Sunil Kumar Patanaik1 , Chaitali Pattanayak2*
, Chaitali Pattanayak2* , Vartika Srivastava2
, Vartika Srivastava2 and Sougata Sarkar3
and Sougata Sarkar3
1Department of Surgery, Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar, India
2Department of Pharmacology, Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar, India.
3Dept of Clinical and Experimental Pharmacology, School of tropical medicine, Kolkata, India.
Corresponding author E-mail: chaitali.pattanayak@kims.ac.in
DOI : https://dx.doi.org/10.13005/bpj/2031
Abstract
Intestinal obstruction is one of the commonest surgical emergencies in all age groups. The diagnosis of intestinal obstruction at times poses a difficult problem, especially in those patients who present as subacute intestinal obstruction (SAIO) with atypical features due to which the diagnosis is delayed. SAIO implies incomplete obstruction. Intermittent nature of symptoms and signs delays diagnosis as well as definitive treatment. This study was undertaken to determine the possible clinical profile of this difficult and confusing entity. 57 patients above 10 years of age presenting with subacute intestinal obstruction were studied from July 2018 to December 2019 in a multispeciality hospital in eastern part of India. Patients with acute intestinal obstruction and bowel strangulation were excluded from this study. Males were more affected than the females. Abdominal pain was the commonest symptom seen in 51 (89.4%) patients, followed by non-passage of faeces / flatus in 45 patients (78.9%) and vomiting seen in 39 (68.4%) patients. About 28 patients (49.1%) had undergone previous abdominal surgery, out of which 25 patients were operated for laparotomy. Out of the 57 patients, surgery was needed to relieve obstruction in 18 (31.6%) patients, the remaining 39 patients (68.4%) were managed conservatively. Most commonly performed procedure was adhesiolysis in 12 patients. Subacute intestinal obstruction continues to be one of the most common abdominal problems faced by general surgeons. Early clinical recognition, diagnostic tools and timely management are extremely important in diagnosing this clinical entity, thereby reducing mortality and long-term morbidity.
Keywords
Adhesions; Strictures; Subacute Intestinal Obstruction
Download this article as:| Copy the following to cite this article: Patanaik S. K, Pattanayak C, Srivastava V, Sarkar S. Clinical Profile and Outcome of Subacute Intestinal Obstruction: A Hospital Based Prospective Observational Study. Biomed Pharmacol J 2020;13(3). |
| Copy the following to cite this URL: Patanaik S. K, Pattanayak C, Srivastava V, Sarkar S. Clinical Profile and Outcome of Subacute Intestinal Obstruction: A Hospital Based Prospective Observational Study. Biomed Pharmacol J 2020;13(3). Available from: https://bit.ly/35axi7o |
Introduction
Intestinal obstruction is one of the most commonly encountered surgical entities in all age groups, which accounts for approximately 15 percent of patients visiting the emergency department with complaints of acute pain in the abdomen1. Even Ebers Papyrus (1550 BC) and Hippocrates have documented cases of bowel obstruction.
The mode of presentation varies with underlying aetiology. The complications associated with intestinal obstruction are sepsis, bowel ischemia and perforation. There is significant decline in the morbidity and mortality associated with intestinal obstruction because of enhanced knowledge regarding pathophysiology, improvement of radiological techniques and better approach towards correction of fluid and electrolyte imbalance, administration of antibiotics for controlling bacterial infections, nasogastric decompression and various newer surgical techniques, yet it is a challenge to manage the condition effectively2. The diagnosis of intestinal obstruction at times poses a difficult problem, especially in those patients who present as subacute intestinal obstruction (SAIO) with atypical features due to which the diagnosis is delayed. Hence, it is important for the treating physicians to weigh the risks of surgery with the drawbacks of initial conservative management3.
SAIO implies incomplete obstruction4. It has been defined in a number of ways and there are many confusions in the treatment protocols. It is characterized by onset of symptoms like colicky abdominal pain, vomiting, and abdominal distension along with continued passage of flatus and/or faeces beyond 6-12 hrs. The patient usually presents with recurrent and intermittent intestinal obstruction, the patient being well in between4. SAIO may get relieved within few hours spontaneously/after conservative management or may progress to acute obstruction. Intermittent nature of symptoms and signs delays diagnosis as well as definitive treatment and the patients often suffer for weeks and months before appropriate treatment is instituted. The intestinal obstruction can be of small intestine or large intestine.
| Common causes of Intestinal obstruction | Uncommon causes of Intestinal obstruction |
| Adhesions and bands following abdominal surgery | Fecal impaction |
| External Hernia | Pseudoobstruction |
| Intussusceptions | colon atresia |
| Volvulus | Fecaloma |
| Neoplasms (benign or malignant) | Endometriosis |
| Strictures (IBD) | Intestinal worms (Ascariasis) |
Small bowel obstructions are commonly due to adhesions and hernias while large bowel obstructions are frequently due to tumors and volvulus5. The diagnosis can be done on plain X-rays; however, CT scan is more accurate. Ultrasound or MRI may be helpful in the diagnosis of children or pregnant women.
The condition may be managed conservatively or with surgery. Usually intravenous fluids are given, a nasogastric tube is administered to decompress the intestines, and analgesics are given, often accompanied with antibiotics. Complications like sepsis, bowel ischemia and bowel perforation may occur6.
Since there are very few studies and insufficient information regarding the causes, course and subsequent management of the cases presenting with features of subacute intestinal obstruction (SAIO), this study was undertaken to determine the possible clinical profile of this difficult and confusing entity.
Aims and Objective
To study the demographic profile of patients admitted with SAIO in our setup
To evaluate the various etiological factors of SAIO
To study the clinical features of patients presenting with SAIO
To study the importance of investigations in diagnosis of SAIO
To study the outcome of management (conservative / surgery) of the cases
Materials and Methods
We conducted a prospective observational study in which a total number of 57 cases of SAIO were studied from July 2018 to December 2019 in a multispeciality hospital in Eastern India.
Inclusion Criteria
All the patients presenting to the surgery OPD or the emergency department with the following features of SAIO were identified and included in the study:-
Patients > 10 years of age
Patients who continue to pass faeces/ flatus even after 12 hours of starting of the symptoms
Much lesser extent of abdominal distension with or without tenderness
No guarding, no rigidity
Bowel sounds sluggish or absent
Plain X-ray abdomen showing gas distended bowel loops/fluid filled bowel loops/multiple air fluid levels
Patients in whom non operative management was decided based on clinical and radiological evaluation
Exclusion criteria
Patients < 10 years of age
Patients presenting with acute intestinal obstruction, in whom operative treatment was planned following clinical and radiological evaluation
Patients presenting with signs of bowel strangulation
The demographic profile of the patients was recorded. The history of the patients was taken which included duration of symptoms, the presenting complaints, namely the type of pain, vomiting, passage of faeces and/or flatus, abdominal distension, number of previous attacks in the patients, previous treatment / surgery and presence of any co-morbid condition.
A detailed clinical examination including rectal examination of the patient was done and the findings which included fever, tachycardia, abdominal signs like distension, tenderness, rigidity, guarding, bowel sounds, presence of visible/palpable bowel loops, presence of any lumps were noted. Investigations included haemogram, biochemical parameters, plain X-ray of abdomen in erect and supine posture, ultrasonography of abdomen, CT abdomen (if necessary) and the findings were recorded.
Following a provisional diagnosis of SAIO, the patients were initially managed conservatively by withholding oral intake, aspiration of gastrointestinal secretions, administration of intravenous fluids and correction of electrolyte imbalance. The patients were observed for features of relief of obstruction like reduction in vomiting, pain score, and passage of faeces / flatus, reduction in tenderness and abdominal girth; the disappearance of visible/palpable bowel loops; and reduction in nasogastric tube output. The patients were monitored regularly for the development of signs of strangulation like tachycardia, fever, abdominal tenderness, etc. If the patient developed signs of strangulation, the patient was operated on emergency basis. If the patient did not get relieved conservatively within 24-48 hours of observation, exploratory laparotomy was performed.
The patients who got relieved within few hours of conservative treatment were further investigated if there was a history of recurrent similar attacks or if patient developed recurrent symptoms. Ultrasound of the abdomen and pelvis, CT scan abdomen, laparoscopy were undertaken in a sequential order to look for findings suggestive of intestinal obstruction and specific signs which suggest cause of obstruction. In case the investigation provided sufficient information to confirm the diagnosis of a lesion explaining the symptoms of SAIO in the patient, appropriate operative intervention was undertaken. When laparoscopy demonstrated any lesion, it was tackled under the same anaesthesia either laparoscopically or by exploratory laparotomy.
Results
A clinical study of 57 patients of subacute intestinal obstruction (SAIO) was done for a period of 18 months. It was done in patients above 10 years of age, the age distribution is shown in Table 1 . The mean age of presentation was 51.9 years. Patients of SAIO were mainly from the age group 51-60 years (21%). Occurrence of SAIO was common in males [36 in number (63%)] as compared to females [21 in number (37%)] as shown in Figure 1. A total number of 36 patients presented with a history of previous attacks in the past out of which 16 patients (44.4%) and 10 patients (27.7%) had one and two such previous attacks respectively, Table 2.
| Age distribution of patients | ||
| Age interval (years) | Number of patients | Percentage (%) |
| 10-20 | 3 | 5.3 |
| 21-30 | 6 | 10.6 |
| 31-40 | 8 | 14 |
| 41-50 | 8 | 14 |
| 51-60 | 12 | 21 |
| 61-70 | 7 | 12.2 |
| 71-80 | 7 | 12.2 |
| >80 | 6 | 10.6 |
| Total | 57 | 100 |
Table 1: Age distribution of patients
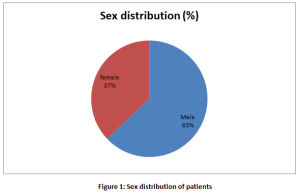 |
Figure 1: Sex distribution of patients. |
| Number of previous attacks | Number of patients | Percentage (%) |
| One | 16 | 44.4 |
| Two | 10 | 27.7 |
| Three | 7 | 19.4 |
| > Four | 3 | 8.3 |
| Total | 36 | 100 |
Table 2: Number of previous attacks in patients
The present study on SAIO showed that abdominal pain was the commonest symptom seen in 51 (89.4%) patients, followed by non-passage of faeces / flatus in 45 patients (78.9%) and vomiting seen in 39 (68.4%) patients (some patients presented with multiple symptoms), Table 3. Most of the patients ( 57.9%) presented with a history of duration of symptoms of 4-6 days as shown in Figure 2, followed by 29.8% patients with a duration of 1-3 days and 12.3% with a duration of more than 6 days.
| Symptoms | Number of Patients | Percentage (%) |
| Abdominal Pain | 51 | 89.4 |
| – Colicky | 28 | – 49.1 |
| – Continuous | 23 | – 40.3 |
| Non- passage of faeces or flatus | 45 | 78.9 |
| Vomiting | 39 | 68.4 |
| Distension of abdomen | 36 | 63.1 |
Table 3: Distribution of symptoms in patients
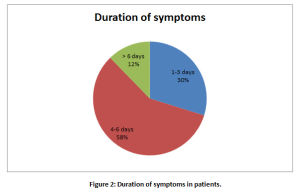 |
Figure 2: Duration of symptoms in patients |
About 28 patients (49.1%) had undergone previous abdominal surgery, out of which 25 patients were operated for laparotomy – gynaecological procedures being commonest (8 patients) and 3 patients underwent laparoscopic procedures in the past, as seen in Table 4.
| Types of surgery | Number of patients |
| Laparotomy | 25 |
| -Gynaecological procedure | – 8 |
| -Abdominal Trauma | – 7 |
| -Intestinal obstruction | – 4 |
| -Appendectomy | – 3 |
| -Cholecystectomy | – 3 |
| Laparoscopic Procedure | 3 |
Table 4: Previous abdominal surgery in 28 patients
On examination of the patients, the most common physical finding was abdominal tenderness found in 46 ( 80.7%) patients, followed by distension in 35 ( 61.4%) patients as shown in Table 5.
| Findings | Number of patients | Percentage |
| Abdominal tenderness | 46 | 80.7 |
| Distension of abdomen | 35 | 61.4 |
| Exaggerated bowel sounds | 27 | 47.4 |
| Decreased/absent sounds | 18 | 31.6 |
| Visible/palpable bowel loops | 9 | 15.8 |
| Lump abdomen | 3 | 5.2 |
Table 5: Physical Findings in patients
Out of the plain X-Ray films of 57 patients, a total of 41 showed positive findings. 36 patients had gaseous distension of bowel loops, 7 patients had fluid filled loops and 5 patients had multiple air fluid levels on erect film (7 patients had more than one finding) as shown in Table 6, Ultrasonography of abdomen was required in 53 ( 92.9% ) patients. It showed abnormal findings in 49 (85.9%) patients and was normal in 4 (7.1%) patients. Dilated bowel loops was the most frequent finding seen in 27 (47.3%) patients, Table 7. Ileal strictures were noticed by ultrasonography in previously diagnosed cases of inflammatory bowel disease (IBD). CT scan was required to be performed in 25 ( 43.8%) patients where the commonest finding was dilated bowel loops as shown in Table 8.
| X-ray findings | Number Of Patients |
| Gaseous distension of bowel loops | 36 |
| Dilated fluid filled bowel loops | 7 |
| Multiple air fluid levels | 5 |
| Total | 41 (7 patients had >one finding) |
Table 6: X-ray findings in patients
| Findings | Number of Patients |
| Dilated bowel loops | 27 |
| Free fluid in abdomen | 7 |
| Ileal stricture (IBD) | 6 |
| Mesentric lymphadenopathy | 3 |
| Contracted pulled up caecum | 3 |
| Herniation of contents | 3 |
| Total | 49 |
Table 7: USG findings in patients
| CT findings | Number of patients |
| Dilated bowel loops | 7 |
| Bowel thickenings | 6 |
| Stricture (IBD) | 6 |
| Ileo-caecal Tuberculosis | 3 |
| Herniation of contents | 3 |
| Total | 25 |
Table 8: CT findings in patients
Out of the 57 patients of SAIO, surgery was needed to relieve obstruction in 18 (31.6%) patients, the remaining 39 patients ( 68.4%) were relieved of the symptoms on being managed conservatively, Figure 3. The most commonly performed surgical procedure was adhesiolysis in 12 patients, Table 9.
| Surgical Procedure | Number of Patients |
| Adhesiolysis | 12 |
| Resection and anastamosis of bowel | 3 |
| Stricturoplasty | 2 |
| Inguinal exploration and herniorraphy | 1 |
| Total | 18 |
Table 9: Surgeries performed in patients
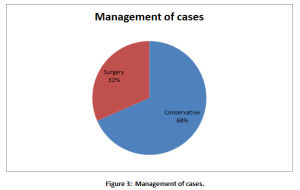 |
Figure 3: Management of cases. |
After doing the investigations like radiography, ultrasonography, CT scan and performing surgery in the required cases of SAIO, the causes of intestinal obstruction were determined in 40 patients. The commonest cause of intestinal obstruction in the study group was found to be due to adhesions in 21 patients (52.5%) followed by small intestinal strictures due to IBD in 6 patients ( 15%) as depicted in Table 10.
| Causes | Number of Patients | Percentage |
| Adhesions | 21 | 52.5 |
| Small intestinal strictures (IBD) | 6 | 15 |
| Hernia(Inguinal, Incisional) | 5 | 12.5 |
| Tubercular | 5 | 12.5 |
| Carcinoma | 3 | 7.5 |
| Total | 40 |
Table 10: Causes of intestinal obstruction
Discussion
Sub-acute intestinal obstruction (SAIO) is an enigma. It is one of the important causes of morbidity in day to day surgical practice. This is especially true for patients who present with atypical features, thus causing delayed diagnosis7.
In the present clinical study, which has excluded children less than 10 years of age, the peak incidence is seen in the 51-60 years age group (21%), and mean age of presentation is 51.9 years, which is more as compared to the study by Ojha et al, where the mean age of presentation with SAIO was 31.8 years. Both males and females are equally affected and the condition can occur at any age8, but our study shows that the males (63%) are more affected as compared to the females (37%), male : female ratio being 1.7:1, which is almost similar to the study by Ojha A et al where the ratio was 1.5:14.
Most of the patients (57.9%) presented within 4-6 days of onset of symptoms. About 36 out of 57 patients had recurrent symptoms, with 16/36 patients (44.4%) of them having one previous attack in the past, again comparable to study by Ojha et al, where 43% patients were reported to have one such previous attack4. These findings confirm prolonged suffering of these patients due to SAIO alongwith waxing and waning nature of the condition.
The important features of intestinal obstruction are colicky abdominal pain, nausea and vomiting, abdominal distension, and a cessation of flatus and bowel movements. It is essential to demarcate between true mechanical obstruction and other causes of these symptoms. Most of the patients of SAIO in this study presented with multiple symptoms out of which abdominal pain (89.4%) and non-passage of faeces or flatus (78.9%) were more frequent as compared to vomiting (68.4%) and distension of abdomen (63.1%). Colicky type of abdominal pain (49.1%) is more common than continuous abdominal pain (40.3%) in the SAIO cases studied. This is in contrast to the study by Ojha et al, where colicky abdominal pain (89%) and vomiting (82%) were more frequent than non-passage of flatus or faeces (46%) and distension of abdomen (44%)4. Lower abdominal surgeries, including appendectomies, colorectal surgery, gynaecologic procedures, and hernia repairs, are associated with a greater risk of adhesive small bowel obstruction9. In our study, 28/57 (49.1%) patients were found to have a history of previous abdominal surgery, the common surgeries performed being gynaecological procedures in 8 patients and laparotomy for abdominal trauma in 7 patients. On physical examination, the most frequent finding was presence of abdominal tenderness seen in 80.7% patients followed by distension of abdomen (61.4%) which is different from study by Ojha et al, where the most frequent finding was exaggerated bowel sounds (60.3%). Lesser degree of distension may be due to continued passage of flatus/faeces in the SAIO patients. Increased bowel sounds, visible/palpable bowel loops, abdominal distension and lumps in the abdomen were observed in 60.3%, 28.5%, 25.3% and 19.0% patients, respectively in a study by Jain BK et al9. The findings of our study point more towards subacute nature of the intestinal obstruction, mostly due to small bowel involvement.
The primary investigation of patients with clinical signs and symptoms of intestinal obstruction should include plain upright abdominal radiography. Radiography can quickly detect if intestinal perforation has occurred; free air can be seen above the liver in straight films or left lateral decubitus films. Radiography can diagnose intestinal obstruction in approximately 60 percent of cases10. In our study, 36/57 (63.2%) patients had gaseous distension of bowel loops and only 5/57 patients (8.8%) had multiple air fluid levels as compared to Ojha et al where 47/63 patients (74.6%) had multiple air-fluid levels on erect films4. However, plain X-ray films of abdomen appeared normal in 16/57(36.8%) patients which might be due to early obstruction and high jejunal or duodenal obstruction. As a general rule, most underlying causes of bowel obstruction cannot be diagnosed with an abdominal radiograph, as they are radiologically occult. Ultrasonography remains a reliable investigation for unstable patients with a confusing diagnosis and in patients for whom radiation exposure is contraindicated, such as pregnant women. It is extremely sensitive for diagnosing high-grade intestinal obstruction, sensitivity being almost 85 percent11. Ultrasonography was undertaken in 53 (92.9%) patients. It showed abnormal findings in 49 patients while it was reported normal in 4 patients. Dilated bowel loops were the most frequent finding in 27 patients. Nowadays, CT scan has largely replaced ultrasonography as the first-line investigation in stable patients in whom intestinal obstruction is suspected. In clinically suspected patients of intestinal obstruction, where initial radiography is negative, Contrast enhanced computed tomography (CECT) should be undertaken12. CT is appropriate for further evaluation of patients with suspected intestinal obstruction in whom clinical examination and radiography do not yield a definitive diagnosis(as in our study). CT is sensitive for detection of high-grade obstruction (up to 90 percent in some series)13, and has the additional benefit of defining the cause and level of obstruction in most patients14,15. It is seen that, though CT is highly sensitive and specific for high-grade obstruction, its value decreases in patients with partial obstruction1. In most patients, CT should be ordered when the diagnosis is in doubt, when there is no surgical history or hernias to explain the etiology, or when there is a high index of suspicion for complete or high-grade obstruction. In our study, CT findings were confirmatory for diagnosing the condition in 25 cases.
The management of intestinal obstruction should aim at correcting physiologic derangements caused by the obstruction, bowel rest, and removing the source of obstruction. The decision to perform surgery for subacute intestinal obstruction (SAIO) can be difficult. Treatment of stable patients with subacute intestinal obstruction and a history of abdominal surgery presents a challenge. Conservative management of a high-grade obstruction should be attempted initially, using nasogastric decompression, aggressive intravenous rehydration, and appropriate antibiotics. Conservative management is successful in 40 to 70 percent of clinically stable patients, with a greater success rate in those with partial obstruction16,17. With conservative management, resolution generally occurs within 24 to 48 hours. Beyond this time frame, the risk of complications, including vascular compromise, increases. If intestinal obstruction is not resolved with conservative management, surgical evaluation is required18. In our study 39 ( 68.4%) patients were managed conservatively in a successful manner and remaining 18 (31.6%) patients were subjected to surgery. Adhesiolysis was the most common surgical procedure performed in 12/18 patients followed by resection and anastomosis of bowel in 3/18 patients.
Following the diagnostic modalities and the surgical procedures, the probable causes of intestinal obstruction in 40 patients were delineated. According to another study, adhesions due to prior abdominal surgery are the predominant cause of small bowel obstruction, these are seen in approximately 60 percent of cases19. In our study, adhesions were found to be the most common cause in 21 (52.5%) patients followed by small intestinal strictures in 6 (15%) patients, compared to the study by Jain BK et al, where adhesions and small intestinal strictures were the two most frequent cause of obstruction seen in 31.8% and 27.2%, respectively9. In rest of the 17 patients, in whom the diagnosis could not be ascertained by various means, the causes could be attributed to some obscure pathology including dyselectrolytemia leading to paralytic ileus.
Although conservative management is associated with shorter initial hospitalization, there is also a higher rate of eventual recurrence20. Out of the 39 patients managed conservatively in the study, 5 patients presented again during the study period, but with acute intestinal obstruction and were managed with surgery (they were not included in the study for the second time).
There were no mortalities noted in our study group during the period of observation. Based on our study, we assume that small intestinal obstruction might be a more common cause of SAIO than large intestinal obstruction. Unfortunately, no relevant data pertaining to the follow up of the progress of patients was available to us at the time of compiling this study, which is the limitation of this study.
Conclusion
Subacute intestinal obstruction continues to be one of the most common abdominal problems faced by general surgeons. The present study concluded that subacute intestinal obstruction (SAIO) is seen more commonly in middle age group although no age is immune, with males more commonly affected than females. We observed that abdominal pain was the commonest symptom, while tenderness was the most common sign elicited in these patients. Inspite of the atypical presentation of this confusing entity, majority of the cases of SAIO were managed conservatively. Almost half of the patients had a previous history of surgery and post operative adhesions were largely implicated in causation of SAIO. Early clinical recognition and tools like plain X-ray erect abdomen, ultrasonography, CT scan are extremely important in diagnosing this clinical entity.
Based on our findings, we hope that the clinical characteristics of this ill-defined term will become clear and help in the better management of SAIO, thereby reducing mortality and long-term morbidity. We intend to extend this study further by collecting data on the follow up of the progress of the same patients with time.
Acknowledgement
We are grateful to the staffs involved in collection of the data for the study.
Conflict of Interest
There is no conflict of interest.
Source of Funding
There is no funding source.
References
- Jackson PG, Raiji M. Evaluation and Management of Intestinal Obstruction. Am Fam Physician 2011;83(2): 159-165
- Chintumalla PK, Vemulapally NK, Reddy SN. Clinical study of bowel obstruction in relation to etiological factors. Int Surg J. 2017 Feb;4(2):485-490
- “Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015”. GBD 2015 Mortality and Causes of Death, Collaborators. (October 8, 2016). Lancet. 388(10053): 1459–1544. doi:1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- Ojha A, Jalaj A, Tiwari S, Prasheel V.M . :Diagnosis and Management of Subacute Intestinal Obstruction: A Prospective Study. Journal of Evolution of Medical and Dental Sciences 2014; Vol. 3, Issue 26, June 30; Page: 7326-7340, DOI: 10.14260/jemds/2014/2898
- Fitzgerald, J. Edward F. (2010). “Small Bowel Obstruction”. Emergency Surgery. Oxford: Wiley-Blackwell. -pp. 74-79. doi:1002/9781444315172.ch14. ISBN 9781405170253. Archived from the original on September 8, 2017.
- Gore, RM; Silvers, RI; Thakrar, KH; Wenzke, DR; Mehta, UK; Newmark, GM; Berlin, JW (November 2015). “Bowel Obstruction”. Radiologic Clinics of North America. 53(6): 1225–40. doi:1016/j.rcl.2015.06.008. PMID 26526435
- Ray MS, Deepak BS. An unusual cause of sub-acute intestinal obstruction. Int Surg J 2016;3:2310-3.
- Ferri, Fred F. (2014). Ferri’s Clinical Advisor 2015: 5 Books in 1. Elsevier Health Sciences. p. 1093. ISBN9780323084307. Archived from the original on September 8, 2017.
- Jain BK, Agrawal J, Rathi V, Garg PK, Dubey IB. Subacute intestinal obstruction: an enigma revisited. Trop Doct. 2013 Jan;43(1): 5-8
- Maglinte DD, Heitkamp DE, Howard TJ, Kelvin FM, Lap-pas JC. Current concepts in imaging of small bowel obstruction. Radiol Clin North Am. 2003;41(2):263–283.
- Lim JH, Ko YT, Lee DH, Lee HW, Lim JW. Determining the site and causes of colonic obstruction with sonography. AJR Am J Roentgenol. 1994;163(5):1113–1117.
- Vaishnani, Bhavesh V, Dudhwala, Mohammad FG. Clinical study on role of CECT abdomen in intestinal obstruction. International Journal of Research in Medical Sciences. 2019 Mar;7(4):967-971
- Suri S, Gupta S, Sudhakar PJ, Venkataramu NK, Sood B, Wig JD. Comparative evaluation of plain films, ultrasound and CT in the diagnosis of intestinal obstruction. Acta Radiol. 1999;40(4):422–428.
- Furukawa A, Yamasaki M, Furuichi K, et al. Helical CT in the diagnosis of small bowel obstruction. Radiographics. 2001;21(2):341–355.
- Frager DH, Baer JW, Rothpearl A, Bossart PA. Distinction between postoperative ileus and mechanical small-bowel obstruction: value of CT compared with clinical and other radiographic findings. AJR Am J Roentgenol. 1995;164(4):891–894.
- Mosley JG, Shoaib A. Operative versus conservative management of adhesional intestinal obstruction. Br J Surg. 2000;87(3):362–373.
- Williams SB, Greenspon J, Young HA, Orkin BA. Small bowel obstruction: conservative vs. surgical management. Dis Colon Rectum. 2005;48(6):1140–1146.
- Fevang BT, Jensen D, Svanes K, Viste A. Early operation or conservative management of patients with small bowel obstruction? Eur J Surg. 2002;168(8–9):475–481.
- Dijkstra FR, Nieuwenhuijzen M, Reijnen MM, van Goor H. Recent clinical developments in pathophysiology, epidemiology, diagnosis and treatment of intra-abdominal adhesions. Scand J Gastroenterol Suppl. 2000; (232):52-9.
- Cox MR, Gunn IF, Eastman MC, Hunt RF, Heinz AW. The safety and duration of non-operative treatment for adhesive small bowel obstruction. Aust N Z J Surg. 1993;63(5):367–371








