Bhushan M. Warpe1*, Shweta Joshi-Warpe1 and Sandya V. Pofle2
1Pathology Department, B.K.L. Walawalkar rural medical college (BKLWRMC), Dervan, District-Ratnagiri, State-Maharashtra, India.
2Pathology Department, Indira Gandhi Government Medical College (IGGMC), District-Nagpur, State-Maharashtra, India.
Corresponding Author E-mail: bhushan.warpe@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2193
Abstract
Introduction: Adequacy of thyroid aspirate comprise 5-6 groups of thyroid follicular epithelial cells. Each of the groups consists of ten or more cells on at least two smeared slides. Ultrasonography followed by fine needle cytology (FNC) can be used as a cost-effective, first line tool for diagnosis of thyroid lesions. Aims were: a) To study clinico-radiological, radio-pathological and cyto-histopathological correlation in the diagnosis of variety of thyroid lesions. b) To study the diagnostic parameters for cytological diagnosis of thyroid lesions. Material & Methods: 295 cases of thyroid lesions were studied for a period of two years at a tertiary care hospital in Nagpur, Maharashtra. Clinical data, clinical diagnosis were filled in case proforma. Radiological diagnosis was documented with radiological diagnosis before performing thyroid FNC. The final Bathesda based cytological diagnosis was categorised based on cyto-morphology. Histopathology report of the cases which were operated was correlated with the cytological diagnosis and the radiological diagnosis. The data was entered into Microsoft excel 2016 and analysed. For each correlation; sensitivity, specificity, positive predictive value, diagnostic accuracy was calculated by appropriate formula manually. Results: On comparison of nodularity on clinical examination with USG thyroid examination, the א2-value and p-value was highly significant showing that USG thyroid was better in diagnosing solitary thyroid lesions than clinical examination, after clinico-radiological study. Based on radio-histopathological correlation of cases, the diagnostic parameters were: Sensitivity- 70%, Specificity- 91.3%, Positive predictive value- 70%, Accuracy or Efficacy- 86.5%, False positive rate- 6.74%, False negative rate- 6.74%. Based on cyto-histopathological correlation of cases, the diagnostic parameters were: Sensitivity- 80%, Specificity- 98.44%, Positive predictive value- 94.11%, Accuracy or Efficacy- 94.05%, False positive rate- 01.19%, False negative rate- 4.76%. Conclusion: Diagnostic parameters were thus better on cyto-histopathology correlation than on radio-histopathological correlation. A systematic, sequential, multi-modality approach of clinical examination, radiological diagnosis followed by cytological reporting is the need of the hour. This is important to triage operative neoplastic thyroid lesions from non-neoplastic thyroid cases which are generally not subjected to operative procedures.
Keywords
Fine Needle Aspiration Cytology; Nodule; Thyroid; Ultrasonography
Download this article as:| Copy the following to cite this article: Warpe B. M, Warpe S. J, Pofle S. V. Clinico-Radiological, Radio-Histopathological and Cyto-Histopathological Correlation of Various Thyroid Lesions. Biomed Pharmacol J 2021;14(2). |
| Copy the following to cite this URL: Warpe B. M, Warpe S. J, Pofle S. V. Clinico-Radiological, Radio-Histopathological and Cyto-Histopathological Correlation of Various Thyroid Lesions. Biomed Pharmacol J 2021;14(2). Available from: https://bit.ly/3fqlAvt |
Introduction
The term ‘Thyroid’ originated from the Greek word called ‘Thyreos’ (shield Thomas Wharton of London, UK used this term for the first time in book who renamed it as ‘Glandularis thyroideis’ in 1656. Previous to 1656, thyroid was known as Goitre, Struma and bronchocele. The term ‘Goitre’ is still used till date.1
Thyroid lesions are common and endemic in the developing world due to low iodine intake. Diabetes mellitus followed by thyroid disorders are the two common endocrine disturbances. Goitre with a localized nodule in thyroid or Grave’s and Hashimoto’s disease with diffuse thyroid involvement are commonly seen in clinical practice.2
Benign thyroid lesions do not require excision as they are slow-growing and without complaints. Thyroid malignancies resemble the benign counterparts with various testing modalities like ultrasonography (USG), Serum T4/T3 levels and even sometimes on cytology. Histopathology thus becomes the ‘gold standard’ for definite diagnosis only after effective surgical plan.3
A single palpable thyroid lesion on clinical examination is called solitary thyroid nodule (STN) which show higher tendency for malignancy. The latter range from 5 to 35% of entire STNs.4 Diffuse thyroid conditions are seen in thyroiditis and hyperplasias.5
Thyroid tumours though uncommon are showing increased incidence rate due to earlier diagnosis in India and world-wide. Female cases comprise 0.7% of all cancer cases while males comprise 0.2% depicting female preponderance.6 Inspite of rapid diagnostic improvements, the detection of thyroid tumours still remains an issue due to aggressive tumour status and relatively less incidence compared to other tumours.7,8 It is important to evaluate thyroid disorders in India because about 216000 new cases of thyroid cancers are reported in a year.8
Thyroid cytology-Fine Needle Cytology (FNC) has proven to be a ‘first-line’ tool to study the thyroid lesions because of its low cost and prompt reporting time with high patient compliance.
FNC chiefly, guided FNC helps to segregate thyroid nodules that are operable from the non-operable ones. The latter helps the surgeons to promptly decide on their plan of action.3-
Studies must be done to understand the thyroid disease status in various regions like in our study done in Central India. With that perspective, the following were our aims and objectives: a) To study clinico-radiological, radio-pathological and cyto-histopathological correlation in the diagnosis of various thyroid lesions. b) To assess diagnostic parameters for cytodiagnosis of thyroid lesions.
Material and Methods
This single-centered, prospective, observational study was done in Pathology Department, IGGMC in a tertiary care hospital of Central India from September 2011 to August 2013. A total of 295 thyroid patients who were subjected for cytology were included in study using consecutive sampling technique.
Inclusion Criteria
All thyroid lesions, disregarding their age and sex, referred for cytological study from ENT/Surgery OPDs and those with ward admissions were studied. In each patient detailed clinical history was obtained and thorough clinical examination was done prior to procuring sample for cytological study using case proforma.
Exclusion Criteria
Patients not willing for USG-guided or non-guided FNC of their thyroid lesions even after explaining the importance and consequence of the procedure were excluded.
A detailed clinical history with local examination of thyroid swelling led to a clinical diagnosis by surgeons with special mention of the nodularity status. Supplementary investigations like Thyroid function tests were documented. Radiological (ultrasonography/USG of thyroid) investigation report was documented wherever done with special mention of nodularity status on USG. After USG of thyroid, cytology was done.
Prior to aspiration, size, shape, mobility of thyroid swelling with swallowing, nodularity and clinical complaints were assessed. Fine needle cytology was done by non-aspiration technique (FNC/FNCB) except for cystic lesions which were aspirated (FNAC). FNAC was done using 23 G needle attached to a 10 ml syringe which was further attached to syringe holder. In each case, haematoxylin and eosin (H&E), papanicolaou (PAP) and May-Grunwald-Giemsa (MGG) staining of smeared slides were done. Number of needle passes, nature of aspirate, cytological diagnosis was done based on Bathesda classification for cytodiagnosis of thyroid lesions. As not all lesions are subjected to surgery, only the operated thyroid cases were studied for correlation studies. Nature of operative procedure, gross diagnosis and histopathological diagnosis was documented.
The data was entered into Microsoft excel 2016 and analyzed using MedCalc software program version 14.8.1. Various statisticial formulas were used to calculate diagnostic parameters with 95% confidence interval. On comparison of nodularity on clinical examination with USG thyroid examination, the א2-value and p-value was found. For ultrasonographic-histopathology correlation and cyto-histopathology correlation, diagnostic parameters were found manually.
Results
Based on case details, the following observations were made in the two years study period. Thyroid cytology comprised 5.16% of total FNACs conducted at our institution.
Table 1: Age wise distribution of the 295 thyroid cases
| Age group in years | No. of cases | Percentage |
| 0-10 | 6 | 2.03 |
| 11-20 | 21 | 7.11 |
| 21-30 | 66 | 22.37 |
| 31-40 | 94 | 31.86 |
| 41-50 | 51 | 17.29 |
| 51-60 | 34 | 11.55 |
| 61-70 | 20 | 6.77 |
| 71-80 | 3 | 1.02 |
| Total | 295 | 100 |
| Mean Age | 38.41 ± 14.49 years | |
| SD | 3-75 years | |
Table 1 indicates the overall age of incidence of thyroid lesions in 295 cases. The age of presentation ranged from 3 to 75 years with a mean age of 38.41 ± 14.49 years.
Age of the youngest patient in this series was three years-there were two patients with cytological diagnosis of thyroglossal cyst and a case of colloid cyst respectively. The oldest patient was of 75 years with cytological diagnosis of nodular colloid goitre.
 |
Graph 1: Pie diagram showing sex-wise distribution of cases. |
Graph 1 shows that in the present study, the thyroid lesions were more common in females than males, in the ratio of 6.02:1.
 |
Graph 2: Pie diagram showing site of thyroid lesion. |
Graph 2 shows that bilateral / diffuse involvements of thyroid lesions were most common in 36.27% cases.
Table 2: Clinical symptoms in patients with thyroid lesions
| Complaints | No. of cases | Percentage |
| Swelling in neck | 293 | 98.98 |
| Dysphagia | 53 | 17.97 |
| Palpitation | 51 | 17.29 |
| Pain in swelling | 49 | 16.61 |
| Hoarse voice/ change in voice | 29 | 9.83 |
| Weight loss | 22 | 7.46 |
| Cough with expectoration | 4 | 1.36 |
| Cough without expectoration | 3 | 1.02 |
| Diarrhoea | 2 | 0.68 |
| Headache | 1 | 0.34 |
| Local trauma | 0 | 0.00 |
| Weight gain | 14 | 4.75 |
| No thyroid swelling | 2 | 0.68 |
| Fever | 23 | 7.80 |
| Breathlessness / Dyspnoea | 31 | 10.51 |
| Noisy respiration | 1 | 0.34 |
| Menstrual cycle irregularity | 6 | 2.03 |
| Anorexia | 10 | 3.39 |
| Giddiness | 1 | 0.34 |
| Oedema | 2 | 0.68 |
| Excess sweating | 1 | 0.34 |
| Generalized weakness | 6 | 2.03 |
| Constipation | 2 | 0.68 |
| Oral ulcers | 1 | 0.34 |
| Palpable lymph nodes | 18 | 6.10 |
| Vomiting | 1 | 0.34 |
| Burning micturition | 1 | 0.34 |
| Exophthalmoses | 1 | 0.34 |
| Abdominal mass | 1 | 0.34 |
Sum of percentages of all symptoms is not equal to 100% because multiple complaints were present in a single patient. Table 2 shows that the most common clinical symptom in patients with thyroid lesions was swelling in the neck which was present in 98.98% incidence followed by dysphagia in 53 cases (17.97%). No thyroid swelling was palpated in two cases.
Table 3: Duration of symptoms.
| Duration of symptoms | No. of cases | Percentage |
| ≤1 month | 69 | 23.39 |
| 1-6 months | 88 | 29.83 |
| 6-12 months | 41 | 13.9 |
| > 1 year | 97 | 32.88 |
| Total | 295 | 100 |
| Mean ± SD | 23.95 ± 48.53 months | |
Table 3 shows that out of 295 cases, the maximum number of patients-32.88% presented with duration of symptoms being more than one year. Minimum number of cases-13.9% had the duration of symptoms between 6-12 months.
Table 4: Size of thyroid swelling in 293 cases on palpation
| Size of thyroid swelling-Largest diameter in centimeter (cm) | No. of cases | Percentage |
| ≤ 1cm | 23 | 7.85 |
| ≤ 2 cm | 104 | 35.49 |
| ≤ 3 cm | 89 | 30.38 |
| ≤ 4 cm | 37 | 12.63 |
| ≤ 5 cm | 20 | 6.83 |
| ≤ 6 cm | 9 | 3.07 |
| ≤ 7 cm | 3 | 1.02 |
| ≤ 8 cm | 3 | 1.02 |
| Two thyroid swellings palpated in a case | 5 | 1.71 |
| Total | 293 | 100 |
Thyroid swelling was not palpable in two cases on local examination out of 295 cases. The size of smallest thyroid swelling was 0.9 x 0.8 cm and the size of the largest swelling- 8 x 6 cm.
Mobility, tenderness of thyroid swelling
Out of total 293 palpable thyroid swellings cases, 98.98% were mobile on palpation. Only three thyroid cases were fixed on palpation which turned out to be malignant.
293 thyroid swellings moved up with deglutition. Nine thyroid swellings moved up with both deglutition and protrusion of tongue. Majority of the thyroid cases-260/283 cases (88.74%) were non-tender on clinical examination of the swelling while 33/283 cases (11.26%) were associated with tenderness.
 |
Graph 3: Bar diagram showing consistency of thyroid swelling. |
From Graph 3, it is observed that the maximum number of thyroid lesions were firm in consistency-55.56%, followed by thyroid lesions of mixed consistency. Hard thyroid lesions were few on palpation.
Table 5: Thyroid function tests in 221 cases.
| Functional thyroid status | No. of cases | Percentage |
| Euthyroid | 188 | 85.07 |
| Hyperthyroid | 21 | 9.5 |
| Hypothyroid | 12 | 5.43 |
| Total | 221 | 100 |
Table 5 shows that out of total 295 cases, TFT was done in 221 (74.92%) patients and not done in 74 cases. Out of 221 cases, 85.07% were euthyroid. Among the thyroid derangements, 21 cases (9.5%) were hyperthyroid and 12 cases (5.43%) were hypothyroid.
Table 6: Distribution of cases on clinical diagnosis
| Cases | On Clinical examination | |
| No. of cases | % | |
| Solitary | 248 | 84.64 |
| Multi-nodular | 45 | 15.36 |
| Total | 293 | 100 |
In two cases referred for cytology, thyroid swelling was not palpable and could only be detected on USG examination. Table 6 shows that the most common type of presentation was solitary thyroid nodule-84.64% patients. 15.26% patients had multinodular goitre.
Table 7: USG diagnosis of 295 cases
| USG diagnosis | No. of cases | Percentage |
| Thyroglossal cyst | 9 | 3.05 |
| Thyroiditis | 23 | 9.83 |
| Solitary-Colloid goitre | 52 | 26.78 |
| Multi-nodular goiter (MNG) | 166 | 56.27 |
| Neoplasm | 11 | 3.73 |
| Hyperplastic thyroid nodule | 1 | 0.34 |
| Total | 295 | 100 |
USG thyroid was done in all 295 cases. Table 7 shows that out of 295 cases, the maximum number of thyroid cases on USG were diagnosed as MNG accounting for 56.27% of cases. Colloid goitre in a solitary nodule was diagnosed in 26.78% cases on USG thyroid.
Table 8: Comparison of nodularity on clinical examination with USG thyroid examination.
| Cases | On clinical examination | On USG neck examination | ||
| No. of cases | % | No. of cases | % | |
| Single swelling | 248 | 84.64 | 129 | 43.73 |
| Multiple swellings | 45 | 15.36 | 166 | 56.27 |
| Total | 293 | 100 | 295 | 100 |
| א2-value | 36.71 | |||
| p-value | P<0.0001, Significant | |||
In our study in 293 out of 295 thyroid cases the swellings were palpable while in remaining two cases, only USG examination detected the thyroid swelling. 84.64% of thyroid cases were solitary on palpation but only 43.73% proved to be solitary on USG examination. On comparison of nodularity on clinical examination with USG thyroid examination, the א2-value and p-value was highly significant showing that USG thyroid was better in diagnosing STN cases than clinical examination.
Table 9: Frequency of needle passes.
| No. of passes | No. of cases | Percentage (%) |
| One | 192 | 65.08 |
| Two | 90 | 30.51 |
| Three | 12 | 4.07 |
| Four | 1 | 0.34 |
| Total | 295 | 100 |
Table 9 shows that 65.08% of thyroid cases yielded adequate cellularity on FNAC/FNC done on single first prick of the swelling.
Table 10: Sampling technique used.
| Technique | Cases | Guided sampling | Unguided
sampling |
|||
| No. | % | No. | % | No. | % | |
| Fine Needle Capillary Biopsy (Non-aspiration)/ FNC/ FNCB | 233 | 78.98 | 61 | 59.80 | 125 | 64.77 |
| Fine Needle Aspiration Cytology aspiration/ FNAC | 62 | 21.02 | 41 | 40.20 | 68 | 35.23 |
| Total cases | 295 | 100 | 102 | 100 | 193 | 100 |
Table 10 shows that Fine Needle Capillary Biopsy (FNC/FNCB) comprised 78.98% of cases, while Fine Needle Aspiration Cytology (FNAC) comprised 21.02% of thyroid cases.
Total 102 out of 295 cases were subjected to USG-guided sampling technique. Out of these, 59.80% cases were done by FNC and rest 40.20% cases were done by FNAC technique.
Total 193 out of 295 cases were subjected to Unguided or Free-hand sampling technique. Out of these, 64.77% cases were done by FNC and rest 35.23% cases were done by FNAC technique.
 |
Graph 4: Bar diagram showing aspiration material obtained. |
Graph 4 shows that out of 295 cases, thyroid aspirate material obtained most of the times was hemorrhagic -144 cases (48.81%), followed by blood mixed colloid 117 cases (39.66%). Least number of cases-34 in number (11.53%) was frank colloid in nature.
 |
Graph 5: Bar diagram showing diagnostic success rate on cytology. |
Graph 5 shows that satisfactory cytological smears were obtained in 263 (89.15%) cases. Out of total 295 cases, the thyroid aspirates were inadequate for interpretation in 32 (10.85%) cases.
Table 11: Routine cytological diagnosis of 263 cases
| Routine cytological reporting | No. of cases | Percentage (%) |
| Colloid cyst / Cystic colloid nodule | 38 | 14.46 |
| Colloid goitre | 172 | 65.40 |
| Hyperplastic nodule / Adenomatoid goitre | 6 | 2.28 |
| Thyroglossal cyst | 8 | 3.04 |
| Infected cystic lesion | 1 | 0.38 |
| Granulomatous thyroiditis | 4 | 1.52 |
| Hashimoto’s thyroidits | 4 | 1.52 |
| Lymphocytic thyroidits | 9 | 3.42 |
| Intra-thyroid reactive lymph node | 1 | 0.38 |
| Follicular neoplasm | 6 | 2.28 |
| Papillary Carcinoma | 9 | 3.42 |
| Anaplastic Carcinoma | 2 | 0.76 |
| Medullary Carcinoma | 2 | 0.76 |
| Insular carcinoma | 1 | 0.38 |
Table 11 shows that more than half the number of thyroid FNACs in our study was diagnosed as colloid goitre (65.4% cases).
Diagnostic categorization based on Bathesda classification was applied to all 295 cases as follows:
Table 12: Diagnostic categorization of 295 thyroid FNACs based on Bathesda classification
| Categories | Total no. of cases | % |
| Group 1 : Benign | 239 | 81.01 |
| Group 2 : Atypia with Undetermined Significance (AUS) | 2 | 0.68 |
| Group 3 : Suspicious for Neoplasm | 6 | 2.03 |
| Group 4 : Suspicious for malignancy | 2 | 0.68 |
| Group 5 : Malignant | 14 | 4.75 |
| Group 6 : Inadequate/Non-diagnostic | 32 | 10.85 |
| Total | 295 | 100 |
Table 12 shows that 81.01% of 295 thyroid FNACs was cytologically benign and colloid goitre comprised 65.4% (Table 11). The two cases under Atypia of undetermined significance (AUS) were Follicular neoplasm / Multinodular goitre and Follicular neoplasm / Adenomatoid goitre.
There were six cases under the neoplasm category-all six cases cytologically diagnosed as follicular neoplasm.
Suspicious for malignancy category included two cases-Hyalinizing Trabecular Adenoma/Columnar Variant of Papillary Carcinoma and Medullary carcinoma / Oncocytic neoplasm.
Under the malignant category, there were fourteen cytologically diagnosed cases-nine cases as Papillary carcinoma, two cases each of Anaplastic carcinoma and Medullary carcinoma and a single case of Insular carcinoma respectively. Also, in the Inadequate / Non-diagnostic category there were 32 cases comprising 10.85% of cases.
Discussion
Table 13 shows that there is wide age distribution with respect to various thyroid lesions in various studies. In our study, 38.41 ± 14.49 years was the mean age of patients with thyroid lesions.
In benign category youngest case was 3 years of age, whereas oldest patient was 75 years of age. In the malignant category, youngest patient was 30 years of age, whereas oldest patient was of 70 years. In our study maximum number of cases were seen in the third decade of life (31.86%) followed by 21-30 years (22.37%).
Table 13: Age groups encountered in different studies
| Author(s) | Year | No. of Cases | Age Range
(yrs) |
Mean Age
(yrs) |
| Singh P et al 9 | 2000 | 108 | 12-80 | 47 |
| El Hag IA et al 10 | 2003 | 303 | 5-90 | 36 |
| Sangalli G et al 11 | 2006 | 5469 | 6-91 | 47.2 |
| Aravinthan et al 12 | 2007 | 110 | 26-59 | 46 |
| Handa U et al 13 | 2008 | 434 | 5-80 | 37.69 |
| Mandal S et al 14 | 2011 | 120 | 15-71 | – |
| Chittawadagi BB et al 15 | 2018 | 100 | 15-80 | 38.62 |
| Present study | 2020 | 295 | 3-75 | 38.41 |
Female:Male ratio was 6.02:1 in this study. It was comparable with most of the other studies. It was closest to Handa U et al (2008)13 in which the Female: Male ratio was 6.35:1. The thyroid diseases affect females more commonly than males. 16,17 In our study 42 males (14.24%) with thyroid swellings were referred for cytological study during the two years study period. Out of the total 42 male cases, five cases were neoplastic thyroid lesions, 34 were non-neoplastic lesions and three cases were unsatisfactory on cytology.
Liechty RD et al (1965)18 inferred that thyroid nodules affect right lobe more commonly than the left thyroid lobe. The present study like Kapilla K et al (1995)19 shows that bilateral/ diffuse involvement of thyroid lesions were observed maximum in 36.27% cases, closely followed by the right lobe of thyroid which was involved in 32.54% cases and left lobe involvement in 21.02% thyroid cases. The involvement of isthmus was observed in least number of cases in the present study, 10 cases i.e. 10.17%.
In 1993, Ananthakrishnan N, et al4 studied clinicopathological profile of 503 patients STN where apart from swelling of thyroid gland, pain was the commonest symptom. Handa U et al (2008)13 stated in their study that the diffuse or nodular thyroid swelling was the main presenting symptom. Pain in the swelling with difficulty in swallowing (dysphagia), hoarse voice and cough were the other lesser found complaints. Thus thyroid swelling in present study is in accordance to many mentioned studies in literature.
The duration of thyroid swelling varies due to low literacy, poverty, ignorance, mild complaints, from study to study. Maximum number of patients (32.88%) had thyroid lesions with symptoms more than one year in our study which correlates with study by Handa U et al (2008)13.
Size of thyroid swelling
The lower size of the thyroid swelling mostly favours benign pathology. In our study, the majority of the patients-216 cases (73.72%) had the size of the thyroid swelling between 1 to 3 cm. Maximum size of the swelling was ≤ 8 cm diameter in three of our cases. Two separate thyroid swellings were palpated in five of our cases.
Walker J et al (1985)20 observed that for a thyroid nodule to be detected by palpation it must be atleast 1 cm in diameter, while USG detects nodules as small as 3 mm in diameter.
Aravinthan T et al (2007)12 suggested that non-palpable thyroid nodules less than 1 cm diameter are generally not malignant. Jayaram G and Orell SR et al (2012)21 stated that nodules less than 1 cm in diameter are generally detected during USG thyroid examination rather than on clinical examination. Without strong suspicion or family history, such tiny thyroid nodules detected incidentally on USG thyroid should not be subjected for cytopathology opinion.
Mobility of thyroid swelling
The reason for the upward mobility of the neck swellings like thyroid lumps with deglutition is due to relation of neck swellings to the trachea. If a swelling is fixed to the trachea then it will move when the trachea moves. The process of swallowing elevates the trachea. One must observe the neck lump as the patient swallows. 22 In 98.98% of our thyroid cases, the thyroid lesion moved with deglutition.
Relation of midline neck swellings to the hyoid cartilage is responsible for swellings moving up with both protrusion of tongue and deglutition. The hyoid cartilage ascends when the tongue is protruded and due to fixity of the swelling to the hyoid bone, it tends to move the swelling upwards with tongue protrusion. The midline neck swellings usually present as a painless, rounded cystic lump, moves on swallowing or protruding the tongue. It can occur anywhere along the thyroglossal tract i.e. from the foramen caecum to the thyroid isthmus, but is most commonly above the hyoid bone. The cyst is freely mobile and the majority transilluminate. Occasionally they become infected and present as a thyroglossal cyst.22 In nine of our 295 cases the swellings moved up with both protrusion of tongue and deglutition which was diagnosed on cytology as thyroglossal cyst.
Tenderness of thyroid swelling
Pain and tenderness of thyroid swelling is mostly associated with benign etiology.17 Granulomatous or viral (de Quervain) thyroiditis is the most common cause of thyroid pain.16 In our study, the majority of the swellings-260/293 (88.74%) cases were not associated with tenderness on clinical palpation of the thyroid lesions. This finding is in accordance to study by Ananthakrishnan N et al (1993),4 which had 10% thyroid cases with tenderness while 90% cases were non-tender thyroid lesions. Thyroid swelling was associated with tenderness in 33 of the 293 clinically palpable lumps (11.26% cases). This included 24 cases of colloid goitre, four cases of thyroiditis, three cases of malignancy and a case each of thyroiditis and hyperplastic nodule in our study.
Consistency of thyroid swelling
Consistency of thyroid swelling17 The consistency of normal thyroid is considered as rubbery. A patient with Grave’s disease has a thyroid that feels softer than normal, often described as spongy and malleable. A spectrum of increased firmness of the thyroid tissue has been described from the Grave’s disease, to colloid goitre and early Hashimoto’s thyroiditis. Adenomatous and multi-nodular goitres are firm in consistency. Also, the gland is firm in late Hashimoto’s thyroiditis due to extensive fibrosis. Infiltrating primary thyroid malignancies, thyroid lymphomas and fibrotic gland affected by Riedel’s thyroiditis are stony hard or having woody consistency. In our study, the majority of thyroid lesions were firm on palpation (55.56%), followed by those with mixed consistency (32.42%).
Our TFT findings correlated with Godinho-Matos L et al (1992).23 Four out of 21 cases had clinical signs and symptoms of clinical hyperthyroidism while rest of our cases were subclinical hyperthyroid cases. Hyperthyroidism is diagnosed based upon clinical signs/symptoms, supplemented by serum free T3/T4/TSH levels and radioactive iodine uptake tests in few.23
The pre-operative anaesthetic evaluation includes TFT. All patients must be euthyroid before surgery to avoid critical medical emergency of thyroid storm. In this condition the patients with underlying Grave’s disease have acute elevation of catecholamines due to surgery resulting in fever, tachycardia and fatal cardiac arrhythmias.16,17
Importance of performing Thyroid function tests (TFTs) before FNAC
Importance of performing Thyroid function tests (TFTs) before FNAC:17,24 TFT and FNAC are both non-invasive investigations that help the clinicians decide on medical line of management or undertake surgical intervention. Routine thyroid palpation or FNAC may result in increased levels of measured thyroid hormones and thyroglobulin within two hours of examination, while TSH levels are unaffected. Also TFT helps the pathologists before performing cytological procedure to rule out certain certain conditions like Grave’s disease, Hashimoto’s thyroiditis, and toxic adenoma, toxic multi-nodular goitre which are associated with deranged TFTs. This confirms the importance of performing TFTs before performing the FNAC procedure. We followed this same protocol in each of our 221 cases in which TFT was done.
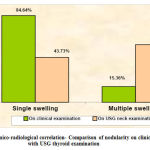 |
Graph 6: Clinico-radiological correlation- Comparison of nodularity on clinical palpation with USG thyroid examination. |
In our study on clinical examination 84.64% of thyroid cases which were STNs on palpation were reduced by nearly half to 43.73% on USG evaluation (Graph 6) USG examination of thyroid is more sensitive, accurate diagnostic procedure to find about thyroid nodularity.17,24 The risk of thyroid cancer is more seen with STNs than MNG.16 Simeone JF et al (1982) 25 stated that the USG based detection of more than one thyroid nodule reduces the malignancy potential to 1-6%. Walker J et al (1985)20 have shown that the prevalence of multi-nodularity in clinically detected STNs is 20% to 40%.
Number of needle passes and nature of aspirate: Maximum number of patients yielded good cellularity on FNAC/FNC done once (65.08% cases). Least number of cases-11.12% cases were frank colloid in nature mainly seen in cystic thyroid lesions. Out of 295 thyroid aspirates, repeat aspiration due to sample inadequacy, poor preparation, cystic lesions, suspected neoplastic lesions or bigger lumps was done in 34.92% cases (n=103). This discrepancy in our study can be attributed to inexperienced cytopathologists with rotational posting performing the sampling procedure. In our study, the number of needle passes was restricted to less than four. In cases of inadequate smears by first sampling, repeat sampling was advised each time following a different needle track which reduced chances of blood aspirated from previous trauma. The FNAC technique was used early for cystic thyroid lesions in our study and later residual lesion was sampled.
The aspirate obtained most of the times from thyroid sampling in our study was haemorrhagic (48.81%), followed by blood mixed colloid (39.66%), as thyroid is a highly vascular organ.46 Jayaram G and Orell SR et al (2005)46 suggested that the average number of needle passes recommended for adequate sampling of thyroid lumps is two to five. As thyroid gland is a highly vascular organ, with each impending trauma the chances of aspirating haemorrhagic fluid rises each time, so they advised to keep the number of aspirates to minimum. Mandal S et al (2011)43 performed repeat aspiration in 5.5% (n=6) wherever the first thyroid aspirate was inadequate in their study of 120 cases. Mondal SK et al (2013)106 in their study on 1020 cases conducted repeat FNAC in 6.76% (n=69) with initially non-diagnostic aspirates.
Adequacy of aspirated thyroid material:21,26 All thyroid FNAs must be technically adequate, with well-preserved, well-prepared thyroid follicular epithelial cells for interpretation. Aspirates that contain only cyst fluid, histiocytes, and erythrocytes are inadequate. Usually, 1-4 thyroid aspirates are suffice in single nodular lesion of diameter less than 3 cm whereas 4-8 aspirates are required for thyroid lesions more than 3 cm, which help reduce false negative rate.
Hamburger JI et al (1989)27 suggested that in the dominant nodule, evidence of six follicular epithelial clusters on two separate smears constitute a minimum FNC material for sample adequacy. Using these criteria, they observed that 77% of satisfactory aspirates were achieved with 2-4 needle passes, whereas 23% required 6-8 passes. If lesser amounts of material were accepted as satisfactory, higher rates of false negative diagnoses occurred in their study. Other authors rely on similar criteria (5-6 groups of follicular cells with more than 10 cells/group).
Jayaram G and Orell SR (2012)21 suggested that abundant clean colloid without altered blood or debris generally indicates a benign STN. Also more than four needle passes were seen to cause local tissue injury with lower patient compliance.
Sanchez MA and Stahl RE (2006)26 suggest that the number of follicular epithelial cell criteria is unrealistic as, for example, pure colloid may be consistent with the diagnosis of benign colloid goitre and a pure population of macrophages may be diagnostic of a thyroid cyst or pseudocyst in a patient with past history of haemorrhage. In neither of the examples is the presence of certain number of epithelial cells required for diagnosis. They concluded that the skill of the person performing thyroid FNB is of more paramount importance and also the type of thyroid lesion (cystic or solid).
Hall TL et al (1989)28 suggested that on average, 80% of aspirates are satisfactory and this figure rises to 90% on repeat aspiration. Those with the widest experience achieve over 97% of satisfactory samples.
Thus, adequate or satisfactory thyroid smears are defined as -the smears having minimum of six clusters or groups of thyroid follicular cells with ten cells per cluster, on atleast two thyroid FNB procedures.
Table 14: Performance of Aspiration (FNAC) and Non-aspiration cytology (FNC) in 295 cases
| Sampling technique used | No. of cases | USG guided | Unguided | Inadequate | |||
| Guided | Un-guided | Total | % | ||||
| FNC | 233 | 61 | 125 | 16 | 6 | 22 | 9.44 |
| FNAC | 62 | 41 | 68 | 8 | 2 | 10 | 16.13 |
| Total | 295 | 102 | 193 | 24 | 8 | 32 | 10.85 |
Thyroid gland is a highly vascular organ. Table 14 shows that out of 295 total cases, non-aspiration technique was used for most of the cases (n=233) in our study while aspiration technique yielded adequate cellularity for interpretation in 62 cases. Out of 295 cases, unguided cytological sampling was done in 193 of our cases while USG-guided cytological sampling was done in 102 cases.
Overall 32 aspirates were unsuitable for cytogical interpretation. Out of these 32 inadequate aspirates, 22 cases (9.44%) were unsuitable for cytodiagnosis by FNC as compared to ten cases (16.13%) by FNAC technique. This shows that the aspirate inadequacy rate was lesser by FNC technique as compared to FNAC technique, which was a finding similar to studies by Santos JEC et al (1988)29 and Khan S et al (2004).30
With the utilization of both FNAC and FNC techniques together, the overall sample inadequacy rate was reduced to 10.85%. This finding correlated to the study by Maurya AK et al (2010).31
Mishra M et al (2001)32 conducted a study of 100 different lesions from lymph nodes, breast, thyroid, soft tissue lesions and liver mass. Like our study, they concluded that FNC yields diagnostically superior FNC aspirate in 68% thyroid cases with a highly significant p-value of <0.01 as against 42% by the conventional FNAC procedure.
Guided FNAC: Ultrasound examination (USG) of thyroid gland and the neck region provides the information on structure of parenchyma of thyroid gland, on its relationship to its surrounding and on regional lymphnodes.33 Though the method of thyroid gland ultrasound developed greatly in the recent years, it is not reliable enough by itself for the diagnosis of malignant focal lesions.33 Ultrasound was primarily used to distinguish between cystic and solid thyroid lesions.34
USG-thyroid followed by FNC has been recommended in thyroid nodules rather than one of the procedures been used alone. USG-thyroid helps passage of needle for fine needle aspiration within a thyroid nodule and thus improves the diagnostic quality.
Ultrasound guided FNAC is preferred to and appears to be more sensitive than palpation-guided non-aspiration sampling technique for indistinctly palpable thyroid nodules, those that are predominately cystic (>25%), small nodules <1 cm, and when a prior FNA was non-diagnostic. Ultrasound guidance for FNC results in high accuracy and safety.35,36 The rate of inadequacy smears is reduced significantly by usage of UGG-guided FNAC when compared to routine/ free hand/ unguided FNAC.37
Amirkachi M et al (2001)38 studied that selection of cases with prior ultrasonography will yield a lower number of inadequate samples.
Table 15: Comparison of unsatisfactory smears-USG guided vs Unguided sampling
| Studies | Year | FNAC | Unsatisfactory smears | ||
| Unguided / Guided | Total sampling | No. | % | ||
| Rosen IB et al33 | 1993 | USG | 59 | 19 | 32 |
| Hatada T et al 34 | 1998 | USG | 72 | 12 | 17 |
| Unguided | 94 | 28 | 30 | ||
| Mehrotra P et al 39 | 2005 | USG | 121 | 19 | 15.6 |
| Unguided | 141 | 66 | 46.8 | ||
| Cai XJ et al 37 | 2006 | USG | 373 | 24 | 6.4 |
| Unguided | 61 | 8 | 13.1 | ||
| Present study | 2020 | USG | 32 | 8 | 7.84 |
| Unguided | 32 | 24 | 12.44 | ||
Table 15 shows that total 32 aspirates (10.85%) were inadequate for cytologic interpretation. Among them the cytological sampling done by US-guided FNAC were unsatisfactory in eight cases whereas sampling done by unguided / free hand FNAC technique were unsatisfactory in 24 cases with smear inadequacy rate being 7.84% and 12.44% respectively.
This finding was comparable to study by Cai XJ et al (2006).37 The smear inadequacy rate was lower in both unguided and guided FNAC in our study as compared to studies by Rosen IB et al (1993)33, Hatada T et al (1998)34 and Mehrotra P et al (2005).39 The presence of colloid shows that it’s a thyroid aspirate however, without cells it is not helpful in diagnosis.40
FNAC of thyroid swellings in our study yielded satisfactory smears in 89.15% of cases which is comparable to most of the above mentioned studies and closest to Guhamallick M et al (2008).41 In the present study the cytological smears were inadequate for interpretation in 10.85% cases which is closest to Santos JEC et al (1988).29 Amrikachi M et al (2001)38 through their study concluded that the experience of the aspirator and the criteria used to define a satisfactory thyroid aspirate are the most important factors which influence the accuracy of aspirations. In our study the majority (n=263) of the aspirations done were satisfactory for cytological examination with satisfactory: unsatisfactory ratio of 8.2:1. In other studies the ratio ranged from 4.5:1 to 84:1. Our satisfactory to unsatisfactory ratio of 8.2:1, was near to the one obtained by Santos JEC al (1988).29
Out of 295 cases over two years, 89 cases underwent surgery. Thus, USG and histopathological correlation was obtained in 89 of those cases.
Table 16: Comparison of USG diagnosis with histopathological diagnosis in 89 cases
| USG Diagnosis | Cytological diagnosis (Bathesda based) | Correlation | |||
| Pre-operative diagnosis | No. of cases | Category | No. of cases | No. | % |
|
Multi-nodular goitre (MNG) |
38 | Benign | 29 | 26 | 89.66 |
| AUS | 2 | 0 | 0 | ||
| Neoplasm | 3 | 2 | 66.67 | ||
| Suspicious of malignancy | 1 | 1 | 100 | ||
| Malignant | 3 | 2 | 66.67 | ||
| Non-diagnostic | 0 | 0 | 0 | ||
|
STN |
15 | Benign | 6 | 6 | 100 |
| AUS | 0 | 0 | 0 | ||
| Neoplasm | 6 | 5 | 83.33 | ||
| Suspicious of malignancy | 1 | 1 | 100 | ||
| Malignant | 2 | 1 | 100 | ||
| Non-diagnostic | 0 | 0 | 0 | ||
| Simple colloid goitre | 12 | Benign | 12 | 12 | 100 |
| AUS | 0 | 0 | 0 | ||
| Neoplasm | 0 | 0 | 0 | ||
| Suspicious of malignancy | 0 | 0 | 0 | ||
| Malignant | 0 | 0 | 0 | ||
| Non-diagnostic | 0 | 0 | 0 | ||
| Thyroiditis | 5 | Benign | 5 | 5 | 100 |
| Thyroglossal cyst | 11 | Benign | 11 | 11 | 100 |
| Benign hyperplastic nodule | 1 | Benign | 1 | 0 | 0 |
| Thyroid Malignancy | 6 | Malignant | 6 | 5 | 83.33 |
| Benign | 0 | 0 | 0 | ||
| USG not done | 1 | Benign | – | – | – |
| Total | 89 | – | 89 | 77 | – |
Table 16 shows that maximum cases in our study were diagnosed as MNG (n=38) on USG neck in the 89 cases wherein USG vs Histopathology correlation was available. Neoplastic lesions were seen more in STN cases than MNG cases. This finding is in accordance to Maitra A (2010).16
The overall correlation of USG vs Histopathology diagnoses was seen in 77 out of 89 cases (86.52%). The correlation of USG diagnosis with Histopathology is given below:
MNG- 31 out of 38 cases (81.58%), STN-13 out of 15 cases (86.67%), Simple colloid goitre-12 out of 12 cases (100%), Thyroiditis-5 out of 5 cases (100%), Thyroglossal cyst-11 out of 11 cases (100%), Benign hyperplastic nodule- 0 out of 1 case (0%), Thyroid malignancy-5 out of 6 cases (83.33%).
Table 17: Diagnostic parameters on the basis of USG and Histopathology study in 89 cases
|
USG |
Histopathology | |||
| Benign | Malignant | Total USG | ||
| Benign | 63 (TN) | 6 (FN) | 69 | |
| Malignant | 6 (FP) | 14 (TP) | 20 | |
| Total Histopathology | 69 | 20 | 89 | |
Table 17 shows that malignancy was indicated on USG and Histopathology in 20 of the 89 cases wherein USG vs Histopathology correlation was available. The correctly correlated malignant cases were 14 in number (TP-True positive). The wrongly diagnosed benign cases on USG which turned out malignant on histopathology (FN-False negative) were six in number.
The cases diagnosed as benign on USG were 69 out of the correlated 89 cases. The cases correctly correlated as benign (TN-True Negative) on histopathology were 63 in number while wrongly interpreted cases as malignant lesions on USG neck but found to be benign (FP-False positive) on such correlation were six in number.
Diagnostic parameters obtained after using USG to detect thyroid malignancy:
Sensitivity- 70%, Specificity- 91.3%, Positive predictive value (PPV)- 70%, Accuracy- 86.52%, False positive rate- 6.74%, False negative rate- 6.74%
Table 18: Comparison of diagnostic parameters on the basis of USG and Histopathology study.
| Series | Sensitivity | Specificity |
| Jones AJ et al (1990) 42 | 75% | 61% |
| Watters DA et al (1998) 43 | 74% | 83% |
| Cai XJ et al (2006) 37 | 80.5% | 97.8% |
| Present study (2013) | 70% | 91.3% |
Table 18 shows that the sensitivity and specificity of USG in detecting malignancy to be 70% and 91.3% respectively which is comparable to the other studies. Watters DA et al (1998)43 emphasized that USG-thyroid be used as a complementary guide rather than an alternative investigative measure to FNAC in management of STNs.
Table 19: Comparison of FNAC diagnoses based on Bathesda classification.
| Diagnostic category | Yassa L et al (2007)44 | Yang J et al (2007)45 | Nayar R and Ivanovic M et al (2009)46 |
Jo VY et al (2010)47 | Mondal SK et al (2013)48 |
Present study (2020) |
| Non-diagnostic | 7 | 10.4 | 5 | 18.6 | 1.2 | 10.85 |
| Benign | 66 | 64.6 | 64 | 59 | 87.5 | 81.01 |
| AUS | 4 | 3.2 | 18 | 3.4 | 1 | 0.68 |
| Neoplasm | 9 | 11.6 | 6 | 9.7 | 4.2 | 2.03 |
| Suspicious for malignancy | 9 | 2.6 | 2 | 2.3 | 1.4 | 0.68 |
| Malignant | 5 | 7.6 | 5 | 7 | 4.7 | 4.75 |
From Table 19, it is clear that our results are comparable to most of the studies and is closest to Mondal SK et al (2013).48 Out of 295 thyroid FNACs over two years, 89 cases underwent surgery.
Table 20: Comparison of malignancy risk on histopathological correlation for each Bathesda category
| Diagnostic category | Yassa L et al (2007) 44 | Yang J
et al (2007) 45 |
Nayar and Ivanovic et al (2009) 46 |
Jo VY et al (2010) 47 | Mondal SK et al (2013)48 | Present study (2020) |
| Benign | 0.3 | 0.7 | 2 | 11 | 4.5 | 0 |
| AUS | 24 | 19.2 | 6 | 17 | 20 | 0 |
| Neoplasm | 28 | 32.2 | 14 | 25.4 | 30.6 | 83.33 |
| Suspicious for malignancy | 60 | 64.8 | 53 | 70 | 75 | 100 |
| Malignant | 97 | 98.4 | 97 | 98.1 | 97.8 | 92.86 |
| Non-diagnostic | 10 | 10.7 | 9 | 8.9 | 0 | 0 |
Table 20 shows that the results of our study are comparable to the others. It shows that the result of malignancy risk for Benign category is 0% and is closest to Yassa L et al (2007)44. Jo VY et al. (2010)47 reported higher risk of malignancy than all the other studies.
Secondly, the malignancy risk for AUS category is 0%, which is lower than other studies because we had only two cases in this category and both were benign on histopathology.
Thirdly, the malignancy risk for Neoplasm category is 83.33% in our study, which is higher than the other studies because five cases out of total six cases in this category turned out malignant on histopathology. The risk of malignancy in the category of ‘suspicious for malignancy’ is 100% and higher than the other studies because in our study, only two cases were seen in this category and both were malignant on histopathology.
The malignancy risk for malignant category in our study is 92.86% which is slightly lower than the other studies. The result of malignancy risk for Non-diagnostic category is 0% and is similar to Mondal SK et al (2013)48 but lower than the other studies.
This study inferred that the Bathesda system is a very useful method for a standardized system of reporting of thyroid cytopathology and improving the communication between clinicians and cytopathologists that lead to more consistent management approaches. 106
Table 21: Comparison of routine FNAC with histopathological diagnosis for diagnostic parameters in 84 cases
|
FNAC |
Histopathology | |||
| Benign | Malignant | Total Cytology | ||
| Benign | 63 (TN) | 4 (FN) | 67 | |
| Malignant | 1 (FP) | 16 (TP) | 17 | |
| Total Histopathology | 64 | 20 | 84 | |
Total 89 cases out of 295 cases underwent surgery. Pre-operative routine cytodiagnosis due to inadequacy was not possible in five of the 89 cases. So in our study cyto-histopathology correlation was possible in 84 cases as in Table 21.
On such correlation the correctly correlated malignant cases were 16 in number (TP-True positive). The wrongly diagnosed benign cases on routine FNAC which turned out malignant on histopathology (FP-False negative) were four in number. All four cases were cytologically diagnosed as follicular neoplasm and all were found to be follicular carcinoma on histopathologic correlation which led to high false negative rate.
The cases diagnosed as benign lesions on FNAC were 64 out of the correlated 84 cases. The cases correctly correlated as benign (TN-True Negative) were 63 in number. There was a single case wrongly interpreted as malignant on FNAC but found to be benign on such correlation. This discrepant false positive case was cytologically diagnosed as papillary carcinoma and as nodular colloid goitre on histopathology respectively.
Diagnostic parameters of FNAC with Histopathological correlation
Sensitivity-80%, Specificity- 98.44%, Positive predictive value (PPV)- 94.11%, Accuracy- 94.05%, False positive rate- 1.19%, False negative rate- 4.76%
High false negative rate-4.76% was mainly because four cases that were diagnosed as follicular neoplasm (considered benign) on cytology were found to be follicular carcinoma on histopathology. This leads us to the conclusion that benign and malignant follicular neoplasms are difficult to differentiate from one another by FNAC leading to high false negative rate and can be confirmed only on histopathology.
Table 22: Comparison of diagnostic parameters on cyto-histopathological correlation in various studies
| Predictive values | Bukhari MH et al (1997) 49 |
Lopez LH et al (1997) 50 |
Flanagan MB et al (2006) 51 |
Chao TC et al (2007) 52 |
Present study |
| Sensitivity | 85% | 90% | 81.7% | 86.1% | 80% |
| Specificity | 90% | 99% | 56.4% | 59% | 98.44% |
| Accuracy | 87% | 99% | 82% | 64.6% | 94.05% |
| Clinical reliability | Reliable | Reliable | Reliable | Reliable | Reliable |
Table 22 shows that our diagnostic parameters on cyto-histopathological correlation are comparable to the other studies. In our study sensitivity was 80% which was lower than other studies but was closest to Flanagan MB et al (2006).51 The specificity and accuracy was 98.44% and 94.05% which were better than most mentioned studies except Lopez LH et al (1997).50
Conclusion
Thyroid cytology proves to be a reliable, simple, cheap, first-line diagnostic procedure with better patient compliance and without complications. The thyroid cytology results must be assessed in addition with clinical examination and other investigations like TFT/ USG findings. The cytology procedure has acceptable sensitivity and specificity in wide range group of patients in experienced hands. Hence thyroid cytology after USG-thyroid reporting can be used as a pre-operative diagnostic modality, thus reducing the number of surgeries. Studies to evaluate various diagnostic parameters are necessary in all cytology centers to improve upon technical as well as interpretative errors. A systematic, sequential, multi-modality approach of clinical examination, radiological diagnosis followed by cytological reporting is the need of the hour.
References
- Shuja A. History of thyroid surgery. Professional Med J 2008;15(2):295-7.
- Gritzmann N, Koischwitz D, Rettenbacher T. Sonography of the thyroid and parathyroid glands. In: Weber AL, editor. The Radiologic Clinics of North America. 3rd New York: Elsevier; 2000 .p. 1131-43.
CrossRef - Pandit AA and Kinare SG. Fine needle aspiration cytology of thyroid. Indian J Cancer 1986;23(1):54-8.
- Ananthakrishnan N, Rao KM, Narasimhans R, Veliath S, Smilet SR, Jagadish S. The Single Thyroid Nodule: A South Indian Profile of 503 Patients with Special Reference to Incidence of Malignancy. Indian J Surg 1993;55(10):487-92.
- Baloch Z, Livolsi V. Pathology of thyroid and parathyroid disease. In: Sternberg’s diagnostic surgical pathology. 4th Edinburgh: Lippincott Williams & Wilkins; 2004. p. 557-95.
- Kishore N, Shrivastava A, Sharma LK, Chumber S, Kochupillai N, Griwan MS, et al. Thyroid neoplasm. A profile. Indian J Surg 1996;58:143-8.
- Bhansali SK, Stocker RS, Bijlani JC, Dhungal JVP, Govindan V, Shanbhag VV. Some facets of non-toxic goiters: an appraisal of 884 cases. Indian J Surg 1973; 35:473-9.
- Rosai J, Carangiu ML, Delellis RA. Tumours of the thyroid gland.Atlas of tumor pathology, 3rd series, fascicle 5. Washington: Armed Forces Institute of Pathology, 1992.
- Singh P, Chopra R, Calton N, Kapoor R. Diagnostic Accuracy of Fine Needle Aspiration Cytology of Thyroid lesions. Journal of Cytology 2000;17(3):135-9.
- El Hag IA, Kollur SM, Chiedozi LC. The role of FNA in the initial management of thyroid lesions : 7-years experience in a district general hospital. 2003;14(3):126-30.
CrossRef - Sangalli G, Sergio G, Zampatti C, Bellotti M, Lomuscio G. Fine needle aspiration cytology of the thyroid: A comparison of 5469 cytological and final histological diagnosis. 2006;17(5):245-50.
CrossRef - Aravinthan T, Banagala ASK, Gamage KJPK. Use of fine needle aspiration cytology on thyroid lumps. Galle Medical Journal 2007;12(1):25-9.
CrossRef - Handa U, Sukant G, Mohan H, Nagarkar N. Role of fine needle aspiraton cytology in diagnosis and management of thyroid lesions: A study on 434 patients. J Cytol. 2008;25(1):13-7.
CrossRef - Mandal S, Barman D, Mukherjee A, Mukherjee D, Saha J, Sinha R. Fine needle aspiration cytology of thyroid nodules-evaluation of its role in diagnosis and management. J Indian Med Assoc. 2011;109(4):258-61.
- Chittawadagi BB, Karthikeyan TM, Rajeshwari M. Cyto-Morphological, Biochemical and Radiological Correlation of Various Thyroid Lesions at a Tertiary Care Center. Annals of Pathology and Laboratory Medicine 2018;5(8): A668-A673.
CrossRef - Maitra A. The Endocrine system.In: Kumar V, Abbas AK, Fausto N, Aster JC, editors. Robbin and Cotran Pathologic Basis of Disease. 8th Philadelphia: Saunders Elsevier; 2010. p. 1107-26.
- Hennessey JV. Physical examination of the thyroid gland. In: Braverman LE, Cooper DS, editors. Werner & Ingbar’s The thyroid: A fundamental and clinical text. 10th China: Lippincott Williams & Wilkins; 2013. p. 320-5.
- Liechty RD, Graham M, Freemeyer P. Benign Solitary Thyroid Nodule. Surg Gynecol Obstet. 1965;121:571-3.
- Kapila K, Sathar SA, Al-Rabah NA, Prahash A, Seshadri MS. Chronic lymphocytic (Hashimoto’s) thyroiditis in Kuwait diagnosed by fine needle aspirates. Saudi Med 1995;15(4):363-6.
CrossRef - Walker J, Findlay D, Amar SS, Small PG, Wastie ML, Pegg CA. A prospective study of thyroid ultrasound scan in the clinically solitary thyroid nodule.Br J Radiol;58(691):617-9.
CrossRef - Jayaram G, Orell SR. Thyroid. In: Orell SR, Sterrett GF, editors. Fine Needle Aspiration Cytology, 5th Gurgaon: Reed Elsevier India Private Limited; 2012. p. 118-55.
CrossRef - Kapre M, Vaidya AD. Surgery of thyroid. In: Hathiram BC, Khattar VS, editors. Atlas of operative otorhinolaryngology and head & neck surgery. New Delhi: Jaypee; 2013. p. 1410-21.
CrossRef - Godinho-Matos L, Kocjan G, Kurtz A. Contribution of fine needle aspiration cytology to diagnosis and management of thyroid disease. J Clin Pathol. 1992;45:391-5.
CrossRef - Jameson JL, Weetman AP. Disorders of the thyroid gland. Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Harrison’s principles of Internal Medicine. 16th ed. New York: McGraw-Hill; 2005. p. 2104-27.
- Simeone JF, Daniels GH, Mueller PR, Maloof F, vanSonnenberg E, Hall DA, et al. High-resolution real-time sonography of the thyroid. Radiology 1982;145(2):431-5.
CrossRef - Sanchez MA, Stahl RE. The Thyroid, Parathyroid, and Neck Masses Other Than Lymph Nodes. In: Koss LG, Melamed MR, editors. Koss’ Diagnostic Cytology And Its Histopathologic Bases. 5th China: Lippincott Williams & Wilkins; 2006. p. 1148-85.
- Hamburger JI, Husain M, Nishiyama R, Nunez C, Solomon D. Increasing the accuracy of fine-needle biopsy for thyroid nodules. Arch Pathol Lab Med.1989;113: 1035-41.
- Hall TL, Layfield LJ, Philippe A, Rosenthal DL. Sources of diagnostic error in fine needle aspiration of the thyroid. Cancer 1989;63:718-25.
CrossRef - Santos JEC, Leiman G. Non aspiration fine needle cytology: Application of a new technique to nodular thyroid disease. Acta Cytol 1988;32(3)353-6.
- Khan S, Maheshwari V, Aziz M, Hussain M, Verma AKJ. Cytology of Thyroid lesions with emphasis on Non-Aspiration Technique. J Cytol 2004;21(4):179-82.
- Maurya AK, Mehta A, Mani NS, Nijhawan VS, Batra R. Comparison of aspiration vs non aspiration techniques in fine needle cytology of thyroid cancers. J Cytol 2010;27(2):51-4.
CrossRef - Mishra M, Bandyopadhyay SP. Fine Needle Capillary Sampling (Non Aspiration Technique) vs Conventional FNAC in Cytological Diagnosis. J Cytol 2001;18(1):25-30.
- Rosen IB, Azadian A, Walfish PG, Salem S, Lansdown E. Ultrasound guided fine needle aspiration biopsy in the management of thyroid disease. Am J Surg 1993;166:346-9.
CrossRef - Hatada T, Okada K, Ishii H, Ichii S, Utsunomiya J. Evaluation of ultrasound guided fine needle aspiration biopsy for thyroid nodules. Am J Surg 1998;175:133-6.
CrossRef - Sankhla DK, Hussein SS, Bererhi H, El Shafie O, Woodhouse NJ, Nirmala V. Are scintigraphy and ultrasonography necessary before fine-needle aspiration cytology for thyroid nodules? J Sci Res Med Sci. 2001;3(1):29-33.
- Peter DP. The pharynx and larynx, the neck. In: David Sutton editor. Text book of radiology and imaging. 7th ed. London: Churchill Livingstone; 2003. p.1489-518.
- Cai XJ, Valiyaparambath N, Nixon P, Waghorn A, Giles T, Helliwell T. Ultrasound-guided fine needle aspiration cytology in the diagnosis and management of thyroid nodules. Cytopathology 2006;17(5):251-6.
CrossRef - Amrikachi M, Ramzy I, Rubenfeld S, Wheeler TM. Accuracy of thyroid fine needle aspiration of thyroid. Arch Pathol Lab Med 2001;125(4):484-8.
CrossRef - Mehrotra P, Hubbard JGH, Johnson SJ, Richardson DL, Bliss R, Lennard TWJ. Ultrasound scan-guided core sampling for diagnosis versus free hand FNAC of thyroid gland. Surgeon 2005;1:1-5.
CrossRef - Jen-Der-Lin, Bie-Yu Huang, Tzu-Chieh Chao. Diagnosis of Occult Thyroid Carcinoma by Thyroid Ultrasonography with Fine Needle Aspiration Cytology. Acta Cytol 1996;41(6):423-8.
CrossRef - Guhamallick M, Sengupta S, Bhattacharya NK, Basu N, Roy S, Ghosh AK, et al. Cytodiagnosis of thyroid lesions-usefulness and pitfalls: A study of 288 cases. J Cytol 2008;25(1):6-9.
CrossRef - Jones AJ, Aitman TJ, Edmonds CJ, Burke M, Hudson E, Tellez M. Comparison of fine needle aspiration cytology, radioisotopic and ultrasound scanning in the management of thyroid nodules. Postgrad Med J. 1990;66(781):914-7.
CrossRef - Watters DA, Ahuja AT, Evans RM, Chick W, King WW, Metreweli C, et al. Role of USG in the management of thyroid nodule. Am J Surg 1998;164(6):654-7.
CrossRef - Yassa L, Cibas ES, Benson CB, Frates MC, Doubilet PM, Gawande AA, et al. Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer 2007;111(6):508-16.
CrossRef - Yang J, Schnadig V, Logrono R, Wasserman PG. Fine-needle aspiration of thyroid nodules: a study of 4703 patients with histologic and clinical correlations. Cancer 2007;111(5):306-15.
CrossRef - Nayar R, Ivanovic M. The indeterminate thyroid fine-needle aspiration: experience from an academic center using terminology similar to that proposed in the 2007 National Cancer Institute Thyroid Fine Needle Aspiration State of the Science Conference. Cancer 2009;117(3):195-202.
CrossRef - Jo VY, Stelow EB, Dustin SM, Hanley KZ. Malignancy risk for fine-needle aspiration of thyroid lesions according to the Bethesda System for Reporting Thyroid Cytopathology. Am J Clin Pathol 2010;134(3):450-6.
CrossRef - Mondal SK, Sinha S, Basak B, Roy DN, Sinha SK. The Bethesda system for reporting thyroid fine needle aspirates: A cytologic study with histologic follow-up. J Cytol 2013;30(2):94-9.
CrossRef - Bukhari MH, Niazi S, Hanif G, Qureshi SS, Munir M, Hasan M, et al. An updated audit of fine needle aspiration cytology procedure of solitary thyroid nodule. Diagn Cytopathol. 2008;36(2):104-12.
CrossRef - Lopez LH, Canto JA, Herrera MF, Gamboa-Dominguez A, Rivera R, Gonzalez O, et al. Efficacy of fine-needle aspiration biopsy of thyroid nodules: Experience of a Mexican institution. World J Surg. 1997;21(4):408-11.
CrossRef - Flanagan MB, Ohori NP, Carty SE, Hunt JL. Repeat thyroid nodule fine-needle aspiration in patients with initial benign cytologic results. Am J Clin Pathol. 2006; 125(5):698-702.
CrossRef - Chao TC, Lin JD, Chao HH, Hsueh C, Chen MF. Surgical treatment of solitary thyroid nodules via fine-needle aspiration biopsy and frozen-section analysis. Ann Surg Oncol. 2007;14(2):712-8.
CrossRef







