Manuscript accepted on :22-Jun-21
Published online on: 05-07-2021
Plagiarism Check: Yes
Osama M Alshehri1* , Mohammed H Nahari1
, Mohammed H Nahari1 , Elhashimi E Hassan1
, Elhashimi E Hassan1 , Musab F Alqahtani2
, Musab F Alqahtani2 and Turki H Awaji3
and Turki H Awaji3
1Department of Clinical Laboratory Sciences, College of Applied Medical Sciences, Najran University, Najran, Saudi Arabia.
2Department of Medical Laboratory, Armed Forces Hospital, Najran, Saudi Arabia.
3Department of Blood Bank, Armed Forces Hospital, Najran, Saudi Arabia.
Corresponding Author E-mail: usamah2012@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2210
Abstract
The knowledge of Red blood cells polymorphism and blood group antigens prevalence at the local and regional levels is necessary for safe blood transfusion services. This study was aimed to estimate the prevalence of significant blood group phenotypes like ABO, Rh, and Kell among the Najran people of Saudi Arabia. The transfusion transmittable infection (TTI) rate and blood abnormalities among various blood types were assessed to ensure safe blood transfusion. ABO and Rh blood prevalence (n=970) and Rh phenotype polymorphism were estimated in over 531 unrelated donors. The blood samples were screened for certain TTIs like AHBC- Anti-hepatitis B core, HTLV-1- human T-lymphotropic virus type I, HCV- hepatitis C virus, HBsAg- Hepatitis B antigen, HIV- Human immunodeficiency virus, SIC- Sickle cell, MP- Malaria parasite, and SYP- Syphilis. The selected samples were also observed for blood abnormalities by performing a complete blood count (CBC). Out of 970 subjects, 966 were males, and only 4 were females. The O>A>B>AB blood groups were identified with 46.89, 29.3, 9.1, and 2.38% prevalence among Rh-positive phenotype. While in the Rh system, 87.6% and 12.3% of Rh positive and Rh negative was observed. Among 953 samples, the prevalence of seropositive donors was approximately 5.66%. The screening showed about 5.036, 0.104, 0.314, 0.209, 2.18, 0.104, and 0.209% positivity for AHBC, HCV, HBsAg, HIV, SIC, MP, and SYP respectively. Results found that the frequency of D, C, E, c, and e were 99.9%, 67.98, 25.8, 77.9, 98.49%, respectively, in over 531 subjects. The e allele was more prevalent in Najran city. After observing the variations in the CBC parameters among the donors, it was perceived that about 28.78, 99.9, 29.41, and 31.6% of blood abnormalities were noticed for O, AB, B, and A blood groups, respectively. For blood banks and transfusion services, which play a significant role in the medical care of the patient, awareness of the distribution of the blood group is essential. Increasing consistency of blood donation programs would improve both donor satisfaction and motivation for potential donations of blood in near future.
Keywords
ABO; Blood Donation; Complete Blood Count (CBC); Kell; Rh Factor; Transfusion-Transmitted Infections (TTI)
Download this article as:| Copy the following to cite this article: Alshehri O. M, Nahari M. H, Hassan E. E, Alqahtani M. F, Awaji T. H. Prevalence of ABO, Rh and KELL Blood Group Types and Transfusion- Transmissible Infections (TTI) among Blood Donors in Najran City, Saudi Arabia. Biomed Pharmacol J 2021;14(2). |
| Copy the following to cite this URL: Alshehri O. M, Nahari M. H, Hassan E. E, Alqahtani M. F, Awaji T. H. Prevalence of ABO, Rh and KELL Blood Group Types and Transfusion- Transmissible Infections (TTI) among Blood Donors in Najran City, Saudi Arabia. Biomed Pharmacol J 2021;14(2). Available from: https://bit.ly/3xvsohS |
Introduction
The blood group antigens are inherited factors that are important for blood transfusion with different factors such as patterns of ancestry, genetic abnormalities, vulnerability to diseases, and demographic movement1. Until now, over 346 blood group antigens are present, which clusters inside 36 blood group frameworks, according to the International Society of Blood Transfusion (ISBT) congress2. In the development of blood transfusion, Karl Landsteiner’s finding of the ABO blood groups was a significant accomplishment. He won the Noble Prize, preceded by his discovery of Rhesus (Rh) antigen by Wiener3.
To maintain blood banks and safe blood transfusion facilities efficiently, awareness of the delivery of ABO and Rh blood groups at the local and regional levels is necessary. The Rh is known as the world’s leading blood group network, which differs across races4,5. The two popular blood forms in transfusion medicines are ABO and Rh-positive (Rh (D))6. In the blood group structure for ABOs, people are divided into four significant groupings of blood, including A, B, AB, and O. They are sub-divided into Rh-negative and Rh-positive due to the existence of antigens and agglutinins on their cell surface7. However, these blood groups are strongly polymorphic, and their allelic frequency distribution differs between regions of the world8. There are 18 distinct phenotypes, with anti-D, C, c, E, and e, with eight potential haplotype arrangements, which results in 36 genotypes in line with ISBT 0049.
The monitoring of blood banks in healthcare institutions is known to be a mandatory procedure for minimizing the onset of transfusion-transmitted infections (TTIs)10. In addition, between different regions of the world, the incidence of TTIs among blood donors often differs dramatically10. Any blood bank’s principal role is to provide patients with stable and compatible blood or blood supply on time. Any negligence of blood transfusion will endanger life with acute and delayed hemolytic transfusion (AHTR and DHTR) complications as well as in hemolytic disease in newborn (HDN)11. Currently, 36 antigens with an explicit immunogenic K antigen nature in the KELL system are associated with AHTR, DHTR, and HDN (ISBT-006)12.
A large proportion of TTIs is triggered by Human immunodeficiency virus (HIV) 1 and 2, hepatitis B virus (HBV), hepatitis C virus (HCV), syphilis, sickle cell anemia and human T-lymphotropic virus type I (HTLV-1)10,13. HTLV-1 is a virus linked with inflammation, a high-risk factor in adult T-cell leukemia/lymphoma for lymphocytic involvement, which arises primarily in Japan, South America, the Middle East, and other Austro-Melanesia countries13. The risk for transfusion-based Hepatitis B virus infection was subsequently reduced by introducing surface hepatitis B antigen (HBsAg) testing in blood donors14. Additional risk factors of TTI include inadequate surveillance systems, transfusion within family members, poor implementation of WHO rules and regulations, or the absence of reference screening tests such as Enzyme Immunoassays (EIA) or Nucleic Acid Testing (NAT)15. The new Minipol NAT technology (MP-NAT), which includes 96- blood donor data, is highly adaptive and has been embraced by several countries to eliminate “false reactive” outcomes16. However, TTI exposure in underdeveloped countries remains comparatively large, mainly because of the lack of infrastructure and funds to introduce sensitive testing techniques compared to developed countries17. ABO, Rh and KELL, and TTIs worldwide differed widely, and no reported data on this topic was available from Najran City, Saudi Arabia.
Donor selection is essential for protecting blood transfusion and eligibility policies and is intended to safeguard both the donor and recipients18. When blood is repeatedly donated, a person either achieves equilibrium at a lower level or becomes anemic19. Donors with comparatively low amounts of hemoglobin (Hb) or platelet count cannot contribute to blood donation20. Hb screening is a conventional aspect of donor collection. However, Hb alone is ineffective in diagnosing donors of the blood that have an iron deficiency but who have no anemia21. The electronic hematology analyzers can calculate red cell indices such as mean cell hemoglobin (MCH) and mean cell volume (MCV) with a high degree of specificity and precision. A drop in MCV and MCH generally represents an increasing iron shortage22. Thus the goal is to evaluate various serological tests relevant for TTI-related blood donors and the percentage of different ABO and Rh antigens of Najran city. Moreover, this study focuses on analyzing the CBC of selected donors to assess an iron deficiency.
Materials and Methods
The current study was conducted according to the Ethics Committee’s guidelines on Human Science at Najran University To engage in the research, all participants provided written consent.
Sample Size, Collection, and Selection Criteria
People from Najran City, Saudi Arabia, were among the population surveyed in our study. More than 966 unrelated people enrolled as donors to the Najran Hospital and took part in blood donation research. All the volunteers are from Saudi Arabia, where their details related to age, sex, clinical records were documented. The guidelines for blood transfusion were followed as per the National blood transfusion of Saudi Arabia. Blood donors have been estimated and recorded for infection history, complete blood picture (CBP), recurrent illnesses, and hemoglobin levels.
Blood Group Typing
The DiaMed method was used to conduct ABO and Rh D blood grouping by the gel column agglutination ID card process (ABO-Rh/Reverse Grouping, ID-Card, BIO-RAD, Switzerland). Blood of donors has been stored in EDTA anticoagulant tubes and processed further. Aluminum foil was removed from the selected microtubes as required by holding the ID-Card in the upright position. About 50 µL of red cell suspension was added to ID-Card. Later, the ID-Card was centrifuged for 10 min at 1030 rpm, and the results were read and recorded. Blood group classification was based on the reverse and forward groupings and a negative control outcome. The presence of the poor D-phenotype has been further checked for RhD. Donors were also graded as D-negative in weak D testing signal.
Sample Collection and Screening for Different Blood Types to Detect TTIs
The blood serum samples of donors have been subjected to nucleic acid testing (NAT) (Cobas TaqScreen, MPX Test version 2.0, Roche, Switzerland). Further, screening for HIV, HCV, HTLV-I/II, HbsAg, Syphilis, and HBC II by ELISA method (ABBOTT, ARCHITECT i1000, Germany) using kit method supplied by ARCHITECT (Germany) for HIV Ag/Ab Combo, Anti-HCV, HTLV-I/II, HBsAg qualitative II, Syphilis TP, and Anti-HBc II reagent kit, respectively. For SIC, qualitative determination of hemoglobin S (Hb-S) in blood was followed by using the kit SAS SICKLE CELL TEST (USA). Immunochromatographic membrane assay (USA) and rapid plasma reagin (RPR) method was followed to the detected malaria parasite and Syphilis, respectively.
Categorization of Rh Phenotypes by Antigen Typing
For Rh expanded phenotyping, a unique single monoclonal antiserum, detected by Antigen D and Kell (Antigens C, c, E, e and K), and a Gel test was performed (Bio-Rad ID-Card, Switzerland). Each ID-Card was reviewed to ensure that the results were accurate and followed the same procedure as described for blood group typing12.
Analysis of Complete Blood Count (CBC)
The CBC analysis was performed using an automated blood cell counter analyzer (SYSMEX XN 1000, Japan). All the tests were carried out by following standard procedures by assuring blood sample quality23.
Statistical Analysis
The percentage prevalence of different blood group types and Rh antigens, and Kell blood groups was estimated. The figures were shown in percentages. Further, student t-test (unpaired) was performed for CBC data analysis. GraphPad Prism version 8 was used to calculate the prevalence percentage and to generate the graphs. Statistical difference was set at p<0.05, and values of p<0.001 indicate high significance.
Results
Distribution of ABO and Rh Types
A current survey of 970 volunteer blood donors was conducted in Najran City to determine the level of ABO and Rh-blood distribution among Saudi citizens. There were more male donors than female donors, with 966 and 4 respective members. Fig. 1A outline the prevalence of male vs. female donors. Our findings on the distribution of ABO blood types revealed that, O positive blood category was most prevalent with 46.89%, followed by A positive, B positive, O negative, A negative, AB positive, B negative, and AB negative with 29.3, 9.11, 7.45, 4.24, 2.38, 0.41, and 0.21%, respectively (Fig. 1B). The Rh (D) positive and Rh (d) negative subjects are shown in Fig. 1C, where a more prevalent Rh-positive (87.6.%) than Rh negative (12.3%) was observed.
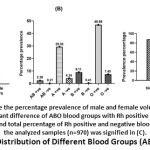 |
Figure 1: Distribution of Different Blood Groups (ABO and Rh) |
Distribution and Comparison of TTIs among Males and Females
In this report, we have tested the blood donors for various blood-transfusing infections. In 953 samples, the prevalence of seropositive donors was approximately 5.66 percent, which includes AHBC, HCV, HBsAg, and HIV) (Fig. 2A). The NAT analysis showed positive reactions for only two patients for HBV, and none of the patients tested positive for HIV and HCV. However, the serological screening showed about 5.037, 0.104, 0.314, and 0.209 seropositivity for AHBC, HCV, HBsAg, and HIV. Other TTI infection analysis for Sickle cell (SIC), malaria (MP) and syphilis (SYP) were found to be around 2.18, 0.104, and 0.209% positivity respectively. However, none of the studied donors showed positive for human T cell leukemia virus (HTLV) (Table 1). We also measured the percentage of seropositivity of TTIs in males as well as in females’ donors, out of the total studied blood donors and observed that none of the females (n=4) possessed any TTI’s, whereas 8.16% of males were found to be positive for the tested infections. Out of the total studied blood donors (n = 953), the percent TTIs in males (n = 78) were found to be appreciably in greater number when compared to females (n = 0) (Fig. 2B).
Table 1: Percentage Prevalence of Various TTIs among the Donors (n= 955) of Najran City.
| TTIs | Percentage of positive reaction | Percentage of negative reaction |
| AHBC | 5.037 | 94.963 |
| HTLV | 0.000 | 100.00 |
| HCV | 0.105 | 99.895 |
| HBs Ag | 0.315 | 99.685 |
| HIV | 0.210 | 99.790 |
| SIC | 2.183 | 97.817 |
| MP | 0.104 | 99.895 |
| SYP | 0.209 | 99.790 |
Where, AHBC- Anti-hepatitis B core, HTLV-1- human T-lymphotropic virus type I, HCV- hepatitis C virus, HBs-Ag- Hepatitis B antigen, HIV- Human immunodeficiency virus, SIC- Sickle cell, MP- Malaria parasite, SYP- syphilis.
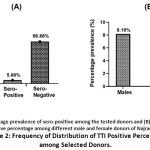 |
Figure 2: Frequency of Distribution of TTI Positive Percentage among Selected Donors. |
Prevalence of Various Rh Phenotypes
The distribution of alleles C, E, c, and e among the 531 donor volunteers has been calculated in the present analysis. Results found that the frequency of D, C, E, c, and e were 99.9%, 67.98, 25.8, 77.9, 98.49%, respectively (Fig. 3A). The prevalence of the K blood system was 12.05% in the sampled population. The most common Rh-positive haplotype frequency in the study was noticed for DCce with 33.40%, while in Rh D negative haplotype was observed for dce with 19.25% presence. The other forms of haplotypes identified in our analysis were DcEe, DCe, DCcEe, DCE, DcE, and DCee with 11.51, 21.51, 12.83, 1.13, 0.19, and 0.19% prevalence, respectively. The less common haplotypes noticed were DCE, DcE, and DCee (Fig. 3B). The haplotypes distribution among the Najran populace were found to be statistically different (p<0.05), with the highest prevalence of DCce type (33.4%) and least incidence of DcE and DCee (0.19% each) types.
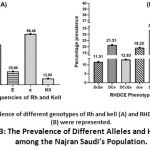 |
Figure 3: The Prevalence of Different Alleles and Haplotypes among the Najran Saudi’s Population. |
Selection of Donors based on Complete Blood Count (CBC)
The donors who had shown positive reaction for TTIs were eliminated, and further analysis of CBC was performed for those donors whose Rh phenotype data is available. It was perceived that among 500 donors with different Rh haplotype profiles showed variation in their CBC analysis, the donors with any abnormalities and low or high values than the reference range were excluded from the study. Table 2 represents the overall prevalence of different blood group types based on the demographic feature of the age. The age group between 31-40 yrs was found to donate more blood in almost all the blood group types. The blood donation was more in O type followed by A, B, and least contribution was observed in AB blood group donors.
Table 2: Demographic Distribution of Donors based on Age Factor.
| Variables | Donors (both Rh+ and Rh–) (n=500) | Frequency distribution (%) | ||||||
| Age group | O | AB | A | B | O | AB | A | B |
| <20 | 8 | 0 | 0 | 0 | 0.003 | 0 | 0 | 0 |
| 21-30 | 99 | 4 | 65 | 18 | 37.5 | 50.0 | 37.3 | 35.2 |
| 31-40 | 104 | 4 | 76 | 22 | 39.3 | 50.0 | 43.6 | 43.1 |
| 41-50 | 48 | 0 | 32 | 9 | 18.18 | 0 | 18.3 | 17.6 |
| 51-60 | 5 | 0 | 1 | 2 | 0.018 | 0 | 0.005 | 0.039 |
| Overall Total | 264 | 8 | 174 | 51 | 52.8 | 1.6 | 34.8 | 10.2 |
The Hb levels showed no variation (p<0.0001) among the selected donors and were in the acceptable range, where the mean values were 15.44, 16.39, 15.44, and 15.65 (g/dL) for O, AB, A, and B blood groups, respectively (Table 3). Similarly, the WBC and RBC count was also in the normal range (p<0.0001), except few abnormalities in WBC levels were noticed for few donors (n-63). The MCV and MCH levels were lower in few donors indicating few irregularities in the blood samples analyzed. The other parameters, like HCT, MCHC, and PLT, were in the acceptable range for all the donors. The values obtained for CBC did not show any significant variation (p<0.0001), and R2 values were around 0.9 for all the parameters, except for the WBC data for the AB blood group (Table 3). Further, since the data distribution was uneven, statistical analysis using student t-test (unpaired) was used to conclude statistical vs clinical significance. Accordingly, calculated t-value was significantly higher than the tabulated t- value at the level of significance used in all the cases except in WBC count of AB blood group. Hence, no significant (p>0.005) association can be considered between the tested variables. After observing the variations in the CBC parameters among the donors, it was perceived that about 28.78, 99.9, 29.41, and 31.6% of blood abnormalities were noticed for O, AB, B, and A blood groups, respectively (Table 4). In AB group, out of 8 people analyzed, 7 were showing statistical varied WBCs count indicating significant abnormalities at the tested population and the level of significance. The abnormality level was high in this particular group. However the since the sample size is less, mean is very much affected by the outliers. Thus the samples which showed TTIs and blood abnormalities can be eliminated for blood donation.
Table 3: Complete Blood Count (CBC) Parameters among Various Blood Group Types of Najran’s City.
| Blood group types | Parameters | Complete blood count (CBC) (n=500) | |||||||
| WBCs (x109/L) | RBCs (x1012 /L) | HGB (g/dL) | HCT (%) | MCV (/µm3) | MCH (pg/cell) | MCHC (Hgb/dL) | PLT (x109 /mm3) | ||
| Reference range | 4.5-10 | Males:
4.3- 5.9 Females: 3.5-5.5 |
Males: 13.5- 17.5
Females: 12-16 |
Males: 41-53
Females: 36-46 |
80-100 | 25.4-34.6 | 31-36 | 150-400 | |
| O | Min | 2.25 | 4.26 | 12 | 37.7 | 37.1 | 18.1 | 13.7 | 173 |
| Max | 12.43 | 16 | 18.6 | 56.3 | 96.4 | 33.5 | 35.8 | 481 | |
| Range | 10.18 | 11.74 | 6.6 | 18.6 | 59.3 | 15.4 | 22.1 | 308 | |
| Mean | 6.85 | 5.67 | 15.44 | 47.15 | 83.42 | 27.41 | 32.67 | 265.4 | |
| t-value | 58.88 | 115.2 | 210.1 | 238.2 | 207.0 | 170.8 | 290.8 | 83.29 | |
| df | 264 | 264 | 264 | 264 | 264 | 264 | 264 | 264 | |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| R2 | 0.929 | 0.981 | 0.994 | 0.995 | 0.994 | 0.991 | 0.997 | 0.963 | |
| Significant | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| AB | Min | 3.6 | 5.44 | 14.6 | 42.2 | 76.7 | 26.5 | 32 | 230 |
| Max | 11.85 | 6.94 | 18.4 | 57.5 | 85.8 | 28.5 | 34.7 | 476 | |
| Range | 8.25 | 1.5 | 3.8 | 15.3 | 9.1 | 2 | 2.7 | 246 | |
| Mean | 7.43 | 5.92 | 16.39 | 49.28 | 83.2 | 27.70 | 33.31 | 29.75 | |
| t-value | 6 | 33 | 37.40 | 30.31 | 79.67 | 101.6 | 111.4 | 11.06 | |
| df | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | |
| p-value | 0.0004 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| R2 | 0.854 | 0.994 | 0.995 | 0.992 | 0.999 | 0.999 | 0.999 | 0.946 | |
| Significant | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| A | Min | 3.22 | 4.77 | 8.9 | 34.2 | 27.2 | 15.9 | 26 | 110 |
| Max | 16.23 | 7.59 | 18.4 | 57 | 95.9 | 33.7 | 36.3 | 767 | |
| Range | 13.01 | 2.82 | 9.5 | 22.8 | 68.7 | 17.8 | 10.3 | 657 | |
| Mean | 6.63 | 5.62 | 15.44 | 47.07 | 83.34 | 27.68 | 32.80 | 289.0 | |
| t-value | 45.15 | 154.8 | 198.3 | 211.2 | 137.2 | 149.5 | 324.3 | 52.13 | |
| df | 178 | 178 | 178 | 178 | 178 | 178 | 178 | 178 | |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| R2 | 0.920 | 0.993 | 0.996 | 0.996 | 0.991 | 0.992 | 0.998 | 0.939 | |
| Significant | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| B | Min | 3.3 | 4.38 | 12.2 | 38.8 | 71.5 | 21.5 | 30.1 | 205 |
| Max | 13.08 | 7.03 | 17.4 | 54.9 | 93.8 | 31.5 | 35.4 | 527 | |
| Range | 9.78 | 2.65 | 5.2 | 16.1 | 22.3 | 10 | 5.3 | 322 | |
| Mean | 6.95 | 5.70 | 15.65 | 47.85 | 84.28 | 27.64 | 32.76 | 295.6 | |
| t-value | 23.41 | 79.63 | 96.10 | 109.7 | 109.9 | 83.82 | 203.8 | 36.16 | |
| df | 50 | 50 | 50 | 50 | 50 | 50 | 50 | 50 | |
| p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| R2 | 0.916 | 0.992 | 0.995 | 0.996 | 0.996 | 0.993 | 0.999 | 0.963 | |
| Significant | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
Reference values were obtained from Dean,42. In the above table WBC, RBC, HBG, HCT, MCV, MCH, MCHC and PLT stand for White Blood Cell, Red Blood Cell, Hemoglobin, Hematocrit, Mean Corpuscular Volume, Mean Corpuscular Hemoglobin, Mean Corpuscular Hemoglobin Concentration And Platelet count, respectively. While df is degree of freedom.
Table 4: Percentage of Blood Abnormalities among Various Donors.
| Blood group | No. of donors | Abnormalities (%) |
| O | 76 | 28.78 |
| AB | 7 | 99.9 |
| B | 15 | 29.41 |
| A | 55 | 31.6 |
Discussion
In terms of anthropology, forensics, and transfusion medicine, the knowledge of RBC polymorphism and antigen prevalence was essential, and any incompatibility could result in various forms of severity24. Few reports on TTI seroprevalence among blood donors and the prevalence of ABOs and Rh blood in Saudi communities have been reported. However, our study focuses on selective donor screening with TTI and CBC trends along with Rh phenotype polymorphisms.
This analysis reveals how Saudi donors who donated blood to the blood transfusion service centers at Najran city in Saudi Arabia have spread ABO, Rh, and Kell phenotypes. In Tunisian, Riyadh, and Mauritania populations, the pattern of O>A>B>AB identified among their people was recorded10,25,26. Our results are incompatible with the study indicated by Al-Noaemi and Daghriri27. The O blood group in the City of Najran, Saudi Arabia, was large, and the Yam tribe was most prominent. In a blood transfusion, paternity, ethnicity allocation, and certain criminal proceedings, the Kell blood system plays a significant role. It was noticed that in areas like Riyadh, Sundanese, Caucasian, North India, East Asian Blacks, Japan, the prevalence of Kell blood system was 18.2, 5.6, 9, 4, 2, 0.0001, and 1.97%, respectively12,28. In our current research, the distribution of Kell blood system screening among Najran’s populace was found to be 12.3% and suggests its importance for screening during blood transfusion29. In the genetic, demographic analysis, the Kell blood community has a crucial position for the remedy and transfusion practices related to medical-legal problems28. The Rh(D) positive was more in our study than Rh(D)-negative phenotype, and it was also documented in several areas with the ample existence of the Rh-positive phenotype10,26. Rh-positive figures were reported as 95, 100, and 85%, respectively, in Africans, Americans, and Caucasians30. In an emergency, some blood groups are more required than others. Hence the current study could have a substantial effect on the largest blood banks in Najran state.
The average accumulated frequency of TTIs in donor blood of our study was 5.66%. Our data suggested a high percentage of TTIs among male donors than Riyadh city of Saudi, which possessed only 1.002% TTI10. Few other countries also have strong TTI in places like Ethiopia, New Guinea, and Mozambique, with around 18 to 37 percent10,31. The high TTI prevalence in the Najran population can be certified for detecting AHBC and SIC with 5.037 and 2.183 positivity. Sickle cell is a recessive blood disorder condition with a mutation at rs334 in β-globin gene leading to HbS type32. Individuals with HbS homozygous nature will encounter chronic anemia. Thus, the quantification of %HbS among Najran population indicated about 2% presence, this method was easy, rapid and low-cost effective, which improved the management of SIC33. The seropositivity to HBV and HBsAg is also essential, as HBV can spread through transplantation procedures indicating the contagious HBV negative with HBsAg and anti-HBc positive donors, leading to the spread of infection34. Hence, HBc antibodies must also be tested to minimize the likelihood of transfusion infection. The risk of HCV in the United Kingdom was decreased by 95% and HIV by 10% by NAT analysis35. NAT is an innovative and incredibly adaptive procedure, minimizing HBV, HCV, and HIV windows for 10.34, 1.34, and 2.93 days, respectively36. None of the women (n=4) had shown some TTI. As the sample size for women is very less, we are encouraging more women to donate the blood, by providing more knowledge and bringing awareness about the blood donation through workshops and conferences. A minimal prevalence of HIV, HBV, HCV has been identified, and samples displaying seropositive behavior have been removed, and blood donation has not been suggested.
Saudi Arabia has different gene frequencies for each part of the world37. In the current study, Rh phenotyping (D, C, E, c, and e) in over 531 donors revealed their frequencies of 99.9%, 67.98, 25.8, 77.9, and 98.49%, respectively. In Egypt, the prevalence of D>C>e>c > e was seen as 85.5, 70.4, 41.7, and 91.2 and 100%, respectively, in approximately 216 donor subjects12. Swelem et al. 12 had displayed evidence regarding the Rh world-wide phenotypes distribution. The c antigen was more widespread, with 99% in Africans, whereas it is about 43% in East Asia38. In our analysis, the e antigen is more in the studied Saudis, such prevalence of e allele has been reported in North India39. The prevalence of different Rh alleles among various descendants or families suggests the gene flow. Such observation was reported for the Japanese Brazilian population, where C and E alleles were predominantly present24.
Our analysis investigated hematological criteria for blood abnormalities among healthy donors. The age groups between 31-40 have actively participated in blood donation. Data showed further that the average values for hematology variables of donors in Najran City did not vary significantly except for a considerably higher WBC mean recorded by AB donors (p=0.0004). These anomalies in WBC have also been recorded in Nigerians with substantial variations between healthy blood donors40. Subclinical bacteremia may be the cause of increasing overall WBC count41.
Moreover, it is also necessary to follow-up with both MCV and MCH, as any decline in MCV and/or MCH have been identified, the donors are requested to have iron supplements21. In our study, an abnormality of 28.78, 99.9, 29.41, and 31.6% in O, AB, B, and A blood types was observed, and blood donation was not recommended for such donors. Results indicated that few donors had anemia and might be vulnerable to infections. Alternatively, the enumeration and evaluation of hypochromic cells percentage would offer adequate knowledge in decision-making on blood donation and suggest iron supplements’ desirability to donors.
Conclusion
In creating a blood group database, the data collected from this study on the frequency of ABO and Kell blood phenotypic groups helps scan the available donors in emergencies without effort, especially when it is obscure to have any particular blood groups. The allelic patterns in the Rh phenotype would further strengthen the concept of blood donation. Our study also highlights the importance of TTIs and blood abnormalities as they play a significant role in the early detection of anemia or iron depletion. Extensive data and epidemiological studies would improve quality management in any location and play a vital role in avoiding TTI. Innovative research would offer quick detection methods that will attain significant advantages in the future. Given the numerous challenges, there have been essential improvements and cost-effective strategies for enhancing blood transfusions’ safety. This continued dedication and transfusion service improvements would eventually guarantee the next steps and improve the efficiency and potential blood donation studies.
Limitations (Not Compulsory)
Blood donors typically delegate contagious risk, whereas the threat of part processing transmission is sometimes ignored. It is therefore highly technological, involving high-cost problems, dedicated services, supplies, consumables, and technical skills. Our study also had few limitations, where the serum ferritin levels were not assessed. Further, the data on Rh allele frequency distribution was not available for all the donors considered in the study. Lastly, the screening laboratories used for our research purpose was also found to be limited.
Ethical Clearance and Consent to Participate
The study was approved by the Ethics Committee in Najran University (Ethics board approval number: 23-10-3-19). The methods in the study were in accordance with the guidelines of the Declaration of Saudi Arabia. Written informed consent was obtained from all subjects participating in this research.
Acknowledgment
We would like to thank Armed Forces Hospital in Najran city for their technical and financial support and Deanship of Scientific Research at Najran University for their financial support
Conflict of Interest
The authors claim no conflict of interest.
Funding Source (Grant Number)
This work was funded by the Deanship of Scientific Research, Najran University, Najran, under grant No. NU/MID/17/058
References
- Singh A, Srivastava R, Deogharia K, Singh K. Distribution of ABO and Rh types in voluntary Blood donors in Jharkhand area as a study conducted by RIMS, Ranchi. J Fam Med Prim Care 2016;5:631. https://doi.org/10.4103/2249-4863.197319.
CrossRef - Storry JR, Castilho L, Chen Q, Daniels G, Denomme G, Flegel WA, et al. International society of blood transfusion working party on red cell immunogenetics and terminology: report of the Seoul and London meetings. ISBT Sci Ser 2016;11:118–22. https://doi.org/10.1111/voxs.12280.
CrossRef - Mollison PL. The genetic basis of the Rh blood group system. Transfusion 1994;34:539–41. https://doi.org/10.1046/j.1537-2995.1994.34694295073.x.
CrossRef - Mollison PL. The genetic basis of the Rh blood group system. Transfusion 1994;34:539–41. https://doi.org/10.1046/j.1537-2995.1994.34694295073.x.
CrossRef - Watkins WM. The ABO blood group system: historical background. Transfus Med 2001;11:243–65. https://doi.org/10.1046/j.1365-3148.2001.00321.x.
CrossRef - Avent ND, Reid ME. The Rh blood group system: a review. Blood 2000;95:375–87. https://doi.org/10.1182/blood.v95.2.375.
CrossRef - Contreras M, Daniels G. Antigens in Human Blood. Postgrad Haematol 2010:244–67. https://doi.org/10.1002/9781444323160.ch15.
CrossRef - Daniels G. The molecular genetics of blood group polymorphism. Hum Genet. 2009;126(6):729-42.
CrossRef - Daniels G. Human Blood Groups 2013. https://doi.org/10.1002/9781118493595.
CrossRef - Alabdulmonem W, Shariq A, Alqossayir F, AbaAlkhail FM, Al-Musallam AY, Alzaaqi FO, et al. Sero-prevalence ABO and Rh blood groups and their associated Transfusion-Transmissible Infections among Blood Donors in the Central Region of Saudi Arabia. J Infect Public Health 2020;13:299–305. https://doi.org/10.1016/j.jiph.2019.12.004.
CrossRef - Badjie KS, Tauscher CD, van Buskirk CM, et al. Red blood cell phenotype matching for various ethnic groups. Immunohematology 2011;27(1):12‒19.
CrossRef - Swelem O, Goubran F, Younis S, Kamel N. ABO, RH phenotypes and kell blood groups frequencies in an Egyptian population. Hematol Transfus Int J 2018;6. https://doi.org/10.15406/htij.2018.06.00156.
CrossRef - Zhao J, Zhao F, Han W, Xu X, Wang L, Li R, et al. HTLV screening of blood donors using chemiluminescence immunoassay in three major provincial blood centers of China. BMC Infect Dis 2020;20. https://doi.org/10.1186/s12879-020-05282-2.
CrossRef - Asim M, Ali R, Khan LA, Husain SA, Singla R, Kar P. Significance of anti-HBc screening of blood donors and its association with hepatitis B virus infection: Implications for blood transfusion. Ind J Med Res 2010;312-317.
- Keleta YT, Achila OO, Haile AW, Gebrecherkos BH, Tesfaldet DT, Teklu KS, et al. Seroprevalence of transfusion transmitted infections among blood donors in Gash Barka Zonal Blood Transfusion Center, Barentu, Eritrea, 2014 through 2017. BMC Hematol 2019;19. https://doi.org/10.1186/s12878-019-0136-5.
CrossRef - Hans R, Marwaha N. Nucleic acid testing-benefits and constraints. Asian J Transfus Sci 2014;8:2. https://doi.org/10.4103/0973-6247.126679.
CrossRef - Song Y, Bian Y, Petzold M, Ung COL. Prevalence and Trend of Major Transfusion-Transmissible Infections among Blood Donors in Western China, 2005 through 2010. PLoS One 2014;9:e94528. https://doi.org/10.1371/journal.pone.0094528.
CrossRef - Bönig H, Schmidt M, Hourfar K, Schüttrumpf J, Seifried E. Sufficient blood, safe blood: can we have both? BMC Med 2012;10. https://doi.org/10.1186/1741-7015-10-29.
CrossRef - Abdullah SM. The effect of repeated blood donations on the iron status of male Saudi blood donors. Blood Transfus 2011;9(2):167–171.
- Figueiredo MS. Anemia and the blood donor. Rev Bras Hematol Hemoter 2012;34(5): 323-333.
CrossRef - Vuk T, Magnussen K, De Kort W, Folléa G, Liumbruno GM, Schennach H, et al. International forum: an investigation of iron status in blood donors. Blood Transfus 2017;15(1):20–41.
- Alexander HD, Sherlock JP, Bharucha C. Red cell indices as predictors of iron depletion in blood donors. Clin Lab Haematol 2000;22:253–8. https://doi.org/10.1046/j.1365-2257.2000.00323.x.
CrossRef - Shehri O, Alqahtani JM, Khalil KSM, EI Khawanky MM. Increase in haemoglobin A2 window among healthy children in Najran Area, Saudi Arabia. J Appl Hematol 2020;11:84-88.
CrossRef - Flôres MALR, Visentainer JEL, Guelsin GAS, Fracasso A de S, Melo FC de, Hashimoto MN, et al. Rh, Kell, Duffy, Kidd and Diego blood group system polymorphism in Brazilian Japanese descendants. Transfus Apher Sci 2014;50:123–8. https://doi.org/10.1016/j.transci.2013.09.014.
CrossRef - Said N, Ben Ahmed F, Doghri A, Ghazouani E, Layouni S, Gritli N, et al. Polymorphisme ABO dans une population de donneurs de sang tunisiens. Transfus Clin Biol 2003;10:331–4. https://doi.org/10.1016/s1246-7820(03)00100-9.
CrossRef - Hamed CT, Bollahi MA, Abdelhamid I, Med Mahmoud MA, BA B, Ghaber S, et al. Frequencies and ethnic distribution of ABO and Rh(D) blood groups in Mauritania: results of first nationwide study. Int J Immunogenet 2011;39:151–4. https://doi.org/10.1111/j.1744-313x.2011.01064.x.
CrossRef - Al-Noemi MC, Daghriri HA. The significant high prevalence of Blood Group’ O’ in Yam tribe of Najran City, the South province of KSA. Blood Res Reansfus J 2018;2(1):555579.
- Elsayid M. Phenotypic Profile of Kell Blood Group System among Saudi Donors at King Abdulaziz Medical City-Riyadh. J Med Sci Clin Res 2017;05:15654–7. https://doi.org/10.18535/jmscr/v5i1.75.
CrossRef - Daniels G. The molecular genetics of blood group polymorphism. Hum Genet 2009;126:729–42. https://doi.org/10.1007/s00439-009-0738-2.
CrossRef - Moussa S, Al-zaylai F, Alnawmasi MO, Aljarwan MS, Ishammari HA, Alrashedi LM, Aloufi SA. Pattern of distribution of ABO and Rhesus (RH) blood groups in hail province, Saudi Arabia. Int J Medical and Health Research 2018;4(3):166-170.
- Manoharan D, Kaur SPA, Imanina CW. Distribution of ABO blood group and Rhesus factor among students in ASIA Metropolitan University, Malaysia. Int J Biological Med Res 2013;4:2962–2965.
- Stuart MJ, Nagel RL. Sickle-cell disease. Lancet 2004;364:1343–60. https://doi.org/10.1016/s0140-6736(04)17192-4.
CrossRef - Piety NZ, Yang X, Lezzar D, George A, Shevkoplyas SS. A rapid paper-based test for quantifying sickle hemoglobin in blood samples from patients with sickle cell disease. Am J Hematol 2015;90:478–82. https://doi.org/10.1002/ajh.23980.
CrossRef - Dickson RC, Everhart JE, Lake JR, Wei Y, Seaberg EC, Wiesner RH, et al. Transmission of hepatitis B by transplantation of livers from donors positive for antibody to hepatitis B core antigen. The National Institute of Diabetes and Digestive and Kidney Diseases Liver Transplantation Database. Gastroenterology 1997;113:1668–74. https://doi.org/10.1053/gast.1997.v113.pm9352871.
CrossRef - Soldan K, Davison K, Dow B. Estimates of the frequency of HBV, HCV, and HIV infectious donations entering the blood supply in the United Kingdom, 1996 to 2003. Eurosurveillance 2005;10:9–10. https://doi.org/10.2807/esm.10.02.00520-en.
CrossRef - Weusten J, Vermeulen M, van Drimmelen H, Lelie N. Refinement of a viral transmission risk model for blood donations in seroconversion window phase screened by nucleic acid testing in different pool sizes and repeat test algorithms. Transfusion 2010;51:203–15. https://doi.org/10.1111/j.1537-2995.2010.02804.x.
CrossRef - Stevens D. A thalassemia, blood groups and Saudi tribes (letter). Saudi Med J 1992;13:7879. https://doi.org/10.19080/OABTJ.2018.02.555579.
- Jeremiah ZA, Buseri FI. Comparative Analysis of the ABO and Rh CDE Phenotype Frequencies Among Various Ethnic Groups in Port Harcourt, Nigeria. J Med Lab Sci 2009;15. https://doi.org/10.4314/jmls.v15i2.46893.
CrossRef - Thakral B, Saluja K, Sharma RR, Marwaha N. Phenotype frequencies of blood group systems (Rh, Kell, Kidd, Duffy, MNS, P, Lewis, and Lutheran) in north Indian blood donors. Transfus Apher Sci 2010;43:17–22. https://doi.org/10.1016/j.transci.2010.05.006.
CrossRef - Nubila T, Nubila N, Shu E, Okwuosa C, Okofu M, Obiora B, et al. Hematological profile of apparently healthy blood donors at a tertiary hospital in Enugu, south east Nigeria: A pilot study. Niger J Exp Clin Biosci 2014;2:33. https://doi.org/10.4103/2348-0149.135726.
CrossRef - Lugos MD, Okoh JB, Polit UY, Vwamdem NY, Ofojekwu MJN, et al. Some Hematologic Parameters of Blood Donors at the National Blood Transfusion Service (NBTS), Jos, Nigeria. J Blood Disord Transfus 2019;10:1000416 https://doi.org/10.4172/2155-9864.1000416.
CrossRef - Dean L. Blood Groups and Red Cell Antigens [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2005. Table 1, Complete blood count. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2263/table/ch1.T1/







