Ramachandran S1*, Swethanjali D2, Hima Bindu M2, Devaki K2, Ramam Sripada2, Deepak Srinivas E2, Mithun Chakravarthy3 and Dasaratha Dhanaraju M2
1Department of Pharmacology, GIET School of Pharmacy, Rajahmundry, Andhra Pradesh, India.
2Department of Pharmacy Practice, GIET School of Pharmacy, Rajahmundry, Andhra Pradesh, India
3Lalitha Endocare and Skincare Hospital, Rajahmundry, Andhra Pradesh, India.
Corresponding Author Email: ramsnetin@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/2059
Abstract
Aim: To evaluate the drug utilization of antidiabetic, thyroid and antithyroid drugs at an endocrinology speciality hospital among the ambulatory patients. Method: This was a prospective observational study conducted for a period of 6 months. Patients who were diagnosed with either diabetes mellitus (both type-I & type-II) or thyroid disorders and receiving their respective pharmacological therapy irrespective of age and gender were included in this study. Pregnant, lactating women and patients with endocrine problems other than diabetes mellitus and thyroid disorders were excluded from this study. Results: The total number of cases collected and analyzed during a period of 6 months was 246 in which 139 (56.5%) were diabetes mellitus and 107 (43.5%) were thyroid disorders. Among the parenteral hypoglycaemic agents, long acting-insulin glargine and intermediate acting + short acting- NPH + regular insulin were prescribed in almost similar frequency. In case of mono therapy, teneligliptin was the most commonly prescribed medication and this was the unique finding in this study which signified that the trend in prescribing pattern is changing and updating from time to time. In dual combination therapy Glimepiride + Metformin and in triple combination Glimepiride + Metformin + Voglibose combinations were the most commonly prescribed medication. In hypothyroidism, supplementation with levothyroxine was the only treatment alternative as it is related to the underactive thyroid, secreting insufficient amount of hormone. Irrespective of many classes of drugs available in treating hyperthyroidism carbimazole was the most frequently prescribed drug in this study. Conclusion: It was observed that some changes in the prescribing pattern of antidiabetic drugs that signified the trend in drug utilization pattern. Clinical pharmacists should play a key role in observing and identifying the trends in prescribing patterns by performing the drug utilization evaluation studies thereby providing a better pharmaceutical care in collaboration with the other health care professionals.
Keywords
Diabetes; Endocrinology; Teneligliptin; Thyroidism
Download this article as:| Copy the following to cite this article: Ramachandran S, Swethanjali D, Bindu H. M, Sripada R, Srinivas E. D, Chakravarthy M, Dhanaraju M. D. Drug Utilization Evaluation on Antidiabetic, Thyroid and Antithyroid Drugs. Biomed Pharmacol J 2020;13(4). |
| Copy the following to cite this URL: Ramachandran S, Swethanjali D, Bindu H. M, Sripada R, Srinivas E. D, Chakravarthy M, Dhanaraju M. D. Drug Utilization Evaluation on Antidiabetic, Thyroid and Antithyroid Drugs. Biomed Pharmacol J 2020;13(4). Available from: https://bit.ly/36Khjyw |
Introduction
Diabetes mellitus and thyroid dysfunction are the common conditions among the endocrine disorders with potentially devastating health consequences that affect all populations worldwide, which would be a significant health burden to the present society (Ramachandran A et al., 2009). The epidemic status of Diabetes mellitus states that in the year 2018, a total of 406 million people were living with diabetes worldwide. Among them half of the population belong to the three countries that include China [130 million], India [98 million] and US [38 million]. Compared to 2015 WHO statistics of diabetes mellitus, there is a quite increase in the number of population suffering from diabetes mellitus with 19.9% in 2018 which is an important note to be considered. In India, around 5% of the population suffers from diabetes mellitus and 3.4 million deaths are due to the high blood sugar. The International Diabetes Federation assesses that the number of Indians with diabetes mellitus may soar to 336 million by 2030 (Sarah W et al., 2004).
Thyroid disorders are common worldwide. Even in India, there is a significant existence of thyroid disorders. According to a projection from various studies on thyroid disorders, it has been estimated that about 42 million people in India suffer from thyroid disorders. A number of drug formulations are available to handle these health problems successfully and novel approaches are being discovered which is on alarming rise (Khalam A et al., 2012). In view of the above situation, Drug Utilization Evaluation of antidiabetic, thyroid and antithyroid medication in health care settings had a valid significance to evaluate the utility of drugs (Sudha S et al., 2016, Kaisa J et al., 2017, Roland N et al., 2017, Sultana G et al., 2001, Canaris G.J et al., 2000, Upadhay D.K et al., 2007, Gajra B et al., 2011). Drug prescription trend studies of antidiabetic, thyroid and antithyroid drugs can be a powerful exploratory tool to establish treatment guidelines and have an insight about commonly prescribed drugs by the health care providers (Veronesi M et al., 2007, Venturini F et al., 1999).
Drug Utilization Evaluation (DUE) program plays a key role in helping managed healthcare systems understand, interpret, evaluate and improve the prescribing, administration and use of medicines (Abdi S.A.H et al., 2012). It is valuable since the results are used to foster more efficient use of scarce health care resources. Pharmacists play a key role in DUE process because of their expertise in the area of Medication Therapy Management (Satish, K.B.P et al., 2013). Hence in this study, we made an attempt in assessing the drug utilization evaluation of antidiabetic, thyroid and antithyroid drugs at an endocrinology speciality hospital among the ambulatory patients.
Materials and Methods
This was a prospective observational study conducted for a period of 6 months at Lalitha endocare & skin care hospital, Rajahmundry. Patients who were diagnosed with either diabetes mellitus or thyroid disorders and receiving their respective pharmacological therapy irrespective of age and gender were included in this study. Pregnant, lactating women and patients with endocrine problems other than diabetes mellitus and thyroid disorders were excluded from this study. After obtaining the approval from IEC (GSPRJY-IEC/Pharm.D/2018/06), all the necessary and relevant information was collected on a previously designed patient data collection proforma. A total of 256 cases related to the treatment of diabetes mellitus and thyroid disorders were assessed by evaluating the prescriptions from the respective disease conditions.
Results and Discussion
Gender wise categorization of the study population
Table 1 represents gender wise categorization in both diabetes mellitus and thyroid disorders. In this study, a total of 246 cases were considered for Drug Utilization Evaluation of antidiabetic, thyroid and antithyroid drugs. Among them, 139(56.5%) cases were with diabetes mellitus and about 107(43.5%) cases were with thyroid disorders. In case of diabetes, females were more affected when compared to males which was similar to the study done by Gay J Cannaris et al., (1995). Similarly in case of thyroid disorders, females were found to be more prevalent when compared to males in our study.
Table 1: Gender wise categorization of cases with diabetes mellitus and thyroid disorders
| Gender | Male (%) | Female (%) | Total (%) |
| Diabetes | 57(76) | 82(48) | 139(56.5) |
| Thyroid | 18(24) | 89(52) | 107(43.5) |
| TOTAL | 75 (100) | 171 (100) | 246 (100) |
Age wise categorization of patients with diabetes mellitus
Figure 1 represents the age wise categorization of patients with Diabetes Mellitus. Most of the patients were observed in the age group 51-60 years (32.4%) followed by the age group 41-50 years (26.6).
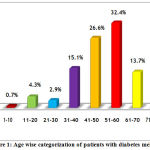 |
Figure 1: Age wise categorization of patients with diabetes mellitus |
Age wise categorization of the patients thyroid disorders
Figure 2 represents the age wise categorization of patients with thyroid disorders. Most of the patients were observed in the age group 21-30 years (27.1%) followed by the age group 31-40 and 41-50 years(20.6% and 20.6%) respectively.
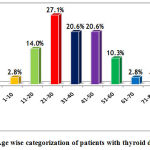 |
Figure 2: Age wise categorization of patients with thyroid disorder |
Study results of the patient population with diabetes mellitus
Co-morbidities observed with diabetes mellitus
In this study, various co-morbidities were clinically observed in the patients with diabetes mellitus. The commonly observed co-morbidities were hypertension 32(30.2%), obesity 9(8.5%), hypothyroid 5(4.7%), hyperthyroid 1 (0.9%) hypertension associated with obesity 22(20.8%), hypertension associated with hypothyroid 8(7.5%), hypothyroid associated with obesity 3(2.9%), hypertension along with obesity and hypothyroid 7(6.6%) and miscellaneous 19(17.9%). Most of the patients were observed with co-morbidity hypertension (30.2%) followed by hypertension associated with obesity (20.8%).
Drug utilization and evaluation of anti-diabetic drugs
In our study, Insulin Glargine (Long acting) 100 IU (48.6%) was most commonly prescribed followed by NPH + Regular Insulin (Intermediate acting + short acting) 30/70 IU (47.4%) among the parenteral hypoglycemic agents. Table 2 represents the commonly prescribed monotherapy in Diabetes Mellitus. In our study, Teneligliptin (50.1%) was the most commonly prescribed antidiabetic drug followed by Metformin 500 mg(12.9%). Table 3 represents the commonly prescribed dual combination therapy in Diabetes Mellitus. In our study, Glimepiride + Metformin (38.2%) was the most commonly prescribed dual combination followed by Teneligliptin + Metformin(34.8%). Table 4 represents the commonly prescribed triple combination therapy in Diabetes Mellitus. In our study, Glimepiride + Metformin + Voglibose (70.4%) was the most commonly prescribed triple combination followed by Glimepiride 1 mg + Metformin 500 mg + Pioglitazone 15 mg (29.6%).
Table 2: Commonly prescribed monotherapy in Diabetes mellitus
| Class of drug | Drugs | Dose | Frequency (%)
(N=54) |
| Sulphonylureas
1 (1.8) |
Gliclazide | 30 mg | 1 (1.8) |
| Meglitinide analogues
1 (1.8) |
Repaglinide | 500 mg | 1 (1.8) |
|
Dipeptidyl peptidase-4-inhibitors 30 (55.5) |
Vidagliptin | 50 mg | 1 (1.8) |
| Saxagliptin | 5 mg | 1 (1.8) | |
| Linagliptin | 5 mg | 1 (1.8) | |
| Teneligliptin | 20mg | 27 (50.1) | |
| Biguanides
11 (20.4) |
Metformin | 500 mg | 7 (12.9) |
| 850 mg | 4 (7.5) | ||
| Thiazolidinediones
2 (3.7) |
Pioglitazone | 15 mg | 2 (3.7) |
| α-glucosidase inhibitors
3 (5.6) |
Voglibose | 0.2 mg | 3 (5.6) |
| Sodium – Glucose Co-Transport inhibitors
6 (11.2) |
Dapagliflozin | 10 mg | 2 (3.7) |
| Canagliflozin | 100 mg | 3 (5.7) | |
| Empagliflozin | 10 mg | 1 (1.8) | |
| TOTAL | 54 (100) | ||
Table 3: Commonly prescribed dual combination therapy in Diabetes mellitus
| DRUG CLASS | DRUGS COMBINATION | FREQUENCY (%) (N=144) |
|
Sulfonylureas + Biguanides 57(39.6) |
Glimepiride + Metformin | 55(38.2) |
| Glipizide + Metformin | 2(1.4) | |
|
Dipeptidyl peptidase-4-inhibitors + Biguanides 67(46.5) |
Vidagliptin + Metformin | 7(4.8) |
| Teneligliptin + Metformin | 50(34.8) | |
| Sitagliptin + Metformin | 10(6.9) | |
|
Thiazolidinediones + Biguanides 3(2) |
Pioglitazone + Metformin | 3(2.0) |
|
α-Glucosidase inhibitors + Biguanides 8(5.6) |
Voglibose + Metformin | 8(5.6) |
|
Sodium-Glucose Co-transport inhibitors + Biguanides 9(6.3) |
Dapagliflozin + Metformin | 9(6.3) |
| TOTAL | 144(100) | |
Table 4: Commonly prescribed triple combination therapy in Diabetes mellitus
| DRUG CLASS | DRUGS COMBINATION | FREQUENCY (%) (N=27) |
| Sulfonylureas + Biguanides + α-Glucosidase inhibitors | Glimepiride + Metformin + Voglibose | 19(70.4) |
| Sulfonylureas + Biguanides + Thiazolidinediones | Glimepiride + Metformin + Pioglitazone | 8(29.6) |
| TOTAL | 27(100) | |
Study results of the patient population with thyroid disorders
Co-morbidities observed with thyroid disorders
Different co-morbidities were associated with thyroid disordered patients. Hypothyroid patient with hypertension were 2(8.3%), obesity were 7(29.2%), anaemia were 3(12.5%), hypertension along with obesity were 4(16.6%) and miscellaneous were 8(33.4%). While in hyperthyroid patients, hypertension was the only associated co-morbid condition found in our study. Most of the hypothyroid patients were observed with the co-morbidity obesity (29.2%) followed by HTN associated with obesity (16.6%).
Drug utilization and evaluation of thyroid and anti-thyroid drugs
Levothyroxine therapy is the usual treatment in hypothyroidism. In our study, Levothyroxine 75mcg (18.1%) was the most commonly prescribed dose followed by Levothyroxine 50mcg (15.7%). In case of anti-thyroid therapy in hyperthyroidism, carbimazole (96%) was most frequently prescribed dose followed by Methimazole (4%) in our study.
Conclusion
Majority of the Diabetes Mellitus cases were observed in the age group of 51-60 years and thyroid disorders were observed in the age group of 21-30 years. Hypertension and obesity were the most commonly associated co-morbidities found in diabetes mellitus patients, obesity with respect to hypothyroidism and hypertension with respect to hyperthyroidism were the most commonly associated co-morbidities found in thyroid disordered patients. With regard to body mass index, obese patients were of the highest proportion in diabetes mellitus which indicates that they require proper life style modifications which would be a great tool in improving their health outcomes. Among the parenteral hypoglycaemic agents, long acting-insulin glargine and intermediate acting + short acting- NPH + regular insulin were prescribed in almost similar frequency. In mono therapyteneligliptin was the most commonly prescribed medication. This was the unique finding in the present study which signified that the trend in prescribing pattern is changing and updating from time to time. In dual combination therapy Glimepiride + Metformin and in triple combination Glimepiride + Metformin + Voglibose combinations were the most commonly prescribed medication.In hypothyroidism, supplementation with levothyroxine was the only treatment alternative as it is related to the underactive thyroid, secreting insufficient amount of hormone. Since this is a known fact, an attempt was made to know the routinely prescribed doses, it was found that 50 mcg next to 75 mcg were of greatest measure. Irrespective of many classes of drugs available in treating hyperthyroidism carbimazole was the most frequently prescribed drug in this study. Clinical pharmacists should play a key role in observing and identifying the trends in prescribing patterns by performing the drug utilization evaluation studies thereby providing a better pharmaceutical care in collaboration with other health care professionals.
Acknowledgments
Authors wish to acknowledge the management of GIET School of Pharmacy for providing necessary facilities and also thank the staff of Lalitha Endocare & Skincare Hospital, Rajahmundry, Andhra Pradesh, India for their kind support.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Source
No funding source was involved.
References
- Abdi S.A.H, Churi S and Ravi Y. Study of drug utilization pattern of antihyperglycemic agents in a South Indian tertiary care teaching hospital. Indian Journal of Pharmacology, 2012; 44: 210-214.
CrossRef - Canaris G.J, Manowitz N.R, Mayor G and Ridgway E. The Colorado Thyroid Disease Prevalence Study. Arch Intern Med.,2000; 160: 526–534.
CrossRef - Gajra B, Adhikari A.K, Vidyasagar G, Rathore D.S and Bhakti G. Drug utilization review of antidiabetic drugs in patients of a tertiary care hospital of India. The Indian Journal of Hospital Pharmacy, 2011; 48: 32-34.
- Kaisa J and Lipska X. Trends in drug utilization, glycemic control, and rates of severe hypoglycemia. Diabetes Care, 2017; 40: 468-475.
CrossRef - Khalam A, Dilip C and Shinu C. Drug use evaluation of diabetes mellitus in hospitalized patients of a tertiary care referral hospital. J Basic Clin Physiol Pharmacol, 2012; 23: 173-177.
CrossRef - Ramachandran A and Snehalatha C. Current scenario of diabetes in India. Journal of diabetes, 2009; 1: 18-28.
CrossRef - Roland N and Chijioke N. Utilization study of antidiabetes medicines at a tertiary care hospital in Nigeria. Future Journal of Pharmaceutical Sciences, 2017; 4: 109-115.
CrossRef - Sarah W and Gojka R. Global prevalence of diabetes estimates for the year 2000 and projections for 2030. Diabetes care, 2004; 27; 1047-1053.
CrossRef - Satish K.B.P, Prasanna D, Rajesh V and Prashant C. Assessment of clinical pharmacist intervention in tertiary care teaching hospital of Southern India. Asian J Pharm Clin Res., 2013; 6: 258-261.
- Sudha S and Vishal R. Prescribing Pattern of Oral Hypoglycaemic Drugs, Rationality and Adherence to American Diabetes Association (ADA) Treatment Guidelines among Type 2 Diabetes Mellitus (T2DM) Postmenopausal Women. Journal of Clinical Diagnostic Research, 2016; 10: 11-15.
- Sultana G and Kapur P. Drug utilization of oral hypoglycemic agents in university teaching hospital in India. J Clin Pharm Ther., 2001; 35: 267-277.
CrossRef - Upadhay D.K and Palaian S. Prescribing Pattern in Diabetic Outpatients in a tertiary Care Teaching hospital in Nepal. Journal of Clinical and Diagnostic Research, 2007; 1: 248-245.
- Venturini F, Nichol M.B, Sung J.C.Y, Bailey K.L, Cody M and McCombs J. Compliance with sulfonylureas in a health maintenance organization: A pharmacy record-base study. Ann Pharmacother, 1999; 33: 281-288.
CrossRef - Veronesi M, Cicero A and Prandin M. A prospective evaluation of persistence on antihypertensive treatment with different antihypertensive drugs in clinical practice. Vascular Health and Risk Management, 2007; 3: 999-1005.








