Department of Physiotherapy, SRM College of Physiotherapy, Faculty of Medical and Health Sciences, SRM Institute of Science and Technology,SRM Nagar, Kattankulathur, 603 203 Kanchipuram, Chennai, Tamilnadu, India.
Corresponding Author E-mail: anandhid@srmist.edu.in
DOI : https://dx.doi.org/10.13005/bpj/2131
Abstract
BACKGROUND: Incentive spirometry is a device which helps in the improvement of lung function after abdominal surgery. It motivates the patients by giving visual feedback about their lung volumes. It is one of the less expensive and user-friendlydevices. Incentive spirometry facilitates the patients to take slow deep breath and there by producing a sustained maximal inspiration (SMI) that mainly helps in the prevention of atelectasis. But it is a common practice for physiotherapists to teach the patients to do expiratory exercise by reversing the incentive spirometer. The simplest way to measure the maximal inspiratory and expiratory pressures is by respiratory pressure meter in cmH2o. OBJECTIVE: To find out the efficacy of incentive spirometer in improving the expiratory muscle strength following abdominal surgery. METHODOLOGY: Quasi-Experimental study. PROCEDURE: 30 subjects were conveniently selected based on inclusion and exclusion criteria and allotted to group A (n=15) and group B (n= 15). Both groups were trained for inspiratory muscle and group A was also trained for expiratory muscle using incentive spirometry. OUTCOME MEASURES: Maximal inspiratory pressure (MIP), Maximal expiratory pressure (MEP). RESULT: This study shows that the mean MIP value have improved from 2nd to 7th postoperative day, but it is not statistically significant (P>0.05). The mean MEP values shows statistically significant (P<0.05) improvement from second to 7th postoperative day in group A when compared to group B. CONCLUSION:This study concludes that there is significant improvement in the expiratory muscle strength along with inspiratory muscle strength by training with the Incentive spirometry in the upside down and upright positions respectively.
Keywords
Forced Expiratory Volume; Incentive Spirometer; Maximal Inspiratory Pressure; Maximal Expiratory Pressure; Respiratory Pressure Meter; Sustained Maximal Inspiration
Download this article as:| Copy the following to cite this article: Gayathiri T, Anandhi D. Efficacy of Incentive Spirometry in Expiratory Muscle Training Following Abdominal Surgery. Biomed Pharmacol J 2021;14(1). |
| Copy the following to cite this URL: Gayathiri T, Anandhi D. Efficacy of Incentive Spirometry in Expiratory Muscle Training Following Abdominal Surgery. Biomed Pharmacol J 2021;14(1). Available from: https://bit.ly/38ElIEm |
Introduction
Incentive spirometry is a device which helps in the improvement of lung function. It motivates the patients by giving visual feedback about their lung volumes1. It is one of the less expensive and user friendly device3. Incentive spirometry facilitates the patients to take slow deep breathe and there by producing a Sustained Maximal Inspiration (SMI) that mainly helps in the prevention of atelectasis 2,4.
Incentive spirometry is designed to mimic natural sighing or yawning by encouraging the patient to take long, slow, deep breaths. This decreases pleural pressure, promoting increased lung expansion and better gas exchange7. Incentive spirometry is classified into two types, they are Volume oriented and Flow oriented6. According to earlier study, there will be increased work of breathing and increased muscle activity of upper chest in flow-oriented device, but less work of breathing and improved diaphragmatic activity in volume oriented device8.Tachypnea and paradoxical abdominal chest movement are the signs of fatigue during breathing6. After thoracic or abdominal surgery incentive spirometry is done mandatory for 10 times per hour 9.
Abdominal surgery is defined as any surgical operation done on the abdominal cavity, its walls and orifice5. Post-operative complications are reported in the range of 2-39% in upper abdominal surgery, due to the surgery closer to diaphragm and 2-5% in lower abdominal surgery10. The common complications after abdominal surgery are: atelectasis, pneumonia, bronchitis, pneumothorax, bronchospasm, chronic lung disease. Post-operative pulmonary
complication is about 80% in upper abdominal surgery; they cause changes in pulmonary function and respiratory mechanics11.
They are always due to the anaesthesia (general, local), type of incision and the surgical technique undergone. At last they decrease the Forced Vital Capacity (FVC) and Forced Expiratory Volume(FEV)12. Due to shallow breathing, temporary diaphragmatic dysfunction, decreased mucociliary clearances and decreased cough effectiveness result in lack of lung inflation13. Patients should be advised to move early after the abdominal surgery which plays important component of post-operative care14.
The most familiar method to obtain the strength of respiratory muscle is by vital capacity, maximal inspiratory method and maximal expiratory method15. The estimation of maximal inspiratory pressure and maximal expiratory pressure is by using respiratory pressure meter (RPM), it is one of the non-invasivemethods by which the strength of respiratory muscles is assessed16.
Strength of diaphragm and other inspiratory muscles reflects the maximal inspiratory pressure (MIP) and strength of abdominal muscles and other expiratory muscles reflects the maximal expiratory pressure(MEP)17. The simplest way to measure the maximal respiratory pressure is by respiratory pressure meter in cmH2O stated by Black and Hyatt in 196918. Respiratory pressure meter(RPM) displays as a digital read out peak pressure for inspiratory and expiratory effort19.
The maximal sub atmospheric pressure created during inspiration against a blocked airway is known as maximal inspiratory pressure(MIP). The maximal expiratory force against a blocked airway known as maximal expiratory pressure(MEP)20. Disadvantage of the device is that the patient with the bulbar and facial weakness are prone to get imperfect outcomes as they cannot keep their lip tight around the mouthpiece22. Advantage of the device is that it can be used by paediatric and adult patients over the age of 3 years21.
Incentive spirometry by principle, is so far used to train only the inspiratory muscles. But it is a common practice for few physiotherapists to teach the patients to do expiratory exercise by reversing the incentive spirometry. Early studies suggest that, strength of both inspiratory and expiratory muscles decreases after abdominal surgery. There is no published literature on the use of incentive spirometry in improving the expiratory volumes and capacities. Hence the need of the study is to check the effect of incentive spirometry in upside down position training, to improve expiratory muscles strength following abdominal surgery.
Materials Used
Incentive spirometer (Ramson’s respirometer)
Respiratory pressure meter
 |
Figure 1: Incentive spirometer |
 |
Figure 2: Respiratory pressure meter |
Methods
30 abdominal surgery patients both men and women whose age between 30-60 years were included. Patients undergoing any emergency laparotomy, Malignancy, Cardiac conditions, Pulmonary conditions, Immediate post-operative complication were excluded in this study.
The procedure was described to subjects and written consent was obtained. This study cleared institutional ethical clearance. Prior to the surgery, patient’s confidence was gained by educating about the working and advantage of the device. Subjects were conveniently allocated to Group A (n=15) who trained in incentive spirometry in both upright and upside position and Group B (n=15) who trained in incentive spirometry in upright position alone.
Group A patients were made to sit upright in a bed with back support holding the incentive spirometry at the eye level. The patients were asked to hold a pillow at the site of incision in order to decrease the pain in the area of incision. The patients were asked to take three normal breaths before the mouth piece was held on their mouth and they were asked to hold it tightly by their lips. Now the patients were asked to take deep breath slowly through their mouth and asked to hold the balls as high as possible for 3 seconds. Once the ball reached the base of spirometry, the patients were asked to breath out slowly. Then they were asked to repeat these steps for 10 times per hour. With sufficient break they were asked to hold incentive spirometry in upside down position and exhale through mouth piece as much as possible. This procedure was repeated for 10 times per hour.
Group B patients were asked to use incentive spirometer only in upright position (10 times per hour).Both groups were asked to use incentive spirometry whenever they are awake.They were also instructed to use it after one hour of their meal.
The strength of respiratory muscles (Maximal inspiratory pressure and maximal expiratory pressure) was evaluated using respiratory pressure meter for both groups pre operatively, on the second post-operative day and on the seventh post-operativeday(POD). Patients were made to sit with back support. By placing inspiratory mouth piece they were asked to breath in hard and three trails were taken with adequate intervals, from that the best score was recorded in the assessment sheet. This shows the Maximal Inspiratory Pressure(MIP) of the individual is in cm of H2O. Then by placing expiratory mouth piece they were asked to breath out hard and three trails were taken with adequate interval, from that the best score was recorded in the assessment sheet. This shows the Maximal Expiratory Pressure(MEP) of the individual is in cm of H2O.
Results and Discussion
Table 1 and graph 1 shows the mean MIP values of group A has improved from 23.66on II POD to 41.33 on the VII POD and that of group B has improved from 16.26 on II POD to 47.46 on the VII POD. There is no statistically significant difference (p>0.05) between group A and B in MIP on the VII POD.
Table 1: Comparison Of Mip Between Group A And B Preoperatively, On The Ii Pod And Vii Pod
| POD | GROUP | MEAN | SD | MEAN DIFFERENCE ( 95% CI) |
t- STATISTIC (df) |
P -VALUE |
| BEFORE
SURGERY |
A
(n=15) |
64.73 | 13.79 | -6.07 | -1.47 | 0.15 |
| B
(n=15) |
70.80 | 8.11 | ||||
| SECOND POD | A
(n=15) |
23.66 | 13.24 | 7.40 | 1.97 | 0.05 |
| B
(n=15) |
16.26 | 6.08 | ||||
| SEVENTH POD | A
(n=15) |
41.33 | 15.24 | -6.13 | -1.32 | 0.19 |
| B
(n=15) |
47.46 | 9.57 |
(p<0.05)
Table 1 shows the mean MIP values of group A has improved from 23.66 on II POD to 41.33 on the VII POD and that of group B has improved from 16.26 on II POD to 47.46 on the VII POD. There is no statistically significant difference (p>0.05) between group A and B in MIP on the VII POD.(p<0.05)
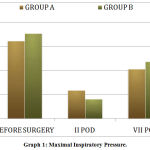 |
Graph 1: Maximal Inspiratory Pressure |
Table 2 and graph 2 shows the mean MEP values of group A has improved from 25.13on II POD to 45.20 on the VII POD and that of group B has improved from 14.73 on II POD to 21.46 on the VII POD. There is statistically significant difference (p<0.05) between group A and B in MEP on the VII POD.
Table 2: Comparison Of Mep Between Group A And B Preoperatively, On The Ii Pod And Vii Pod
| POD | GROUP | MEAN | SD | MEAN DIFFERNCE (95% CI) |
t- STATISTIC (df) |
P -VALUE |
| BEFORE
SURGERY |
A
(n=15) |
65.26 | 11.82 | -0.867 | -0.20 | 0.84 |
| B
(n=15) |
66.13 | 12.49 | ||||
| SECOND POD | A
(n=15) |
25.13 | 14.36 | 10.40 | 2.71 | 0.01 |
| B
(n=15) |
14.73 | 3.67 | ||||
| SEVENTH POD | A
(n=15) |
45.20 | 12.31 | 23.73 | 7.07 | 0.00 |
| B
(n=15) |
21.46 | 4.18 |
(p<0.05)
Table 2 shows the mean MEP values of group A has improved from 25.13 on II POD to45.20 on the VII POD and that of group B has improved from 14.73 on II POD to 21.46 on the VII POD. There is statistically significant difference (p<0.05) between group A and B in MEP on the VII POD.
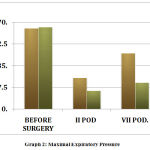 |
Graph 2: Maximal Expiratory Pressure |
Discussion
The main objective of the study is to find out the efficacy of incentive spirometry in improving the expiratory muscle strength following abdominal surgery when the incentive spirometry is used in upside down position. The improvement is actually measured by respiratory pressure meter. Vincken, et al., states that the maximal inspiratory pressure in male is 105 ±25 and female is 71± 23, maximal expiratory pressure male is 140± 38 and female is 89 ±24. This study shows that the mean values of maximal inspiratory pressure and maximal expiratory pressure in both groups show improvement on comparing from second to seventh post-operative day. There is no statistically significant difference (p>0.05) between group A and B in MIP on the VII POD.Studies have proved that during maximal inspiration there will be increased production of surfactant, improved compliance and oxygenation23,24.
Once after abdominal surgery, patients tend to have breathing difficulty and reduced cough effort due to pain and anaesthetic effect. The use of incentive spirometry has effect on respiratory muscles which reduces postoperative pulmonary complications. Incentive Spirometry is the most widely prescribed technique for preoperative and postoperative lung expansion. It is characterized by active recruitment of the diaphragm and other inspiratory muscles. During erect position of spine, the chest wall is symmetrical, any improper positioning like slouching, leaning over the affected side due to pain that reduces the alveolar ventilation and addition to that there will be mucociliary disturbances which end up in stagnation of mucus and results in infection25. SR Kulkarni reveals that use of incentive spirometry decreases post pulmonary complications but systemic analysis does not support in the reduction of post pulmonary complication.
In inspiratory phase using incentive spirometry there will be thoracic expansion which reduces the pleural pressure that transmit to alveoli. Trans respiratory Pressure gradient will be created between alveoli and airway opening which causes air to flow from the alveoli. On seventh post-operative day, the mean value of MIP improved in group B which underwent only inspiratory muscle training than group A which underwent inspiratory and expiratory training but it is not statistically significant. Overend, et al., states that incentive spirometry does not support in reducingpulmonary complication after abdominal surgery.
There is statistically significant difference (p<0.05) between group A and B in MEP on the VII POD. This study reveals that there is more improvement in expiratory muscle strength which is trained by incentive spirometry. For effective level of gaseous exchange, the strength of respiratory muscle pump is important25.
During spontaneous expiration the chest wall recoils, which reverses the transrespiratory gradient. Now the alveolar pressure rises above atmospheric pressure that cause gas to flow from alveoli to atmosphere. Paltiel et al concluded that lung functions like FEV1 can be increased significantly when incentive spirometry and specific inspiratory muscle training are used before and after operation26. FEV1 is an expiratory function of the lungs which can be improved only when the expiratory muscles strength is adequate. So, this shows indirectly that MEP will also be improved after Incentive spirometry training.
According to the AARC clinical practice guidelines, Incentive Spirometry should be contrasted with expiratory maneuvers which do not have sigh mechanism and have been associated with reduction of lung volumes.Yet our study has proved that MEP values have improved after using incentive spirometry in the upside down position. It can be due to the fact that respiratory muscles can be trained just like the skeletal muscles by training in the upright and upside-down positions with visual feedback and also by the principle, that when the muscles are stretched to the ideal or optimal length it can produce maximum muscular contraction.
Conclusion
This study concludes that there is significant improvement in the expiratory muscle strength along with inspiratory muscle strength by training with the Incentive spirometry in the upside down and upright positions respectively.
Acknowledgment
I extend my gratitude to all the Participants who consented to be the models for my study, without whose consent my study would be incomplete.
Conflict of Interest
No conflict of interest.
Funding Resource
There are no funding source.
References
- The cleveland clinic foundation retrieved 2013/11/03.
- Hough A, Physiotherapy in respiratory and cardiac care, an evidence based approach 4th Cengage learning 2014.p 186-189.
- O’Donohue WJ. Prevention and treatment of postoperative atelectasis: Can it and will it be adequately studied?. Chest. 1985 Jan 1;87(1):1-2.
CrossRef - Porter S. Tidy’s Physiotherapy E-Book. Elsevier Health Sciences; 2013 Jan 17.
- Isabel Spradlin. Abdominal surgery. statistics oct 14,2013.
- Kacmarek RM, Stoller JK, Heuer A. Egan’s Fundamentals of Respiratory Care E-Book. Elsevier Health Sciences; 2019 Dec 18.
- Renault JA, Coata-val R, Rossett MB. Respiratory physiotherapy in the pulmonary dysfunction after cardiac surgery. Rev bras circardiovas 2008 23(4) 562-569.
CrossRef - Agostini P, Singh S. Incentive spirometry following thoracic surgery: what should we be doing?. Physiotherapy. 2009 Jun 1;95(2):76-82.
CrossRef - AARC clinical Practice guidelines; respiratory care 191;36(12).
- Fisher BW, Majumdar SR, McAlister FA. Predicting pulmonary complications after nonthoracic surgery: a systematic review of blinded studies. The American journal of medicine. 2002 Feb 15;112(3):219-225.
CrossRef - AmaravadiSampathkumar, Gopala krishnaalarpathi, Alfred Joseph Augustine, Zulfeequerchundaanveetil, Pazhagaohayil. aerobic exercise training and incentive spirometry can control post pulmonary complication. After laparoscopic cholecystectomy.2015 459-463.
- El-Markby AA, Darweish, Anwar E, Mostafa EL-Gendysr, Gaowgzeh RA, etal. Aerobic exercise training and incentive spirometry can control post pulmonary complication. After laparoscopic cholecystectomy.2015 459-463.
- Overend TJ, Anderson CM, Lucy SD, Bhatia C, Jonsson BI, Timmermans C. The effect of incentive spirometry on postoperative pulmonary complications: a systematic review. Chest. 2001 Sep 1;120(3):971-978.
CrossRef - Browning L, Denehy L, Scholes RL. The quantity of early upright mobilisation performed following upper abdominal surgery is low: an observational study. Australian Journal of Physiotherapy. 2007 Jan 1;53(1):47-52.
CrossRef - Black and Hyatt 1969, Vicken et.al 1987,Working party standardisation of lung function test 1993.
- Smyth,M.SC,kennethR.Chapman.M.D,F.C.C.R,Anthonys.Rebuck,M.D, F.C.C.P.Reference value for lung function test maximal respiratory pressure and voluntary ventilation.
- Schoser B, Fong E, Geberhiwot T, Hughes D, Kissel JT, Madathil SC, Orlikowski D, Polkey MI, Roberts M, Tiddens HA, Young P. Maximum inspiratory pressure as a clinically meaningful trial endpoint for neuromuscular diseases: a comprehensive review of the literature. Orphanet journal of rare diseases. 2017 Dec 1;12(1):52.
CrossRef - Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. American review of respiratory disease. 1969 May;99(5):696-702.
- Hamnegard CH, Wragg S, Kyroussis D, Aquilina R, Moxham J, Green M. Portable measurement of maximum mouth pressures. European Respiratory Journal. 1994 Feb 1;7(2):398-401.
CrossRef - Ruppel G. Manual of pulmonary function testing. Mosby Incorporated; 2003.
- Care fusion manual book, operating manual PDF.
- RA Lyall,N.Donaldson, M.I policy,P.N.Leigh, J.Moxham. lung function test1993.
- Williams JV, Tierney DF, Parker HR. Surface forces in the lung, atelectasis, and transpulmonary pressure. J Appl Physiol.1960;21:819- 827.
CrossRef - Zikria BA, Spencer JL, Michailoff T, Broell JR, Kinney JM. Breathing patterns in preoperative, postoperative, and criticlly ill patients. InSurgical forum 1971 (Vol. 22, p. 40).
- Frownfelter D, Dean E. Cardiovascular and pulmonary physical therapy-E-Book: evidence to practice. Elsevier health sciences; 2014 Mar 12.
- Weiner P, Man A, Weiner M, Rabner M, Waizman J, Magadle R, Zamir D, Greiff Y. The effect of incentive spirometry and inspiratory muscle training on pulmonary function after lung resection. The Journal of thoracic and cardiovascular surgery. 1997 Mar 1;113(3):552-557.
CrossRef









