Balakrishnan Sadasivam , Santenna Chenchula
, Santenna Chenchula  and Avik Ray
and Avik Ray
Department of Pharmacology, All India Institute of Medical Sciences Bhopal, Bhopal 462020, India
Corresponding Author E-mail: avik.jrpharma18@aiimsbhopal.edu.in
DOI : https://dx.doi.org/10.13005/bpj/2176
Abstract
Introduction: Urolithiasis is quite a common disorder affecting around two million people in India every year. Minimally invasive therapies are effective treatment measures in most of the cases. However, a watchful waiting approach with pharmacotherapy promotes the expulsion of stones in a shorter time. We hereby review the efficacy and safety of silodosin, a selective α-1A adrenoceptor antagonist, in medical expulsive therapy for the management of urolithiasis based on the evidences in Indian population. Methods: Medical Subject Headings (MeSH) keywords which were used to systematically search electronic databases: PubMed/Medline, Cochrane Library and Google Scholar from their inception to February 2020 were “Silodosin”, “Ureteral calculi”, “Medical expulsive therapy”, “India”, “randomised controlled trials” and “prospective observational studies”. A total of 29 relevant studies could be found and were included in our analysis. Results: The primary outcomes considered were the stone expulsion rate (SER) and stone expulsion time (SET) along with pain episodes and safety outcomes like orthostatic hypotension and retrograde ejaculation. Eight studies with a total of 1064 patients were identified as evidences considering Indian population which compared silodosin with controls like tamsulosin or tadalafil. Conclusions: Silodosin is highly effective in Indian population for increasing stone expulsion for those with ureteral stones (distal ureteral stones with diameter ≥5 mm and ≤10 mm) with shorter expulsion times along with fewer episodes of pain. It is also effective in post-lithotripsy for accentuating clearance rate and curtailing time to passage of the stones.
Keywords
Medical Expulsive Therapy; Randomized Controlled Trial; Silodosin; Ureteral Stone
Download this article as:| Copy the following to cite this article: Sadasivam B, Chenchula S, Ray A. Systematic Review of Efficacy and Safety of Silodosin in Medical Expulsive Therapy for the Management of Ureteral Stones – Based on Indian Evidences. Biomed Pharmacol J 2021;14(2). |
| Copy the following to cite this URL: Sadasivam B, Chenchula S, Ray A. Systematic Review of Efficacy and Safety of Silodosin in Medical Expulsive Therapy for the Management of Ureteral Stones – Based on Indian Evidences. Biomed Pharmacol J 2021;14(2). Available from: https://bit.ly/3ea4gue |
Introduction
Urolithiasis or stones in the urinary tract (UT) is a common disorder and is often associated with many complications of the UT. It affects about 5%-10% of the population and are often the cause for a rush to the Emergency Department (ED). Every year around two million people in India are affected with nephrolithiasis. Some specific parts of the country such as Gujarat, Maharashtra, Punjab, Rajasthan, Delhi and Haryana, along with some states in the North East, have been named together as a “stone belt area”. Even, different food habits like high intake of tamarind in regular diet is also thought to be commonly associated with kidney stone formation in people hailing from the southern parts of India.
There are various treatment options for urolithiasis such as minimally invasive therapies, in which, extracorporeal shock wave lithotripsy (ESWL) and ureterolithotripsy with ureteroscopy (URS) are highly effective in majority of the cases. However, these procedures are usually expensive and are associated with more than minimal risks1 . Generally, vigilant awaiting can lead to spontaneous calculi expulsion in up to 50% of cases along with some associated complications such as urinary tract infections (UTI), hydronephrosis and colickypain 2. Hence, making an informed decision based on the possible risks and benefits after taking the consent from the patient is necessary. Pharmacotherapy has a role for symptomatic relief and prevention of recurrence of ureteral stones. Some studies suggest that drugs usage promotes the expulsion of stones in a shorter time, allowing the stones to pass spontaneously. This is termed as the medical expulsive therapy (MET) 3,4.
MET is an alternative method for the early treatment of ureteral stones in selected patients by the use of various drugs acting on the smooth muscle of the ureter via different mechanisms 5. Apart from vigilant awaiting approach and MET, the other treatment options have a lot of healthcare burden associated with them. Patients tend to prefer MET as it facilitates spontaneous passage of ureteral stones. There are various pharmacological group of drugs used for MET including α-antagonists, dihydropyridine calcium channel blockers (DHPs) such as nifedipine and phosphodiesterase inhibitors such as sildenafil and tadalafil 6. These drugs have shown to facilitate distal ureteral stone expulsion. Among them, α-blockers offer more benefits than the others and are the most commonly used treatment agents. It includes drugs such as tamsulosin, alfuzosin, doxazosin, terazosin, naftopidil and silodosin 6.
Trials and guidelines
In the year 2015, MET was recommended in the United Kingdom (UK) to help in the passage of small ureteral stones. The famous SUSPEND trial, one of the largest randomized controlled trial on this therapy, showed that there were not much clinical benefits from the use of α-receptor blockers 7. However, recent trials have concluded that α-receptor blockers can help in the expulsion of ureteral stones and thus, reduce the pain associated with the passage of stones.
International guidelines formed by the National Institute for Health and Care Excellence (NICE), American Urological Association (AUA) and the European Association of Urology (EAU) for the treatment of ureteral calculi suggest that in newly diagnosed individuals with ureteral stones with diameters ranging from 5 mm to 10 mm besides controlled symptoms, observation along with frequent evaluation is a choice for early treatment. Appropriate medical therapy in order to facilitate stone passage might be offered during the observation period. A prerequisite for MET is that the patient should be well informed and reasonably comfortable with the management approach and that there is no definite benefit of immediate active removal of stone. Additionally, it is a cost-effective option to treat urolithiasis and the high expenditures of the other treatment methods are avoided.
α-Adrenergic receptors (α-AR) are of three subtypes: α-1A, α-1B, and α-1D. In the urogenital area (namely prostate, bladder base, bladder neck, and ureter), α-1A and α-1D ARs are mainly present and they lead to smooth muscle contraction in these tissues. In the human ureter, α- AR distribution follows the order: α-1D > α-1A > α-1B in terms of their numbers. In particular, α-1D receptors are found more in the distal third of the ureter and show their effect on the detrusor muscle and smooth muscle contraction in the ureter. Recent international standard guidelines have recommended α-AR blockers for the treatment of adults and young people with ureteral stones 8. Blocking the activity of these receptors leads to accentuation in the ureteral pressure gradient around the obstructed ureter by raising the bolus of urine above the stone and decreasing the ureteral pressure below it, resulting in ureteric lumen dilatation, thus facilitating anterograde stone propagation. Further, α1-adrenoceptor blockers attenuate the frequency of ureteric peristaltic contractions and ureteral colic, with areduction in the need of an analgesic. The older α1-AR blockers with quinazo line side chain, such as doxazosin or terazosin, display non-specific interactions with all sub types of α1-AR. Drugs like naftopidil and tamsulosin show relatively high selectivity for α1A and α1D receptor subtypes and are effective in relieving symptoms related to urinary tract obstructive symptoms without any adverse effects on blood pressure. Before the usage of silodosin in MET, many clinical studies have shown that tamsulosin facilitates effective ureteral stone expulsion.
Silodosin, a recently introduced selective α-1A AR antagonist, which was approved in the year 2006 in Japan, is now licensed in more than 50 more countries, including the United States and Europe, for the management of Lower Urinary Tract Symptoms (LUTS) because of Benign Prostatic Enlargement (BPH). A study concluded that a selective α-1D receptor antagonist may be more beneficial for stone expulsion than an alpha-1A receptor antagonist 9. Another study has shown that α-1A adrenoceptor blockers use can lead to more effective stone expulsions than α-1D adrenoceptor blockers. Silodosin in the dose range of 8 mg once daily has shown to have an equal affinity towards α-1D receptor subtype similar to tamsulosin, but the affinity of silodosin for the α-1A receptors is almost 38-fold higher than that of tamsulosin 10.
Materials and methods
We searched for relevant clinical studies in PubMed, Google Scholar and Cochrane library with the following medical subject headings (MeSH) terms and keywords in any combination with boolean operators “AND” or “OR”: “silodosin”, “ureteral calculi”, “medical expulsive therapy”, “India” “randomised controlled trials” and “prospective observational studies”. Other grey literature was also searched for any relevant information. We have considered both randomized controlled trials and observational studies that compared silodosin with placebo or positive controls such as tamsulosin, naftopidil, sildenafil or tadalafil for ureteral calculi management. A total of 29 published studies could be found from inception through February 2020. Figure 1 shows the search strategy. The outcomes of interest for us were expulsion rate (ER), expulsion time (ET) along with number of episodes of pain besides safety outcomes such as incidences of orthostatic hypotension and retrograde ejaculation.
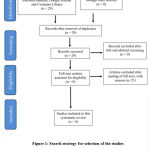 |
Figure 1: Search strategy for selection of the studies included in the systematic review. |
Results and Discussion
Expulsion rate
A meta-analysis based on five case series with a total of 224 patients having stones ≤5 mm in diameter showed that a stone passage rate of 68% for stones less than or equal to 5 mm in diameter gets decreased to 47% for stones of 5-10 mm in diameter 10. The distal ureteral calculi of size ≤5 mm in diameter have >90% chance of spontaneous expulsion and are suitable for traditional management, given that there are symptoms of infection or any indication of renal injury. Stones ≥5 mm in diameter have lesser chance to pass spontaneously with conservative treatment and other treatment modalities should be explained to the patients 11. Silodosin showed a very higher expulsion rate than placebo for stone which are 5-10 mm in diameter as compared to in cases with stone diameter ≤5 mm 11-15.
Expulsion time
In a study it was shown that around 95% of stones with diameter<4 mm passed within 40 days of conservative treatment alone 11. However, for larger stones of 5-10 mm in diameter, silodosin provided a higher stone expulsion rate of 14% as compared to tamsulosin. The mean ET (in days) of distal ureteral stones treated with silodosin were between 6.5 to 16.7 days 12-14. In a prospective randomized study, individuals with symptomatic unilateral ureteral calculi of < 10 mm in diameter were given silodosin (8 mg/day) with instructions to drink two litres of water daily for a maximum of eight weeks. Overall, the mean ET was 10.27 ± 8.35 days 14. For distal ureteral stones, the mean ET was 9.29 ± 5.91 days. For stones with diameter 1‐5 mm, the mean ET was 9.56 ± 8.45 days while for stones with diameter <10 mm, it was 11.33 ± 8.31 days 14.
The time to expulsion can be affected by many factors like site of stone, size and presence or absence of spasms and submucosal edema. Lesser the stone expulsion time is, lesser would be the episodes of pain and the requirement of an analgesic. Silodosin has comparable efficacy with placebo in terms of the requirement of analgesics for attenuating the pain 13.
Safety outcomes
The most common adverse drug reaction reported with silodosin was retrograde ejaculation followed by dizziness. Other adverse reactions reported were orthostatic hypotension, nasal congestion and headache along with diarrhea 12,16. In studies that compared silodosin with tamsulosin, the former showed significantly higher incidence of retrograde ejaculation which gets completely and promptly reversed within a few days after the discontinuation of treatment 11,14,17-20.
Evidence in Indian population.
Till now, very few studies for estimating the efficacy and safety of silodosin in MET for the management of distal ureteral calculi have been conducted on Indian patients. A total of eight studies based on Indian population were found with a total of 1064 patients 21-28. In all of these studies, silodosin was compared with either tamsulosin or tadalafil. In one randomized controlled pilot study, 285 patients with distal ureteric stones of diameter 5-10 mm were randomized to one of the three treatment arms: tamsulosin, silodosin, and tadalafil on an out-patient basis. They concluded that silodosin significantly increases ureteric stone expulsion besides better regulation of pain and significantly lesser analgesic requirements 21. In another randomized controlled trial,silodosin came out to be clinically superior to tamsulosin, both in terms of stone expulsion rate and stone expulsiontime 22. Further, in another randomized trial, it was observed that patients receiving silodosin expelled ureteric stones in lesser time with the mean expulsion time being lesser than the tamsulosin group.
In some studies which reported episodes of pain, it was observed that silodosin was associated with fewer episodes of pain as compared to tamsulosin and other drugs 24-28. In many of the included studies of MET with silodosin, the results showed a lower incidence of adverse effects due to the peripheral vasodilatation but a higher incidence of retrograde ejaculation as compared to tamsulosin 24-27. However, most of these studies have some important limitations including a small sample size of the randomized controlled trials and hence, subgroup analysis based on size of the stones, an important parameter that affects the chances of spontaneous passage of the stones, could not be performed.
Our systematic review shows that silodosin, a predominant selective α-1A receptor blocker which has been approved for the treatment of LUTS/BPH, is an effective and safe drug for MET of distal ureteral stones and is clinically superior in terms of stone expulsion rate, stone expulsion time and analgesic requirements as compared to its controls for stones with diameter of ≥5 mm and ≤10 mm. Additionally, it is associated with limited adverse effects, of which, majority was retrograde ejaculation, which caused withdrawal from the treatment for a very small population 19,21. This is further backed by systematic review of the evidences in the Indian population. Even in the treatment of large distal ureteral stones, silodosin therapy before ureteroscope (URS) has been found to be correlated with better advancing of the URS to reach the stone along with a reduced procedure time, higher stone-free rate, lesser postoperative complications and lesser requirements for postoperative analgesia [15]. Hence, silodosin 8 mg once daily is an effective and well-tolerated medical therapy for the management of distal ureteral calculi 16-18.
Conclusion
When compared with the controls such as tamsulosin, naftopidil, tadalafil, and sildenafil, silodosin showed to be more efficacious and associated with a better safety profile in all the considered clinical outcomes. Based on the data of the nine identified studies on Indian population it can be concluded that silodosin is more efficacious and safer over other drugs which are commonly employed for MET for stones with diameter ≤10 mm. It is also efficacious in post-lithotripsy for increasing clearance rate, reducing time taken for the passage of the stone and attenuating renal colicky pain with most benefits for stones >10 mm in diameter which are located in the renal pelvis, mid-upper calyx or mid-upper ureter. In conclusion, for distal ureteral calculi size of 5-10 mm diameter and for those who are willing to await therapy, MET should preferably be offered as a cost-effective treatment option.
Acknowledgement
None
Conflict of Interest
We declare no conflict of interest.
Funding Source
This study has not received any specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- Colella J, Kochis E, Galli B, Munver R: Urolithiasis/nephrolithiasis: what’s it all about?. Urol Nurs. 2005;25:427-449.
- Dellabella M, Milanese G, Muzzonigro G: Randomized trial of the efficacy of tamsulosin, nifedipine and phloroglucinol in medical expulsive therapy for distal ureteral calculi. J Urol. 2005;174:167-172.
CrossRef - Borghi L, Meschi T, Amato F, Novarini A, Giannini A,Quarantelli C, Mineo F: Nifedipine and methylprednisolone in facilitating ureteral stone passage: a randomized, double-blind, placebo-controlled study. J Urol. 1994;152:1095-1098.
CrossRef - Clayman RV: Effectiveness of nifedipine and deflazacort in the management of distal ureter stones. J Urol. 1994;167:797-798.
- Tzortzis V, Mamoulakis C, Rioja J, Gravas S, Michel MC, de la Rosette JJ: Medical expulsive therapy for distal ureteral stones. Drugs. 2009;69:677-692.
CrossRef - Sridharan K, Sivaramakrishnan G: Efficacy and safety of alpha blockers in medical expulsive therapy for ureteral stones: a mixed treatment network meta-analysis and trial sequential analysis of randomized controlled clinical trials. Expert Rev Clin Pharmacol. 2018;11:291-307.
CrossRef - Assimos D, Krambeck A, Miller NL, et al.: Surgical management of stones: american urological association/endourological society guideline, part i. J Urol. 2016; 196:1153-1160.
CrossRef - Preminger GM, Tiselius HG, Assimos DG, et al.: 2007 guideline for the management of ureteral calculi. J Urol. 2007;178:2418‐2434.
CrossRef - Itoh Y, Kojima Y, Yasui T, Tozawa K, Sasaki S, Kohri K: Examination of alpha 1 adrenoceptor subtypes in the human ureter. Int J Urol. 2007;14:749‐753.
CrossRef - Campschroer T, Zhu X, Vernooij RW, Lock MT: Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2018; 4:CD008509.
CrossRef - Rahman MJ, Faridi MS, Mibang N, Singh RS: Comparing tamsulosin, silodosin versus silodosin plus tadalafil as medical expulsive therapy for lower ureteric stones: a randomised trial. Arab J Urol. 2017;16:245-249.
CrossRef - Huang W, Xue P, Zong H, Zhang Y: Efficacy and safety of silodosin in the medical expulsion therapy for distal ureteral calculi: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016;81:13-22.
CrossRef - Coll DM, Varanelli MJ, Smith RC: Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical ct. Am J Roentgenol. 2002;178:101-103.
CrossRef - Itoh Y, Okada A, Yasui T, et al.: Efficacy of selective α1A adrenoceptor antagonist silodosin in the medical expulsive therapy for ureteral stones. Int J Urol. 2011; 18:672-674.
CrossRef - Ding H, Ning Z, Dai Y, Shang P, Yang L: The role of silodosin as a new medical expulsive therapy for ureteral stones: a meta-analysis. Ren Fail. 2016;38:1311-1319.
CrossRef - Yuceturk CN, Dadali M, Bagbanci MS, et al.: Efficacy of silodosin dose in medical expulsive therapy for distal ureteral stones: a retrospective study. Urol J. 2017; 14:2944-2948.
- Elgalaly H, Eliwa A, Seleem M, et al.: Silodosin in the treatment of distal ureteric stones in children: a prospective, randomised, placebo-controlled study. Arab J Urol. 2017;15:194-198.
CrossRef - Hsu YP, Hsu CW, Bai CH, Cheng SW, Chen KC, Chen C: Silodosin versus tamsulosin for medical expulsive treatment of ureteral stones: a systematic review and meta-analysis. PLoS ONE. 2018;13:e0203035.
CrossRef - Amer T, Osman B, Johnstone A, et al.: Medical expulsive therapy for ureteric stones: analysing the evidence from systematic reviews and meta-analysis of powered double-blinded randomised controlled trials. Arab J Urol. 2017;15:83-93.
CrossRef - Dell’Atti L: Silodosin versus tamsulosin as medical expulsive therapy for distal ureteral stones: a prospective randomized study. Urologia. 2015;82:54-57.
CrossRef - Kumar S, Jayant K, Agrawal MM, Singh SK, Agrawal S, Parmar KM: Role of tamsulosin, tadalafil, and silodosin as the medical expulsive therapy in lower ureteric stone: a randomized trial (a pilot study). Urology. 2015;85:59-63.
CrossRef - Gupta S, Lodh B, Singh AK, Somarendra K, Meitei KS, Singh SR: Comparing the efficacy of tamsulosin and silodosin in the medical expulsion therapy for ureteral calculi. J Clin Diagn Res. 2013;7:1672-1674.
CrossRef - S Naseeruddin, SS Kendri, N Imdad Ali. Comparative study of efficacy of silodosin and tamsulosin in patients of lower ureteric calculi in a tertiary care hospital. Oral Session Abstracts. Indian J Pharmacol 2015;47:S1:13-57
- Priyanka P, Jadhav R R. Comparison between Tamsulosin and Silodosin in Lower Ureteric Stone- a randomized Controlled Study. J Evol Med Dent Sci2017;6:6766–6769.
CrossRef - Rathi S, Agarwal A, Patnaik P, Shaw D, Trivedi S, Dwivedi U. Evaluation of medical expulsive therapy for distal ureteral stone: a prospective randomized controlled study to compare silodosin versus tamsulosin. Indian J Urol 2014;30:S83.
- Sharma G, Khadav B, Sandhasukhi TC, Gupta M, Gupta H L. Comparative analysis of silodosin and tamsulosin in distal ureteric calculus treatment. Int J Evid Based Healthc. 2016;3:4647–9.
CrossRef - Reddy S, Prathvi P, Kulshreshtha M, Singh P. A Prospective Study Comparing Tamsulosin and Silodosin in Medical Expulsive Therapy for Lower Ureteric Stones. J Evol Med Dent Sci. 2016;5:4108–4111.
CrossRef - Arun A, Jayaprakasha G, N Imdad A: Comparative efficacy of silodosin vs tamsulosin for ureteric calculus: a single centre double blind randomised controlled trial. J Med Sci Clin Res. 2017;5:31928-31932.
CrossRef








