Eko Fuji Ariyanto1* and Muhammad Hasan Bashari2
and Muhammad Hasan Bashari2
1Division of Biochemistry and Molecular Biology, Department of Biomedical Sciences, Faculty of Medicine, Universitas Padjadjaran, Jl. Raya Bandung Sumedang, KM. 21, Sumedang, Indonesia, 45363.
2Division of Pharmacology and Therapy, Department of Biomedical Sciences, Faculty of Medicine, Universitas Padjadjaran, Jl. Raya Bandung Sumedang, KM. 21, Sumedang, Indonesia, 45363.
Corresponding Author E-mail: fuji@unpad.ac.id
DOI : https://dx.doi.org/10.13005/bpj/2055
Abstract
Coronavirus disease 2019 (COVID-19) is the current biggest health problem that has caused pandemic in hundreds of countries worldwide. Important efforts for COVID-19 prevention and management have been implemented by WHO and many countries; however, the number of new cases is still increasing. The objective of this review is to formulate appropriate strategies to tackle COVID-19 pandemic using molecular mechanisms-based approach. COVID-19 preventive measures aim to avoid virus entry to human cells by applying physical distancing, hand washing and personal protective equipment, maintaining good immune system by balanced nutrition and physical exercise, developing vaccine against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) based on comprehensive analysis on SARS-CoV-2 antigen presentation and subsequent immunological cascades, considering the patients’ clinical condition including biomolecular parameters, and developing drugs by designing inhibitors for SARS-CoV-2 proteins responsible for virus replication and transcription.
Keywords
COVID-19; Molecular Approach; SARS-CoV-2; Strategy Formulation
Download this article as:| Copy the following to cite this article: Ariyanto E. F, Bashari M. H. Formulating Strategies to Tackle COVID-19 Pandemic by Understanding its Molecular Mechanisms: A Review. Biomed Pharmacol J 2020;13(4). |
| Copy the following to cite this URL: Ariyanto E. F, Bashari M. H. Formulating Strategies to Tackle COVID-19 Pandemic by Understanding its Molecular Mechanisms: A Review. Biomed Pharmacol J 2020;13(4). Available from: https://bit.ly/3kODeJG |
Introduction
Coronavirus disease 2019 (COVID-19) is the current biggest health problem that has caused pandemic in hundreds of countries worldwide very rapidly. As April 20, 2020, the World Health Organization (WHO) reported that the number of confirmed COVID-19 cases globally was 2,314,621 with mortality rate 6.8%.1 Three countries with the highest number of cases were the United States of America (723,605 cases with 34,203 deaths), Italy (178,972 cases with 23,660 deaths) and Spain (195,944 cases with 20,453 deaths).1 COVID-19 was caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and, firstly became an outbreak in Wuhan, China, in December 2019.2 In addition to very serious health problems, this pandemic potentially causes more systemic effect including economic and social crisis.
Some important efforts to tackle COVID-19 have been conducted by WHO and many countries; however, the number of new cases is still increasing. This review aims to formulate appropriate strategies to tackle COVID-19 pandemic using molecular mechanisms-based approach.
Clinical Manifestation of COVID-19
An epidemiological study involving 99 COVID-19 patients in Wuhan, China, reported that the symptoms present in COVID-19 patients were fever, cough, shortness of breath, myalgia, confusion, headache, sore throat, rhinorrhea, chest pain, diarrhea, and nausea and vomiting.3 In line with this study, another study in Wuhan also revealed that, in the early onset of illness, COVID-19 patients were reported to suffer from fever, cough, muscle ache.2 Some patients also complained of sputum production, headache, hemoptysis or diarrhea.2 As the disease developed, patients had dyspnea, lymphopenia and radiographic finding of pneumonia, and, subsequently, might have acute respiratory distress syndrome and multiple organ failure as the complications and died.2-3
Recent retrospective cohort study which involved 191 COVID-19 patients in Wuhan, China reported that almost half of the patients had disease comorbidity, such as hypertension, diabetes and coronary heart disease.4 Furthermore, this study revealed that older age, high Sequential Organ Failure Assessment (SOFA) and higher d-dimer level were associated with higher odds of in-hospital mortality.4 Moreover, an estimation study using model-based analysis unraveled that COVID-19 case fatality ratio dramatically increased in patients aged >60 years.5
Molecular Mechanisms Underlying the Pathogenesis of COVID-19
Spike (S) protein of coronavirus, including those which causes severe acute respiratory syndrome (SARS), was reported to be responsible for virus entry into host cells.6 The mechanism of infection by coronavirus involved the binding of S protein with angiotensin-converting enzyme 2 (ACE2) receptor of the target cell.7 Recent study unraveled that SARS-CoV-2, which caused COVID-19, also binds to ACE2 receptor to initiate the infection.8 Another study reported the role of Mpro, an important CoV enzyme which facilitates viral replication and replication in host cells.9
Antigen presentation is a very important virus entry-following step in the process of infection. Viral antigens are presented by major histocompatibility complex (MHC) or human leukocyte antigen (HLA) in humans and recognized by cytotoxic T lymphocytes which then lead to subsequent immunological cascades. Previous studies reported that HLA polymorphisms were associated with human susceptibility to get severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV).10 Although at this moment we still do not know exactly about the mechanism of SARS-CoV-2 antigen presentation, these reports might give us some clues to optimize our prevention, diagnosis and management on COVID-19.
Investigation on a family cluster infected with SARS-CoV-2 in China found lymphopenia as one of the clinical characteristics of COVID-19 patients.11 Moreover, a recent case report of a severe COVID-19 patient who had a history of travelling to Wuhan, China, revealed that the number of CD4+ and CD8+ T lymphocytes were reduced.12 Further analysis on COVID-19 molecular mechanisms using transcriptome sequencing of bronchoalveolar lavage fluid (BALF) and peripheral blood mononuclear cells (PBMC) revealed the association between increased production of chemokines including CCL2/MCP-1, CXCL10/IP-10, CCL3/MIP-1A, and CCL4/MIP1B with the pathogenesis of COVID-19.13 This study also proposed the induction of P53 signaling pathway and apoptosis as the mechanisms by which lymphopenia commonly occurs in COVID-19 patients.13 Furthermore, recent study suggested the occurrence of cytokine storms in the pathogenesis of COVID-19, starting from the lungs and then circulating to other organs.14 In normal persons, the released inflammatory cytokines will subsequently recruit virus-specific T cells to the infection site in which they remove the infected cells before the spreading of the virus. On the other hand, neutralizing antibodies will prevent further viral infection by attracting alveolar macrophages to phagocytize the infected cells. While in COVID-19 patients, the inflammatory cascades might cause further recruitment of immune cells in the lungs, which, in turn, results in the lungs destruction due to oversecretion of cytokines.14
Strategies to Tackle COVID-19
Viral infection involves three major factors: (1) viral factors, including pathogenicity, transmission and virulence; (2) host factors, consisting of age, lifestyle, immune condition and comorbid diseases; and (3) external factors such as environmental condition, community lifestyle, pharmaceutical and non-pharmaceutical interventions.15 These factors can influence the severity and transmissibility of viral infection.15
The most effective strategy to control COVID-19 is to prevent the virus entry to human cells by implementing physical distancing as recommended by WHO for all affected countries.1 Physical distancing is required to prevent transmission of virus through person-to-person contact, as evidence also reported that COVID-19 can be transmitted from person-to-person.11 WHO recommends keeping distance at least 2 meters with other people as previous study revealed that infectious influenza virus-containing aerosols might be exposed by influenza patients to another person within 1.829 meters.1,16 Moreover, it was estimated that 107 countries implemented school closure to improve the prevention measures, even though a study reported that it only reduced mortality rate 2-4%.17-18 Some countries also implement “lockdown” in public activities including flight restrictions, as, for example, conducted in Turkey.19
Personal protective equipment measures such as wearing appropriate type of masks and regular hand washing with soap or usage of >60% alcohol-based hand sanitizer are also important to prevent SARS-CoV-2 infection. Soap molecules contain surfactants which facilitate removal of microorganisms including virus.20 They have hydrophilic part which dissolves water in one side, and, on the other side, have hydrophobic part which can dissolve fatty layer of virus envelope. Ethanol in hand sanitizer destroys virus by coagulation and denaturation of virus protein structures.21
As immunological response is very important to tackle coronavirus infection, maintaining well functional immunity including good diet with balanced composition of carbohydrates, proteins, lipids, vitamins and minerals and exercise, is the other main strategy. Every cell, including immune cells, requires energy, which is obtained from food, for maintaining their cellular functions. Various cytokines and antibodies are also composed of amino acids whose productions require sufficient protein intake. Previous studies revealed the role of vitamins and minerals, such as vitamin A, beta-carotene, folic acid, vitamin B6, vitamin B12, vitamin C, vitamin E, riboflavin, iron, zinc, and selenium, in the variety of immune functions.22 They support the functions of NK cells, macrophages and T cells, and maintain antibodies and cytokines production.22 Regular exercise of moderate intensity was reported to have several benefits for immune systems, such as increasing the function of neutrophil, T cells and NK cells.23 Regular physical exercise also exerts anti-inflammatory effects through multiple pathways and improves immune system regulation, hence decreases the risk of getting illness including infection.24
Rapid diagnostic test is the other important measure to control the outbreak of COVID-19.1 Hundreds of countries gave big efforts in facilitating this program. Korea transformed the implementation of rapid diagnostic tests by running Drive-through Screening Center for COVID-19 by which the test only took about 10 minutes and the testees did not need to leave their car while being tested. This program increased testing capacity in Korea.25
As COVID-19 severity is correlated with disease comorbidity, it is also important to consider the patients’ clinical condition comprehensively. Clinicians as the first liner in COVID-19 diagnosis and management play pivotal roles in determining the prognosis of COVID-19 by taking some indicators, such as disease comorbidity, age, SOFA and d-dimer level, into account.4 Considering the role of disease comorbidity in COVID-19 severity, community-based promotive and preventive programs for prevention of hypertension, diabetes and other metabolic diseases are indispensable.
The presence transcriptome data of COVID-19 patients is very important to guide us finding the best management for these patients. Careful analysis on these data might also give us valuable clues in developing new drugs and vaccines for SARS-CoV-2. Molecular approach is very important in developing new drugs specific for SARS-CoV-2 control. Recent study reported that drug development has been initiated by discovering the inhibitor for Mpro, a CoV enzyme responsible for virus replication and transcription.9 Other possible targets for vaccines and drug developments are blocking of S protein, which is responsible for interaction with host cells’ ACE2 receptor, inhibition of TMPRSS2, a serine protease which plays pivotal role in the cleavage of S protein for viral entry, activation of CD8+ T cell to remove infected cells by degranulation, and neutralization of pro-inflammatory cytokines to recover cytokine storm.14 Finally, vaccines for SARS-CoV-2 are very urgent to develop body immunity against this virus. Vaccine development might be initiated using a molecular approach based on comprehensive analysis on SARS-CoV-2 antigen presentation and subsequent immunological cascades.
Comprehensive strategies for COVID-19 prevention and management are illustrated in Figure 1.
Figure 1: Comprehensive strategies for COVID-19 prevention and management.1,4,9,14,15,16,22,23,24 PPE: personal protective equipment.
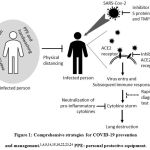 |
Figure 1: Comprehensive strategies for COVID-19 prevention and management.1,4,9,14,15,16,22,23,24 PPE: personal protective equipment. |
Conclusion
Comprehensive strategies are required to tackle COVID-19 pandemic. They include preventive measures to avoid virus entry into human cells, balanced nutrition and physical exercise to maintain good immune system, analysis of biomolecular parameters to determine disease severity and prognosis, and vaccine and drug development against SARS-CoV-2. Molecular approach in formulating the strategies is important to produce precise and effective measure to this pandemic.
Acknowledgement
This work is funded by Universitas Padjadjaran grant Number 1733/UN6.3.1/LT/2020 for MHB.
Conflict of Interest
The authors declare no conflict of interests in this work.
References
- Coronavirus disease 2019 (COVID-19) situation report – 91. April 20, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200420-sitrep-91-covid-19.pdf?sfvrsn=fcf0670b_4 (Accessed on April 21, 2020).
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet., 2020; 395: 497–506.
CrossRef - Chen N, Zhou M, Dong X, Qu J, Gong F, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet., 2020; 395: 507–513.
CrossRef - Zhou F, Yu T, Du R, Fan G, Liu Y, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet., 2020; 395: 1054–1062.
CrossRef - Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis., 2020; 20(6): 669–677.
CrossRef - de Wit E, van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: Recent Insights Into Emerging Coronaviruses. Nat Rev Microbiol., 2016; 14(8): 523–534.
CrossRef - Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature., 2003; 426: 450–454.
CrossRef - Zhou P, Yang XL, Wang XG, Hu B, Zhan L, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature., 2020; 579: 270–273.
- Jin Z, Du X, Xu Y, Deng Y, Liu M, et al. Structure of Mpro from COVID-19 virus and discovery of its inhibitors. Nature., 2020; 582(7811): 289–293.
CrossRef - Li X, Geng M, Peng Y, Meng L, Lu S. Molecular Immune Pathogenesis and Diagnosis of COVID-19. J Pharm Anal., 2020; 10(2): 102–108.
CrossRef - Chan JFW, Yuan S, Kok KH, To KKW, Chu H, et al. A Familial Cluster of Pneumonia Associated With the 2019 Novel Coronavirus Indicating Person-To-Person Transmission: A Study of a Family Cluster. Lancet., 2020; 395(10223): 514–523.
CrossRef - Xu Z, Shi L, Wang Y, Zhang J, Huang L, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med., 2020; 8: 420–422.
CrossRef - Xiong Y, Liu Y, Cao L, Wang D, Guo M, et al. Transcriptomic characteristics of bronchoalveolar lavage fluid and peripheral blood mononuclear cells in COVID-19 patients. Emerging Microbes & Infections., 2020; 9(1): 761–770.
CrossRef - Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The Trinity of COVID-19: Immunity, Inflammation and Intervention. Nat Rev Immunol., 2020; 20(6): 363–374.
CrossRef - Short KR, Kedzierska K and van deSandt CE. Back to the Future: Lessons Learned From the 1918 Influenza Pandemic. Front. Cell. Infect. Microbiol., 2018; 8: 343.
CrossRef - Bischoff WE, Swett K, Leng I, Peters TR. Exposure to Influenza Virus Aerosols During Routine Patient Care. J Infect Dis., 2013; 207(7): 1037–10.
CrossRef - United Nations Educational, Scientific and Cultural Organization (UNESCO). COVID-19 educational disruption and response. 2020. https://en. unesco.org/themes/education-emergencies/coronavirus-schoolclosures (Accessed on March 19, 2020).
- Viner RM, Russell SJ, Croker H, Packer J, Ward J, et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health., 2020; 4(5): 397–404.
CrossRef - Demirbilek Y, Pehlivantürk G, Özgüler ZÖ, Meşe COVID-19 Outbreak Control, Example of Ministry of Health of Turkey. Turk J Med Sci., 2020; 50(SI-1): 489–494.
CrossRef - Chaudhary NK, Bhattarai A, Guragain B, Bhattarai A. Conductivity, Surface Tension, and Comparative Antibacterial Efficacy Study of Different Brands of Soaps of Nepal. Journal of Chemistry., 2020; 2020: 1–13.
CrossRef - Yoo JH. Review of Disinfection and Sterilization – Back to the Basics. Infect Chemother., 2018; 50(2): 101–109.
CrossRef - Saghazadeh A, Mahmoudi M, Rezaei N. Nutrition and Immunity. Cham: Springer; 2019.
CrossRef - Alack K, Pilat C, Kruger K. Current Knowledge and New Challenges in Exercise Immunology. Dtsch Z Sportmed., 2019; 70: 250–2.
CrossRef - Nieman DC, Wentz LM. The Compelling Link Between Physical Activity and Body’s Defense System. Journal of Sport and Health Science., 2019; 8(3): 201–217.
CrossRef - Kwon KT, Ko JH, Shin H, Sung M, Kim JY. Drive-Through Screening Center for COVID-19: a Safe and Efficient Screening System against Massive Community Outbreak. J Korean Med Sci., 2020; 35(11): e123.
CrossRef








