a high score and 100% (10/10 patients) for a very high modified PIRO score (P < 0.001). This research group utilized this score to discriminate the risk of mortality in children admitted with CAP and thus it could be a reliable tool for patients selection for ICU admission 43. Whereas this tool is modified from that designed for CAP in adults, it looks to be a good prognostic tool10.
On comparing the four risk groups of the modified PIRO score regarding CBC parameters, we noted high statistically significant lower mean value of the haemoglobin and platelets in the group of patients of the very high risk of mortality as compared to the other three groups of patients. TLC mean value was lower in the group of the high risk in comparison with the other three risk groups, but there was no significant statistical difference. Our three inflammatory markers; CRP, AGP and ferritin values showed the highest significant levels in the very high risk group of patients .So, modified PIRO score correlates well with the inflammatory markers.
In this study, we proved that modified PIRO score is a good predictor of mortality, as only one patient died from moderate risk group, two patients died from high risk group and another three patients died from very high risk. These findings are in the harmony with the 2011 Pediatric Infectious Diseases Society/ Infectious Diseases Society of America (PIDS/IDSA) guidelines used in the treatment of community acquired pneumonia in children that recommended consideration of acute phase reactants such as CRP to validate severity and mortality scores. The inclusion of these acute phase reactants could lead to modest improvement in predicting outcome enabling physicians to hospitalize risky children early in order to reduce mortality 2.
In this study, we confirmed that the initial values of acute phase reactants (AGP, CRP and ferritin) are significantly higher in non-survivors (children with 30-day mortality) than survivors which are similar to the conclusions of Kellum et al. 44 and Menendez et al. 45. The diagnostic value of 30-day mortality prediction was assessed and evaluated by ROC curve analysis for acute phase reactants. ROC curve analysis of AGP for mortality prediction in children with pneumonia identified that the area under the curve is 0.980 ( more close to one better diagnostic value), (p=0.000) with cutoff level equal to 20.50, with sensitivity 100% and specificity 94.1%. ROC curve analysis of using CRP in mortality prediction showed that the area under the curve is 0.973, (p= 0.000) with cutoff level equal to 16.4, with sensitivity 100 % and specificity 88.2% . ROC curve analysis of ferritin for pneumonia mortalitiy prediction showed that the area under the curve is 0.941, (p= 0.001) with cutoff level equal to 264.0, with sensitivity 83.3% and specificity 88.2 %. AGP showed the best area under the curve, sensitivity and specificity .These results are in concordance with those of Huanying et al. 37 which presented that ROC curve analysis for using AGP in pneumonia mortality prediction was better than that of CRP.
In conclusion, Acute phase reactants (AGP, CRP and ferritin) displayed statistically significant higher levels in the cases of pneumonia than in the healthy controls, non-survivors than survivors and positive correlation with the modified PIRO score, so the present investigation provides a distinct evidence for the prominence of acute phase reactants in comparison with the clinical scores in predicting early high risk prognosis of pneumonia in children.
Further researches having larger sample size with serial measuring AGP, CRP and ferritin levels are needed to establish their reliability in early prediction of pneumonia prognosis and outcome in children.
Acknowledgment
None
Conflict of interest
All authors declared that they have no conflict of interest.
Funding source
none
References
- Johnson WBR and Adulkarim A.A. Childhood pneumonia in developing countries. African journal of respiratory medicine.8(2):4-9 (2013).
- Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis.53 (7): e25-e76 (2011).
CrossRef - Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and aetiology of childhood pneumonia. Bulletin of the World Health Org. 86: 408-416 (2008).
CrossRef - Katrina V Deardorff, Eric D McCollum, and Amy Sarah Ginsburg. Pneumonia Risk Stratification Scores for Children in Low-Resoruce Settings: A Systematic Literature Review. Pediatr Infect Dis J . 37 (8): 743-748 (2018).
CrossRef - Philip Ayieko and Mike Arabic. Case Management of Childhood Pneumonia in Developing Countries. Pediatr Infect Dis J. 26 (5): 432-440 (2007).
CrossRef - Abdel-Maksoud HM , Hasan KA and Helwa MA. Evaluation of iron deficiency Anemia as a predisposing factor in the occurrence of pneumonia in children. Trends in Medical Research. 11 (2): 69-75 (2016).
CrossRef - Macpherson L, Ogero M, Akech S, Aluvaala J, Gathara D, Irimu G, English M and Agweyu. A Risk factors for death among children aged 5-14 years hospitalised with pneumonia: a retrospective cohort study in Kenya. BMJ Global Health .4(5):e001715 (2019).
CrossRef - Fine MJ, Auble TE, and Yealy DM . A prediction rule to identify low risk patients with community acquired pneumonia. N Engl J Med. 336 (4): 243-250 (1997). D
CrossRef - Araya S, Lovera D and Zarte C .Application of a prognostic scale to estimate the mortality of children hospitalized with community acquired pneumonia. Pediatr Infect Dis. J. 35(4):396-373(2016)
CrossRef - Uwaezuoke SN and Ayuk AC. Prognostic scores and biomarkers for pediatric community-acquired pneumonia: how far have we come? Pediatric Health Med Ther.8:9-18(2017).
CrossRef - Sebastein Gibot, Aurelie Cravoisy, Bruno Levy, Marie-Christine Bene. Soluble Triggering Receptor Expressed on Myeloid Cells and the diagnosis of pneumonia. N Engl J Med. 29; 350(5):451-458 (2004).
CrossRef - Thurnham DI, Mburu AS, Mwaniki DL, Muniu EM, Alumasa F and de Wagt A. Using plasma acute-phase protein concentrations in interpret nutritional biomarkers in apparently healthy HIV-1 seropositive Kenyan adult. Br J. Nutr. 100: 174-82(2008).
CrossRef - Naomi Shinoda, Kevin M Sulivan, Katie Tripp, Jügen G Erhardt, Bridgette MH Haynes, Victor J Temple and Bradley Wooduff. Relationship between markers of inflammation and anaemia in children of Papua New Guinea. Public Health Nutrition.16 (2): 289-295 (2012).
CrossRef - Luo Z, Lei H, Sun Y, Liu X and Su D. Orosmucoid, an acute response protein with multiple modulating activities. Physiol Biochem . 71:329-340(2015).
CrossRef - Beata Pucher, Magdalena Sobieska, Michal Grzegorwski, and Jaroslaw Szydlowski. The Acute Phase Proteins Reaction in Children Suffering from Pseudocroup. Mediators of Inflammation. Article ID 6518308,7page (2019).
CrossRef - El-Wakeel MA, El-Kassas GM, Fathy GA, El-Wakkad AS, Sebaii HM, El-Zayat SM. Diagnostic and prognostic values of high sensitive c-reactive protein, tumor necrosis factor and interleukin-1β in neonatal sepsis. Aust J Basic Appl Sci.6:224-8 (2012).
- Bryan M. Gannon, Marshall J. Glesby, Julia L. Finkelstein, Tony Raj, David Erickson and Saurabh Mehta. A point-of –care assay for alph-1 acid glycoprotein as a diagnostic tool for rapid mobile-based determination of inflammation. Current Research in Biotechnology. 1: 41-48(2019).
CrossRef - World Health Organization. Pocket book of hospital care for children: guidelines for the management of common illnesses with limited resources. 2nd Geneva: World Health Organization (2013).
- Addison GM, Beamish MR, Hales CN, Hodgkins M, Jacobs A and Llewllin P. An immunoradiometric assay for ferritin in the serum of normal subjects and patients with iron deficiency and iron overload. J Clin Path.25: 326-329 (1972).
CrossRef - Jackson S, Mathews KH, Pulanic D, Falconer R, Rudan I. and Compbell H. Risk factors for sever acute lower respiratory infections in children-a systematic review and meta-analysis. CroatianMedical Journal. 54 (2): 110-21(2013).
CrossRef - Shaaban L. Dilemma of community –acquired pneumonia. The Egyptian Journal of Chest Diseases and Tuberculosis. 68: 1-4 (2019).
- Fadl N, Ashour A and Muhammed Y. Pneumonia among under-five children in Alexandria Egypt: a case-control study. Journal of the Egyptian Public Health Association.95,14(2020).
CrossRef - Roberts JT, Carnhan E. and Gakidou E. Can breastfeeding promote child health equality? A comprehensive analysis of breastfeeding patterns across the developing world and what we can learn from them. Med. 11 (1):254(2013).
CrossRef - Steller N, Bhatia J, Parish A and Stallings VA. Feeding healthy infants, children and adolescents. In: Kliegman RM, Stanton BF, Geme JWS, Schor NF, Behaman RE, editors, Nelson textbook of pediatrics. 19th ed. Philadelphia: Elsevier Sauders. 160-1(2011).
CrossRef - Zheng X, Qian H, Zhao Y, Shen H, Zhao Z and Sun Y. Home risk factors for childhood pneumonia in Nanjing China. Chin Sci Bull. 58: 423-6 (2013).
CrossRef - Pina JC, Moraes AS, Freitas KM and Mello DF. Role of primary health care in child hospitalization due to peneumonia: a case-control study. Rev Latino-Am Enfemagem. 25(0):e2892(2017).
CrossRef - Raeezani M, Aemmi S and Moghadam Z. Factors affecting the rate of pediatric pneumonia in developing countries; a review and literature study. Int J. Pediatr. 3 (6-2): 1173-81(2015).
- Hussain S, Gattoo I, Bhagat R, Shahzad N and Wani J. Correlation of Serum Iron Levels with Acute Lower Respiratory Tract Infections in Children. IOSR Journal of Dental and Medical Sciences. 14 (7): 71-76 (2015).
- Mourad S, Rajab M, Alameddine A, Fares M, Ziade F and Abou Merhi B. Hemoglobin level as a risk factor for lower respiratory infections in Lebanese children. North Am J Med Sci. 2: 461-466 (2010).
CrossRef - Malla T, Pathak OK and Malla KK. Is low hemoglobin level a risk factor for lower respiratory tract infection?. Indian J Pediatr. 73 (10): 881-883 (2006)
CrossRef - Choi Y, Jeon J and Oh J. Critical combination of initial markers for predicting refractory mycoplasma pneumoniae pneumonia in children: a case control study. Respiratory Research . 20 (1), Article number:193(2019).
CrossRef - Thurnham D, McCabe L, Haldar S, Wieringa F, Northrop C and McCabe G. Adjusting plasma Ferritin concentrations to remove the effects of subclinical inflammation in the assessment of iron deficiency: a meta-analysis. J. Clin Nutr. 92(3): 546-55 (2010).
CrossRef - Abd El-Shaheed A, El-Arab AE, Abou-Zekri M, El Wakeel MA, El-Kassas GM, Mohsen NA, Anwar M. A novel gluten-free meal as a nutritional therapy for Iron deficiency anemia in children with celiac disease. BIOSCIENCERESEARCH.1;15(1):207-14 (2018).
- World Health Organization, Centers for Diseases Control and Prevention Assessing the iron status of population. geneva, Switzerland: WHO Press. ISBN 9789241596107(2007).
- Jeong JE, Soh JE, Kwak JH, et al. Increased procalcitonin level is a risk factor for prolonged fever in children with Mycoplasma pneumonia. Korean J Pediatr. 61 (8): 258-63 (2018).
CrossRef - Xiao X, Long X,Hui-Lin S and Zhi-Hui X. Correlation between serum level of C-reactive protein and infant pneumonia: A meta–analysis. Experimental and Therapuetic Medicine. 9:2331-2338(2015).
CrossRef - Huanying F, Aiping Z and Shusheng Y. Elevation of serum alpha-1-acid glycoprotein in children with bronchial pneumonia caused by Mycoplasma pneumoniae infection. Research Square(2020).
- Ray S, Patel S, Kumar V, et al. Differential expression of serum/ plasma proteins in various infectious diseases: specific or nonspecific signatures. Proteomics Clin Appl. 8 (1-2): 53-72 (2014).
CrossRef - Koster MJ, Broekhuizen BD, Minnaard MC, et al. Diagnostic properties of C-reactive protein for detecting pneumonia in children. Respir107: 1087-1093(2013).
CrossRef - Mintegi S, Benito J, Pijoan J, et al. Occult pneumonia in infants with higher fever without source: a prospective multicenter study. Pediatr Emerg Care.26: 470-474 (2010).
CrossRef - Fournier T, Medjobi-N N and Porquet D. Alpha-1-acid glycoprotein. Biochim Biophys Acta.1482 (1-2): 157-71(2000).
CrossRef - Ceciliani F. and Lecchi C. The immune functions of α1 acid glycoprotein. Curr Protein Pept Sci.20 (6): 505-24 (2019).
CrossRef - Rello J, Rodriguez A, Lisboa T, Gallego M, Lujan W and Wunderink R. PIRO score for community-acquired pneumonia. A new prediction rule for assessment of severity in intensive care unit patients with community-acquired pneumonia. Crit Care Med.37 (2): 456-462 (2009).
CrossRef - Kellum JA, Kong L, Fink MP, et al. Understanding the inflammatory cytokine response in pneumonic and sepsis: Results of the Genetics and Inflammatory Markers of Sepsis (Gen IMS) Study. Arch Intern Med.167:1655-663 (2007).
CrossRef - Menendez R, Cavalcanti M, Reyes S, et al.Markers of treatment failure in hospitalized community acquired pneumonia. 63: 447-52 (2008).
CrossRef








