Thirunavukkarasu Jaishankar , Meera Shivasekar*
, Meera Shivasekar* and Vinodhini V. M
and Vinodhini V. M
Department of Biochemistry, SRM Medical College Hospital and Research Centre, SRMIST, Kattankulathur, Kancheepuram - 603 203, Tamil Nadu, India
Corresponding Author E-mail: meeras@srmist.edu.in
DOI : https://dx.doi.org/10.13005/bpj/2245
Abstract
The mechanism by which circulating ox-LDL and inflammatory indicators such as high sensitivity C-reactive protein may exert their impact on the development of CHD is still poorly understood. The study aims to measure the levels of circulating oxidized LDL and high sensitive C - reactive protein in CHD subjects. This cross-sectional study was conducted in the Department of Cardiology, General Medicine, and Master health check-up OP of SRM Medical college hospital and research centre, Tamil Nadu, India. A total of 182 subjects in which 91 CHD subjects and 91 healthy control in the age group of 30 to 55. ox-LDL and hs-CRP were measured by ELISA method and Lipid Profile is measured using Auto Analyzer AU480. Statistical analysis was done using the student ‘t’ test and Pearson correlation analysis was done for the comparison between two groups. The mean level ox-LDL and hs-CRP in CHD were elevated and statistically significant (p-value <0.001) compared to healthy controls. Ox-LDL was positively correlated with and hs-CRP. This study brings new insights that Ox-LDL and CRP may play a direct role in promoting the inflammatory component of atherosclerosis. Furthermore, more emphasis should be placed on these oxidative stress indicators in the prevention and treatment of CHD.
Keywords
Coronary Heart Disease; High-Density Lipoprotein; High Sensitive C - reactive protein; Low-Density Lipoprotein; Oxidized Low-Density Lipoprotein
Download this article as:| Copy the following to cite this article: Jaishankar T, Shivasekar M, Vinodhini V. M. The Effect of Circulating Oxidized LDL and High Sensitivity C-Reactive Protein on Coronary Heart Disease Susceptibility in a South Indian Population. Biomed Pharmacol J 2021;14(3). |
| Copy the following to cite this URL: Jaishankar T, Shivasekar M, Vinodhini V. M. The Effect of Circulating Oxidized LDL and High Sensitivity C-Reactive Protein on Coronary Heart Disease Susceptibility in a South Indian Population. Biomed Pharmacol J 2021;14(3). Available from: https://bit.ly/3z5ex2l |
Introduction
Coronary Heart Disease is a leading cause of mortality in India.CHD is often regarded as a complex condition influenced by both hereditary and environmental factors (Pranavchand et al., 2013). CHD is increasing rapidly in Indian people and manifesting at a younger age (Strong et al., 1999), and it has been estimated that approximately 10% of those CHD subjects were under the age of 45, has a high risk of morbidity and long-term mortality, and thus poses a serious burden on the family and society (Fournier et al., 2004).
Clinically, identifying risk factors is problematic due to conventional risk variables that do not appear in young people with CHD in a unique way (Cole et al., 2004). Epidemiological research also revealed that several risk variables, such as smoking, hypertension, and dyslipidemia, played a larger influence in young participants (Allen et al., 2001). Among the factors that contribute to the development of atherosclerosis, lipid deposition has received the greatest attention. Several studies have indicated that for the prevention of CHD, statin treatment is used to lower LDL-cholesterol, and high levels of LDL-cholesterol are well-known as a key risk factor for CHD (Steinberg et al., 2002).
Low-density lipoprotein (LDL), the main transporter of cholesterol, accumulates in the intima and on the surface of endothelial cells, where it increases the production of adhesion molecules and chemo attractants by promoting the adherence of circulating monocytes to the endothelium. Following adhesion, monocytes move into the intima, develop into macrophages, internalize and accumulate cholesterol in cells, and finally form foam cells (Steinberg et al., 2009). Because LDL receptors cannot collect cholesterol in macrophages, increasing intracellular cholesterol down-regulates the LDL receptor via the sterol regulatory element-binding protein (SREBP) mechanism.
Certain changed forms of LDL, such as acetylated LDL and oxidized LDL, on the other hand, are eagerly taken up by macrophages via scavenger receptors, resulting in significant cholesterol buildup and foam cell production due to scavenger receptor up-regulation by oxidized LDL (Horton et al., 2002). According to the so-called LDL oxidation theory of atherosclerosis, LDL oxidation leads to atherosclerosis. Endothelial cells and monocytes are stimulated toward increased inflammatory cytokines, chemokines, adhesion molecules, and monocytes/macrophages are stimulated toward enhanced tissue factor, matrix metalloproteinase, apolipoproteinase and scavenger receptors leads to the formation of foam cell in macrophages and atherosclerotic lesions. There are several proposed methods by which LDL might be oxidized by different enzymes in the intimal wall. Lipoxygenase is an internal oxidation enzyme that directly oxygenates polyunsaturated fatty acids. It is a non-heme iron-containing dioxygenase enzyme (Parthasarathy et al., 1989). Lipoxygenase oxidises LDL through direct (enzymatic) and indirect (non-enzymatic) processes, producing oxidant radicals that contribute to non-enzymatic lipid peroxidation.Myeloperoxidase, like lipoxygenase, is linked to inflammation and oxidative stress (Hazen et al., 1997). MPO is a high cationic protein that may attach to endothelial cells, leukocytes, and LDL.MPO generates many reactive oxygen species that oxidise the lipid and protein of LDL, and the interaction of MPO and LDL may increase LDL oxidation (Schindhelm et al., 2009).
The conversion of LDL to Oxidized LDL is a critical event in the oxidation hypothesis of atherogenesis (Leopold et al., 2008). Endothelial dysfunction and plaque disruption are induced by the overproduction of reactive oxygen species by endothelial cells as a result of oxidative alterations (Hadi et al., 2005). Endothelial dysfunction caused by oxidized LDL and CRP leads to the development of atherosclerosis (Park et al., 2015). Increased oxidative stress causes CRP overproduction. Endothelial cell-matrix proliferation promotes basement membrane thickening, which contributes to atherosclerosis. It also boosts the enzyme involved in collagen production and increases endothelial cell collagen IV and fibronectin synthesis. As a result, there is an excess of collagen cross-linking and an increase in extracellular matrix protein synthesis in the vessel wall (Elaine et al., 2006).As a result, there is a buildup of LDL-C particles, which are more likely to be oxidized. As a result, endothelial cell injury occurs, which stimulates inflammatory changes; adhesion and proliferation of vascular smooth cell (Dania Mohty et al., 2008).Endothelial cell dysfunction and coronary heart disease both play important roles in the development of end-organ damage.Endothelial dysfunction is described as the inability of the vascular endothelium to perform its usual function in vasodilation.The inflammatory response is important in the endothelial function.Endothelial dysfunction disrupts the balance between endothelium-derived contracting and relaxing factors due to endogenous and external effectors (Angela et al., 2011).Endothelial dysfunction caused by oxidized LDL and CRP contributes to the development of atherosclerosis.In our study, we not only assessed the quantity of circulating oxidized LDL in the circulation, but also the oxidation ratio of LDL (ox-LDL/TC, ox-LDL/HDL-C, ox-LDL/LDL-C), as well as high sensitivity C- reactive protein in the diagnosis of CHD.
Materials and Methods
Study Design
This cross-sectional study was conducted at SRM Medical College Hospital and Research Centre, Chennai, Tamil Nadu, India.
Inclusion Criteria
Group – 1 (CHD subjects)
The CHD Subjects including both males and females selected based on coronary angiography, chest pain lasting more than 30 minutes, elevated ST-elevation > 0.1 mV on at least two adjacent electrocardiographic leads, and an increase in Creatine kinase (CK) to peak levels at least 2-fold the upper limit of normal values (Prabhat et al., 2016). (Kristian et al., 2007).
Group – 2 (Healthy Controls)
The control group includes those who have no clinical or ECG indications of CHD and no history of a previous CHD or stroke, Diabetes Mellitus, Hypertension, smoking, Dyslipidemia, or a family history of CHD.
Exclusion Criteria
The subjects who were on treatment for renal failure, cancer, autoimmune diseases were excluded.
Study Settings
This cross-sectional study was carried out on subjects attending the Cardiology and Medicine outsubjects departments at SRM Medical College Hospital and Research Centre in Chennai, Tamil Nadu, India, from June 2019 to December 2019.The institutional ethics committee (ECN: 1513/ICE/2018) accepted the study protocol.There were a total of 182 subjects that were age and sex matches in the 30-55 year age range. The control subjects were also taken from Master health check-up Programme and General Medicine OP in SRM Medical College Hospital and Research Centre, Chennai, Tamil Nadu, India.
Anthropometric Measurement
The study was described to the subjects, and signed informed permission was acquired.The baseline examination includes a medical history, a family history of CHD, diabetes, and a physical examination.The 12-lead resting electrocardiogram was used as part of the physical assessment. BMI, weight (kg), height (metres), waist circumference (cm), hip circumference (cm), waist-hip circumference ratio, systolic and diastolic arterial blood pressures were all assessed.
The BMI was based on the Standard Agreement Statement for the Indian population (Misra et al., 2009). A questionnaire was used to assess cigarette smoking, physical activity (including leisure and occupational activity) over the previous year and the previous week.
Measurement of laboratory parameters
After an overnight fast, a blood sample (5mL) was taken in sodium citrate and plain vacationer under aseptic conditions. 2mL of blood was drawn for the assessment of glucose and lipid profile (Total cholesterol by Cholesterol Oxidase method, Triglycerides by Glycerol peroxidase technique, HDL-C and LDL-C by Direct method). The Beckman Coulter Auto analyzer was used to quantify high-density lipoprotein (HDL) cholesterol (HDL-C), TC/HDL-C ratio, and LDL-C/HDL-C ratio (AU480).
Measurement of oxidized LDL-C
3mL of blood was allowed to clot for 30 minutes before being centrifuged at 2500 RPM for 10 minutes to quantify oxidized LDL.The Ox-LDL was calculated using an ELISA kit (Bioassay Technology Laboratory Co., Ltd, China) (Catalogue No: CSB-E07931h) based on the direct sandwich technique, in which two monoclonal antibodies are directed in contrast to distinct antigenic components on the oxidized Apo-lipoprotein B molecule. Absorbance is measured at 450 nm.
Measurement of hs-CRP
3 mL of blood was clotted for 30 minutes before being centrifuged at 2500 RPM for 10 minutes to quantify oxidized LDL. Hs-CRP was estimated using the ELISA kit (Biosource Laboratory) (Catalogue No: MBS2506093) based on the direct sandwich technique. Samples are placed in the micro-ELISA plate wells and mixed with the appropriate antibody.Then, a biotinylated detection antibody specific for Human hs-CRP and an Avidin-Horseradish Peroxidase (HRP) conjugate are added to each micro plate well and incubated.The enzyme substrate reaction is halted by the addition of stop solution, and the color changes to yellow. The OD value is proportional to the concentration of Human hs-CRP. Human hs-CRP concentration is determined by comparing the OD of the samples to the standard curve.A spectrophotometer at 450 nm ± 2 nm is used to measure optical density (OD).
Statistical Analysis
The Statistical Package for the Social Sciences(SPSS) version 21 was used to analyze all of the data.The data was given as the mean ± standard deviation (SD). The difference between the mean levels of several parameters was examined using the student’s t-test. Pearson’s correlation equation was used to evaluate the relationship between distinct variables. The p-value of 0.05 was deemed statistically significant.
Results
This research enrolled a total of 182 people. There were 86(94.5%) male CHD subjects and 5(5.49%) female CHD subjects.And as control subjects, 78(85.7%) were male and 13(14.2%) were female. The majority of CHD subjects are between the ages of 40 and 50, whereas the majority of control subjects are between the ages of 30-45. 27 CHD subjects with a CHD family history as shown in [Table 1], BMI, waist circumference, waist hip ratio, and systolic blood pressure were significantly (p0.05) higher in CHD subjects than in controls.
Table 1: Demographics characteristics of Coronary Heart Disease Subject and Healthy Controls
| Variables | Controls (n=91) |
CHD subjects (n=91) |
p-value |
| Mean age (years, mean ± S.E.M.) | 41.8 ± 9.7 | 42.3 ± 10.5 | NS |
| Male Sex (%) | 78(85.7%) | 86(94.5%) | – |
| Female Sex (%) | 13(14.2%) | 5(5.49%) | – |
| Body mass index (kg/m2) | 21.91±0.37 | 23.47±0.35 | < 0.001 |
| Waist circumference (cm) | 90.9 ± 10.1 | 98.8 ± 9.6 | < 0.001 |
| Waist to hip ratio | 0.94±0.02 | 1.01±0.01 | 0.004 |
| Systolic blood pressure (mm Hg) | 109.73 ±18.32 | 122.38±16.57 | 0.197 |
| Diastolic blood pressure (mm Hg) | 77.69 ±6.95 | 81.58 ±13.26 | 0.010 |
BMI= Body mass index, SBP=Systolic blood pressure DBP= Diastolic blood pressure
*P value < 0.05 is considered significant; NS-Not significant; *** Very highly significant;
**Highly Significant.
The study found that FBG, Total Cholesterol, Triglyceride, LDL-C, VLDL-C, LDL/HDL ratio, and Total Cholesterol/HDL ratio are significantly higher in these subjects when compared to the control shown in [Table 2].The mean HDL-C levels did not differ significantly between subjects with CHD.When comparing CHD subjects to controls, the mean levels of ox-LDL [Figure 1] and hs-CRP indicate a statistically significant rise.BMI, Waist Circumference, Waist Hip Ratio, Total Cholesterol, Triglyceride, LDL-C, VLDL-C, TC/HDL Ratio, and LDL/HDL Ratio were all strongly associated with ox-LDL. Furthermore, ox-LDL was shown to be adversely associated with FBG and HDL-C.The ox-LDL/HDL ratio was shown to be significantly linked to BMI, Waist Circumference, Waist Hip Ratio, and lipid biomarkers such as Triglyceride, LDL-C, VLDL-C, TC/HDL Ratio, LDL/HDL Ratio, and hs-CRP. Furthermore, the ox-LDL/HDL ratio was shown to be adversely linked to FBG, Total Cholesterol, and HDL-C.The ox-LDL/LDL ratio was significantly associated to BMI, Waist Circumference, Waist Hip Ratio, Triglyceride, HDL-C, VLDL-C, TC/HDL Ratio, and hs-CRP.
Table 2: Comparison of Biochemical Parameter between Coronary Heart Disease Subjects and Healthy Controls.
| Variable | Controls (n=91) |
CHD subjects (n=91) |
p- Value |
| FBG (mg/dl) | 90.24±4.18 | 94.29±6.98 | 0.065 |
| Total cholesterol (mg/dl) | 168.8±16.3 | 236.55±40.33 | < 0.001 |
| Triglyceride (mg/dl) | 84.6±30.5 | 159.7±69 | 0.391 |
| HDL-C (mg/dl) | 46±9 | 37.83±4.25 | < 0.001 |
| LDL-C (mg/dl) | 106.4±12.59 | 111.29±14.75 | 0.348 |
| VLDL (mg/dl) | 17.26±8.77 | 28.06±12.14 | < 0.001 |
| TC/HDL Ratio | 3.71±0.70 | 6.17±1.14 | < 0.001 |
| LDL/HDL Ratio | 2.35±0.53 | 4.22±0.75 | < 0.001 |
| ox-LDL (U/L) | 16.73± 3.55 | 41.53± 8.72 | < 0.001 |
| ox-LDL/ LDL Ratio | 0.15±0.016 | 0.37±0.08 | < 0.001 |
| ox-LDL/ HDL Ratio | 0.37±0.11 | 1.10±0.25 | < 0.001 |
| hs-CRP (mg/L) | 1.92±0.47 | 3.80±1.35 | < 0.001 |
FBG- Fasting blood Glucose, TC- Total Cholesterol, HDL- High density lipoprotein, LDL- Low density lipoprotein, VLDL- Very low-density lipoprotein, TG- Triglyceride. Values are expressed in Mean ± Standard Deviation.
*P value < 0.05 is considered significant; NS-Not significant; *** Very highly significant; **Highly Significant.
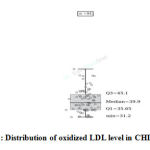 |
Figure 1: Distribution of oxidized LDL level in CHD subjects. |
Further more, the ox-LDL/LDL ratio was inversely associated with FBG, Total Cholesterol, LDL-C, and LDL/HDL Ratio hs-CRP is linked to BMI, Waist Circumference and Waist Hip Ratio, Triglyceride, HDL-C, LDL-C, VLDL-C, TC/HDL Ratio, ox-LDL, ox-LDL/HDL ratio, and ox-LDL/LDL ratio.hs-CRP was found to be adversely associated with FBG, Total Cholesterol, and LDL/HDL Ratio. [Table 3].
Table 3: The Pearson correlations analysis between ox-LDL and hs-CRP with other biochemical parameters in subjects with CHD.
| Variables | CHD Subjects | |||
| ox-LDL | hs-CRP | |||
| r-Value | p- Value | r-Value | p- Value | |
| BMI | 0.111 a | <0.001*** | 0.141 a | <0.001*** |
| Waist Circumference | 0.035 a | <0.001*** | 0.065 a | <0.001*** |
| Waist Hip Ratio | 0.296 a | <0.001*** | 0.286 a | <0.001*** |
| FBG | -0.106 b | <0.001*** | -0.152 b | <0.001*** |
| Total Cholesterol | -0.050 b | <0.001*** | -0.071 b | <0.001*** |
| Triglyceride | 0.145 a | <0.001*** | 0.188 a | <0.001*** |
| HDL-C | -0.148 b | <0.002** | 0.048 a | <0.002** |
| LDL-C | 0.069 a | <0.001*** | 0.020 a | <0.001*** |
| VLDL-C | 0.144 a | <0.001*** | 0.188 a | <0.001*** |
| TC/HDL Ratio | 0.680 a | <0.001*** | 0.541 a | <0.001*** |
| LDL/HDL Ratio | 0.010 a | <0.001*** | -0.023 b | <0.001*** |
| Ox-LDL/HDL Ratio | 0.854 a | <0.001*** | 0.721 a | <0.001*** |
| Ox-LDL/LDL Ratio | 0.783 a | <0.001*** | 0.705 a | <0.001*** |
| Ox-LDL | – | – | 0.853 a | <0.001*** |
| hs-CRP | 0.853 a | <0.0001*** | – | – |
a- Positive Correlation b- Negative Correlation
The linear Regression of Oxidized LDL significantly associated with Total Cholesterol (0.000), LDL-C (0.002), hs-CRP (0.000). This result indicates Oxidized LDL have higher regression with Total Cholesterol, LDL-C and hs-CRP. We didn’t found any significant regression of Oxidized LDL with other parameters observed in CHD subjects.[Table 4].
Table 4: Linear Regression Analysis for CHD in Non-Diabetic Subjects.
| INDEX | Ox-LDL | ||
| Β | 95% CI | P | |
| FBS | -0.003 | -0.013, 0.005 | 0.385 |
| TOTAL CHOLESTEROL | -0.061 | -0.035, 0.004 | 0.110 |
| TRIGLYCERIDE | 0.025 | -0.039, 0.046 | 0.870 |
| HDL-C | 0.001 | -0.017, 0.020 | 0.897 |
| LDL-C | 0.169 | 0.022, 0.099 | 0.002 |
| hs-CRP | 0.992 | 3.579, 3.773 | 0.000 |
Discussion
The oxidative hypothesis proposes that oxidation of LDL in the endothelium wall occurs prematurely in atherosclerosis.Ox-LDL leads to atherosclerotic plaque development by four distinct mechanisms: a) endothelial dysfunction, b) foam cell production, c) SMC migration and proliferation, and c) stimulation of platelet adhesion and aggregation.This might be explained by a variety of connections, such as impaired artery wall integrity and changes in lipid and lipoprotein concentrations (Yoshida et al., 2005). This study found a significant difference in TC, LDL-C, HDL-C, and triglyceride levels; nevertheless, the plasma level of LDL-C cholesterol was significantly greater in CHD subjects compared to controls, an important risk factor in the progression of atherosclerosis.LDL oxidation happens in two phases.In the early phases of LDL oxidation in vitro, oxidative alterations of LDL cholesterol can occur in the absence of changes in Apo-lipoprotein B100.This type of changed LDL is known as mildly oxidized LDL.
The lipids in highly oxidized LDL are cytotoxic and pro-apoptotic, stimulating smooth muscle cell proliferation and perhaps contributing to macrophage foam cells via PI3 kinase/Akt-dependent pathways.In the latter stages, the atherosclerotic lesion may produce necrotic development of the lesion, which promotes plaque rupture.We found a negative relationship between oxidized LDL and HDL-C in our research. HDL cholesterol levels, on the other hand, are connected to the risk of CHD because they prevent atherosclerosis by reducing the stimulatory effect of oxidized LDL on monocyte aggressiveness.According to the findings of a study done on middle-aged adults, there is a negative relationship between oxidized LDL and HDL-C(Sigurdardottir et al., 2002). This is related to the inverse antioxidant effect of HDL components.On the other hand, contradictory findings have been published on the mechanism by which oxidized LDL is an early stage of the illness that leads to atherogenesis.
Glycation of LDL-C may promote oxidative modification, and novel glycosylated end products may induce macrophages to produce ox-LDL(Levitan et al., 2009). Endothelial dysfunction and plaque disruption are caused by the generation of reactive oxygen species by endothelial cells via oxidative alterations (Santa et al., 2018).The high level of ox-LDL implies that inflammatory processes in subjects are exacerbated, which is linked to the development of CHD.In our study, subjects with CHD had higher levels of ox-LDL and hs-CRP than normal healthy people.Ox-LDL is favorably associated with hs-CRP, indicating that LDL oxidation contributes to systemic inflammation through causing CHD.Several studies have also found that the indicators of inflammatory activity are higher in CHD subjects (Ehara et al., 2018). High levels of inflammatory markers are linked to an increased risk of CHD development owing to inflammation in an intimal wall (Fredrikson et al., 2018).
CRP and OxLDL are actively interacting, suggesting that inflammation and oxidative stress are implicated in interconnected pathophysiological processes of cardiovascular disease. Ox-LDL and ox-LDL ratios, including ox-LDL/TC, ox-LDL/HDL-C, and ox-LDL/LDL-C, were related to coronary heart disease in our research.Similar to our findings, Huang et al. discovered that the oxidation ratio of LDL had a greater connection with coronary heart disease than plasma oxidized LDL. They also found that the ox-LDL level and LDL oxidation ratio (ox-LDL/TC, ox-LDL/HDL-C, and ox-LDL/LDL-C) were significantly greater in the CHD group than in the controls (P 0.001). (Huang et al., 2018).
Conclusion
The study shows that a high amount of circulating ox-LDL and hs-CRP is linked with a high risk of cardiovasculardisease.The ox-LDL and hs-CRP are superior indicators for distinguishing between subjects with coronary heart disease and normal healthy controls.ox-LDL levels and ox-LDL/LDL ratio appear to be lipoprotein abnormalities markers rather than the markers of oxidative stress.Furthermore, they serve as a predictive early risk sign in younger CHD subjects.
Financial support
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Allen J, Markovitz J, Jacobs DR, Knox SS. Social support and health behavior in hostile black and white men and women in CARDIA. Coronary artery risk development in young adults. Psychos. Med. 63, 609–618 (2001).
CrossRef - Angela M Thompson, Yonghong Zhang and Weijun Tong. Association of inflammation and endothelial dysfunction with metabolic syndrome, prediabetes and diabetes in adults from Inner Mongolia, China. BMC EndocrDisord. 2011; 11: 16.
CrossRef - Bredie SJ, de Bruin TW, Demacker PN, Kastelein JJ, Stalenhoef AF. Comparison of gemfibrozil versus simvastatin in familial combined hyperlipidemia and effects on apolipoprotein-B-containing lipoproteins, low-density lipoprotein sub fraction profile, and low-density lipoprotein oxidizability. Am J Cardiol (1995) 75:348–353
CrossRef - Cole JH, Sperling LS. Premature coronary artery disease: clinical risk factors and prognosis. Curr. Atheroscler. Rep. 6, 121–125 (2004).
CrossRef - Dania Mohty, Philippe Pibarot, Jean-Pierre Despres, Claude Cote, Benoit Arsenault, Amelie Cartier and Pierre Cosnay. Association between Plasma LDL Particle Size, Valvular Accumulation of Oxidized LDL, and Inflammation in Subjects with Aortic Stenosis. Arteriosclerosis, Thrombosis, and Vascular Biology. 2008;28:187–193
CrossRef - S, M. Ueda, T. Naruko, K. Haze, A. Itoh, M. et al., Elevated levels of oxidized low density lipoprotein show apositive relationship with the severity of acute coronary syn-dromes,Circulation103(2001), 1955–1960.
CrossRef - Elaine W Raines. The extracellular matrix can regulate vascular cell migration, proliferation, and survival: relationships to vascular disease. Int J ExpPathol. 2000 Jun; 81(3): 173–182.
CrossRef - Fournier JA, Cabezon S, Cayuela A. Long-term prognosis of subjects having acute myocardial infarction when 40 years of age. Am. J. Cardiol. 94, 989–992 (2004).
CrossRef - Fisher NM, Meksawan K, Limprasertkul A, Isackson PJ, Pendergast DR, Vladutiu GD. Statin therapy depresses total body fat oxidation in the absence of genetic limitations to fatoxidation. J Inherit Metab Dis (2007) 30:388–399
CrossRef - Fredrikson G.N, B. Hedblad, G. Berglund and J. Nilsson. Plasma oxidized LDL: a predictor for acute myocardial infarction? J Internal Medicine 253(2003), 425–429
CrossRef - Hadi HA, Carr CS, Al Suwaidi J. Endothelial dysfunction: cardiovascular risk factors, therapy, and outcome. Vasc Health Risk Manag. 2005;1(3):183-98. PMID: 17319104; PMCID: PMC1993955.
- Hazen SL, Heinecke JW. 3-Chlorotyrosine, a specific marker of myeloperoxidase catalyzed oxidation, is markedly elevated in low density lipoprotein isolated from human atherosclerotic intima. J Clin Invest 1997;99:2075–81.
CrossRef - Horton JD, Goldstein JL, Brown MS. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J Clin Invest 2002;109:1125–31.
CrossRef - Huang H, Mai W, Liu D, Hao Y, Tao J. The oxidation ratio of LDL: A predictor for coronary artery disease. Disease Markers (2008) 24(6): 341-349.
CrossRef - Kristian Thygesen, Joseph S. Alpert, and Harvey D. White. Universal Definition of Myocardial Infarction. Circulation. Volume 116, Issue 22, 27 November 2007, Pages 2634-2653.
- Leopold JA, Loscalzo J. Oxidative mechanisms and atherothrombotic cardiovascular disease. Drug Discov Today TherStrateg. 2008 Mar;5(1):5-13.
CrossRef - Levitan I, Volkov S, Subbaiah PV. Oxidized LDL: diversity, patterns of recognition, and pathophysiology. Antioxid Redox Signal. 2010 Jul 1;13(1):39-75. doi: 10.1089/ars.2009.2733. PMID: 19888833; PMCID: PMC2877120.
CrossRef - Misra,A, Chowbey P, Makkar B.M, Vikram,N.K. Consensus statement for diagnosis of obesity, abdominal obesity and metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management.J.Assoc.Phys 2009 India57,163–170.
- Ndrepepa G, Braun S, von Beckerath N. Oxidized low density lipoproteins, statin therapy and severity of coronary artery disease. ClinChimActa. 2005;360:178e186.
CrossRef - Park KH and Park WJ. Endothelial Dysfunction: Clinical Implications in Cardiovascular Disease and Therapeutic Approaches. J Korean Med Sci. 2015;30(9):1213–1225. doi:10.3346/jkms.2015.30.9.1213
CrossRef - Parthasarathy S, Wieland E, Steinberg D. A role for endothelial cell lipoxygenase in the oxidative modification of low density lipoprotein. Proc Natl AcadSci USA 1989;86:1046–50.
CrossRef - Prabhat Pandey, Rajendra Kumar Chandrakar, Pavan Kumar et al., Profile of coronary artery disease cases in diabetics and non-diabetics:acomparative prospective study. IntJAdv Med. 2016 Aug;3(3):579-585
CrossRef - Pranavchand R, Reddy B M. Current status of understanding of the genetic etiology of coronary heart disease. J Postgrad Med 2013;59:30-41.
CrossRef - Santa Mundi, MarikaMassaro, Egeria Scoditti, Maria Annunziata Carluccio. Endothelial permeability, LDL deposition, and cardiovascular risk factors—a review. Cardiovascular Research, Volume 114, Issue 1, 01 January 2018, Pages 35–52.
CrossRef - Schindhelm RK, van der Zwan LP, Teerlink T, Scheffer PG. Myeloperoxidase: a useful biomarker for cardiovascular disease risk stratification? ClinChem 2009;55:1462–70.
CrossRef - Sigurdardottir V; Fagerberg B; Hulthe J. Circulating oxidized low-density lipoprotein (LDL) is associated with risk factors of the metabolic syndrome and LDL size in clinically healthy 58-year-old men (AIR study). J Intern Med 252 :440 –447,2002.
CrossRef - Silverstein RL. Executive summary of the third report of The National Cholesterol Education Program (NCEP) expertpanel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA (2001) 285:2486–2497
CrossRef - Steinberg D. Atherogenesis in perspective: hypercholesterolemia and inflammation as partners in crime. Nat Med 2002;8:1211–7.
CrossRef - Steinberg D. The LDL modification hypothesis of atherogenesis: an update. J Lipid Res. 2009 Apr;50Suppl(Suppl):S376-81.
CrossRef - Strong JP, Malcom GT, McMahan CA. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the pathobiological determinants of atherosclerosis in Youth Study. JAMA 281, 727–735 (1999).
CrossRef - http://www.ndei.org/uploadedFiles/Common/NDEI/Treatment_Guidelines/ADA%202015%20Summary %20 PDF.pdf. Accessed 10 March 2016
- Yoshida H, Sasaki K, Namiki Y, Sato N, Tada N. Edaravone, a novel radical scavenger, inhibits oxidative modification of low-density lipoprotein (LDL) and reverses oxidized LDL-mediated reduction in the expression of endothelial nitric oxide synthase. Atherosclerosis 2005;179:97–102.
CrossRef








