Eman Albataineh1*, Enas Al-Zayadneh2, Mohammad Ahmad Abu- Lubad3, Areej Altarawneh4 and Ibrahim Aldmour5
1Department of Microbiology and Immunology, Faculty of Medicine, Mutah University, Al-Karak, Jordan
2Department of Pediatrics, School of Medicine, University of Jordan, Jordan
3Department of Medical Microbiology and Immunology, Mutah University, Faculty of Medicine, Karak, Jordan
4Albasheer Hospital, Amman, Jordan
5Al-Karak Governmental Hospital, Al-Karak, Jordan
Corresponding Author E-mail: emanbatayneh@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/2015
Abstract
Asthma is a chronic disease that affects the patients’ way of life, as it can cause significant Physical, mental and social problems. It is, therefore, important to evaluate the quality of life (QoL) of the asthmatic patients in order to assist them in managing this condition. Aim of the work: The aim of this study was to investigate the QoL determinants in asthmatic adult patients and to identify any differences between the four domains of QoL, namely symptoms, limitations in daily activities, emotional, and exposure to environmental stimuli. Patients and methods: Cross-sectional, questionnaire- based survey was conducted among 93 patients with asthma (aged 14−71) recruited by general practitioners and chest physicians. In addition, all participants completed a demographic questionnaire. Asthma-related QoL was assessed using Juniper Mini-AQLQ (1999), whereas the Asthma Control Questionnaire (ACQ) was employed when determining asthma control. The differences between mean values were evaluated via the student’s t-test or ANOVA test. To quantify the relationship between asthma control and QoL, parametric Pearson correlations were calculated. The binary logistic regression model was adopted to analyze dichotomous variables according to predictor variables. In addition, independent variables with p < 0.05 were included in a multiple linear regression model in order to identify the factors that best predict low QoL scores. Only statistically significant variables (p < 0.05) were retained in the final model. Results: The median patient age was 40.5 years (range = 14−71 years), and 36.6% of patients were male. The mean total QoL score was 3.28±1.56 (3.39 for males and 3.08 for females, p = 0.113), while the mean scores for individual QoL domains were 3.98±1.68 (activity domain), 2.93±1.81 (symptoms domain), 3.39±1.66 (emotional domain), and 2.81±1.86 (environmental domain). Well-controlled asthma and being non-atopic significantly correlated with a higher total AQLQ score, as well as individual scores for the four QoL domains, while age ≤ 55 years correlated with higher total AQLQ and scores on all domains except for the emotional domain. There was a significant association between Allergic Rhinitis (AR) disease and low AQLQ and two (environmental and symptoms) of the four domains. Poorer overall quality of life was recorded in atopic paients sensitive to olive pollens (p < 0.05). Unfortunately, taking treatment, especially ICS, was associated with low QoL scores across all four domains. The factors that best predict poor QoL were positive allergy test (B = -0.203; 95% CI = -0.413−0.007; p = 0.05), bad Asthma Control Test (ACT) (B = -0.164; 95% CI = -0.279−0.048; p < 0.001) and taking ICS (B = -0.192; 95% CI = -0.373−-0.011; p < 0.001).
Keywords
Asthma; Quality of life domains; Quality of life
Download this article as:| Copy the following to cite this article: Albataineh E, Al-Zayadneh E, Abu- Lubad M. A 3, Altarawneh A , Aldmour I. Determinants of Low Quality of Life in Asthmatic Adult Patients in South of Jordan. Biomed Pharmacol J 2020;13(3). |
| Copy the following to cite this URL: Albataineh E, Al-Zayadneh E, Abu- Lubad M. A 3, Altarawneh A , Aldmour I. Determinants of Low Quality of Life in Asthmatic Adult Patients in South of Jordan . Biomed Pharmacol J 2020;13(3). Available from: https://bit.ly/30xbaCF |
Introduction
Bronchial asthma is a widespread condition affecting many people worldwide. It has a heterogeneous etiology that makes it impossible to provide a precise classification of the disease. Bronchial asthma is characterized by episodic improvements and impairments of symptoms such as breathlessness (dyspnea) with wheezing and chest tightness, which can lead to significant limitations in physical, emotional, and social life of asthmatic patients. Asthma morbidity is mainly affected by objective measures such as symptoms, physiological measures and medications, and by subjective measures that can demonstrate how patients feel in their daily life. It is, therefore, important to evaluate the quality of life (QoL) of the patients in addition to the other assessment measures in order to gather full information about their health status.1 Asthma-related quality of life is a subjective concept based on an individual’s perception of the impact of the disease on his life. QoL questionnaires was used for that purpose.2 Numerous studies of asthma patients have investigated their quality of life and its association with different sociodemographic characteristics, such as gender, asthma control, asthma severity, exposure to tobacco smoke, and presence of atopy or allergic rhinitis.3-7 However, few authors have conducted domain-specific analyses of the quality of life of asthma patients. F, we were unable to identify any studies studying the quality of life of asthma patients in Jordan. Understanding the factors that directly affect the quality of life in asthma, especially potentially modifiable ones, can be helpful in designing interventions that improve the life of individuals living with this chronic condition. Thus, the primary aim of the present study was to identify the determinants of low overall QoL and its four domains—(1) symptoms; (2) limitations in daily activities; (3) emotional; and (4) exposure to environmental stimuli—in clinically verified asthmatics.
Patients and Methods
Patients
The data for the present study was collected via a cross-sectional survey involving 93 atopic and non-atopic adult asthma patients aged between 14 and 71 who had been treated for their condition. The patients were enrolled during regular visits to the respiratory outpatient and inpatient departments of Prince Ali Hospital in Alkarak, between March 2013 and June 2014. All participants were clinically diagnosed as having asthma either with or without atopy on the basis of their clinical diagnosis and skin prick testing with inhalant allergens.
Questionnaires
Patients completed questionnaires inquiring into their key demographic features (i.e., sex, age, gender, and smoking habits), duration of asthma, presence of other allergic disease such as allergic rhinitis, body mass index (BMI), asthma medication and personal history of any other comorbid diseases, including hypertension and diabetes. History of influenza vaccination were also obtained.
Asthma control test (ACT) was measured using 5-item questionnaire assessing asthma symptoms, use of medications, and the impact of asthma on daily life [8], whereby a score of ≥ 20 were assessed as a single group (controlled asthma), and those with scores ≤ 19 were placed into the uncontrolled asthma group [9].
Perceived asthma severity was determined by asking patients how severe they thought their asthma was on a 3-point scale including mild, moderate, and severe.
Asthma-related QoL was evaluated using the Mini Asthma Quality of Life Questionnaire (mAQLQ) [10]. This 15-item self-administered questionnaire has been designed to address four domains: symptoms (5 items); limitations in daily activities (4 items); emotional function (3 items); and (4) exposure to environmental stimuli (3 items). The degree of impairment of the QoL was scored on a 7-point scale ranging from 1 (severe impairment) to 7 (no impairment) for each item. The average of the scores related to all 15 questions represented the overall score, and the mean score per domain was calculated.
Allergy Skin Tests
A formal diagnosis of allergy to inhalant allergens, namely Dermatophagoides pteronyssinus (Dp), Dermatophagoides farinae (Df), house dust mite (HDM), olive pollen, cat dander, dog dander, compositae, wall pellitory, salsola kali, four cereals, 12 grasses and mold, along with positive control (histamine) and negative control (vehicle) (Stallergenes, France), was performed in accordance with published guidelines [11]. Atopy was defined as having an allergen-induced wheal reaction equal to or greater than that caused by histamine (1 mg/mL) or exceeding 3 mm in diameter (as ascertained using skin prick tests). The study protocol was approved by the Mutah University Central Ethics Committee and the participants were requested to sign a statement of informed consent.
Statistical Analysis
Results yielded by the mAQLQ were presented as questionnaire scores—ranging from 7 (no impairment in quality of life) to 1 (maximum impairment)—and were expressed as the mean score per item for each of the domains, as well as for the overall quality of life.
Dependent variables were mAQLQ scores, whereas selected patient, disease, and environmental characteristics were treated as independent variables. Student’s t-test and ANOVA were performed to examine the association between each independent variable and the mean AQLQ and its domain scores. To address the correlation between asthma control and QoL and its domains, parametric Pearson correlations were used. The binary logistic regression model was used to analyze dichotomous variables according to predictor variables, and variables with a p-value of less than 0.05 were placed in a multiple linear regression model. Poor QoL was noted if patients scored below the mean.
Results
Sample Characteristics
The median patient age was 40.5 years (range = 14−71 years), and 36.6% of patients were male.
The mean global AQLQ score was 3.28±1.56, while the mean scores for individual QoL domains were 3.98±1.68 (activity domain), 2.93±1.81 (symptoms domain), 3.39±1.66 (emotional domain), and 2.81±1.86 (environmental domain).
The mean AQLQ score was higher in males (3.39±1.41) than in females (3.08±1.64) but the difference was not statistically significant (p = 0.17). The mean value obtained at the asthma control test was 16.64±5.95. Asthma duration ranged from one to forty years (7.29±7.85) and the average body mass index for the recruited patients (BMI) was 27.56±5.04 (Table 1).
Table 1: Key characteristics of the study population.
| Minimum | Maximum | Mean | Std. Deviation | |
| Sex
Men (34) Women (59) Age (years) QOL average of enviromental scaling |
14 1 1
|
71
7 7.00 |
40.47
3.28 2.81 |
13.58
1.56 1.86 |
| average symptom scaling | 1.00 | 7.00 | 2.93 | 1.81 |
| average of activity scaling | 1.00 | 7.00 | 3.98 | 1.68 |
| average of feeling scaling | 1.00 | 7.00 | 3.39 | 1.66 |
| Weight (Kg) | 45 | 110 | 73.25 | 13.25 |
| Length (m) | 120 | 185 | 163.31 | 9.59 |
| BMI | 18.73 | 41.67 | 27.56 | 5.04 |
| time of diagnosis (years) | 1 | 40 | 7.29 | 7.85 |
| asthma control test score 25 | 5.00 | 25.00 | 16.64 | 5.95 |
Mean overall Asthma Quality of Life Questionnaire (AQLQ) scores and scores on its four domains according to different patient characteristics
AQLQ overall score, along with the scores for its four domains—symptoms, limitations in daily activities, emotional function, and exposure to environmental stimuli—were calculated in relation to different patient or disease characteristics. The average of the scores in the 15 questions was recorded as overall AQLQ score, and the mean score per domain was calculated.
As can be seen in Table 2, age < 55 years is significantly associated with better overall AQLQ score as well as scores in all domains except for the emotional domain (p < 0.05).
Asthma duration < 10 years was associated non-significantly with higher overall QoL and individual domain scores, whereas accompanying allergic rhinitis had an adverse impact on the overall QoL and individual domain scores, but the relationship was statistically significant for overall QoL and the environmental and symptoms domain scores only (p < 0.05). Unfortunately, taking treatment (especially ICS) was associated with poor QoL across all four domains (Table 2).
Other factors that may affect asthma-related QoL, such as presence of chronic diseases (hypertension or diabetes), daily tobacco smoking, history of influenza vaccination and BMI, were tested and no significant associations were found (Table 2).
Table 2: Mean scores of Asthma Quality of Life Questionnaire (AQLQ) domains according to patient, disease, and environmental characteristics. (n=number of patients)
| AQLQ domains (mean+- SD) | |||||
| Variable (n) | Overall | Environment
|
Symptoms | Activities
|
Emotions
|
| Form of disease
Non atopic (39) Atopic (54) P |
4.18±1.63 2.63±1.15 0.0 |
3.89± 2.01 2.037± 1.28 0.0 |
3.95±1.91 2.20±1.33 0.0 |
4.71±1.84 3.46±1.35 0.0 |
4.17±1.73 2.833±1.38 0.0 |
| Asthma control
Controlled (42) Uncontrolled (51) P |
4.12±1.57 2.59±1.18
0.0 |
3.66±2.01 2.1176±1.40
0.0 |
3.88±1.80 2.15±1.41
0.0 |
4.80±1.60 3.31±1.44
0.0 |
4.14±1.74 2.78±1.33
0.0 |
| Sex
Men (34) Women (59) P |
3.39±1.41 3.08±1.64 >0.05 |
2.98±1.88 2.52±1.81 >0.05
|
3.08±1.93 2.6765±1.57 >0.05 |
4.18±1.77 3.70±1.50 >0.05 |
3.37±1.79 3.44±1.43 >0.05 |
| Age
Less than 55 (77) More or equal 55 (16) P |
3.46±1.60 2.40±1.01
0.002
|
3.00±1.92 1.93±1.23
0.009
|
3.17±1.82 1.81±1.32
0.006
|
4.19±1.70 3.00±1.21
0.002
|
3.50±1.75 2.87±1.02
0.060 |
| BMI
<30 (68) >=30 (25) P |
3.51±1.92 3.20±1.42 >0.05 |
3.24±2.33 2.66±1.6 >0.05 |
3.20±2.19 2.83±1.66 >0.05
|
3.99±2.09 3.98±1.53 >0.05 |
3.60±1.89 3.32±1.58 >0.05 |
| Smoking
No (67) Yes (26) P |
3.35±1.56 3.09±1.58 >0.05 |
2.88±1.88 2.65±1.83 >0.05 |
3.00±1.82 2.76±1.81 >0.05 |
4.10±1.67 3.69±1.71 >0.05 |
3.44±1.69 3.26±1.63 >0.05 |
| History of allergic rhinitis
No (31) Yes (62) P |
3.8224±1.60758 3.0161±1.48893 0.02 |
3.58±1.97 2.43±1.69 0.005 |
3.49±1.81 2.66±1.76 0.037 |
4.34±1.90 3.80±1.55 >0.05 |
3.87±1.80 3.16±1.55 >0.05 |
| Presence of chronic disease
No (67) Yes (26) P |
3.35±1.51 3.09±1.70 >0.05 |
2.91±1.84 2.57±1.92 >0.05 |
3.07±1.84 2.57±1.72 >0.05 |
4.04±1.62 3.84±1.86 >0.05 |
3.40±1.63 3.38±1.79 >0.05 |
| Patient on treatment
No (21) Yes (72) p |
4.04±1.81 3.06±1.42 0.03 |
3.57±2.22 2.59±1.70 >0.05 |
3.80±1.93 2.68±1.70 0.012 |
4.61±1.80 3.80±1.61 0.05 |
4.1905±1.80 3.16±1.56 0.013 |
| Patient on inhaled b agonist
No (31) Yes (62) p |
3.50±1.69 3.17±1.50 >0.05 |
3.19±1.99 2.62±1.78 >0.05 |
3.19±1.86 2.80±1.78 >0.05 |
4.03±1.77 3.96±1.65 >0.05 |
3.61±1.83 3.29±1.58 >0.05 |
| Patient on inhaled steroids
No (57) Yes (36) p |
3.53±1.61 2.88±1.418 0.048 |
3.05±1.97 2.44±1.62 >0.05 |
3.24±1.92 2.45±1.53 0.039 |
4.17±1.68 3.68±1.67 >0.05 |
3.68±1.51 2.94±1.81 0.037 |
| Patient on oral b agonist
No (74) Yes (19) P |
3.37±1.61 2.93±1.37 >0.05 |
2.93±1.89 2.36±1.70 >0.05 |
3.04±1.83 2.52±1.71 >0.05 |
4.07±1.71 3.63±1.57 >0.05 |
3.44±1.74 3.21±1.35 >0.05
|
| Asthma duration
< 10 year (66) ≥10 years (27) p |
3.38±1.54 3.04±1.62 >0.05 |
2.95±1.83 2.48±1.92 >0.05 |
3.03±1.84 2.70±1.75 >0.05 |
4.01±1.59 3.92±1.92 >0.05 |
3.53±1.67 3.07±1.63 >0.05 |
| History of flu vaccine
No (65) Yes (28) P |
3.21±1.61 4.44±1.53 >0.05 |
2.71±1.85 3.02±1.92 >0.05 |
2.81±1.87 3.11±1.92 >0.05
|
3.86±1.71 4.33±1.67 >0.05 |
3.43±1.78 3.31±1.69 >0.05 |
AQLQ Scores in Controlled and Uncontrolled Asthma
As noted earlier, ≥ 20 and ≤ 19 scores were used to assign patients to controlled and uncontrolled group, respectively. The mean overall AQLQ score for controlled and uncontrolled asthma group was 4.12±1.57 and 2.59±1.18, respectively, whereby the difference between the groups was highly significant for global AQLQ as well as all four domains (t-test, p = 0.0) (Figure 1). Moreover, there were highly significant correlations between AQLQ, four domains mean scores and ACT (p = 0.0) (Figure 2).
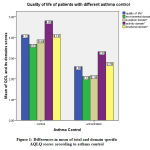 |
Figure 1: Differences in mean of total and domain specific AQLQ scores according to asthma control |
 |
Figure 2: Showing correlation of ACT with AQLQ; overall (A) and the four domains (B, C, D and E). |
Quality of Life of Atopic and Non-Atopic Patients and According to a Specific Allergen
Of 93 patients, 54 (58.1%) showed positive responses to one or more allergens. The total QoL score, as well as scores for all four domains, were significantly higher in patients who did not have atopy compared to those who had (Figure 3).
Poor QoL was defined as a score below mean, which was 3.3. The analysis of influence of allergens on the quality of life of atopic patients showed that majority of patients with atopy had poor QoL especially if they were allergic to olive pollens (Figure 4)
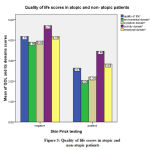 |
Figure 3: Quality of life scores in atopic and non-atopic patients |
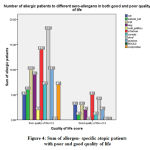 |
Figure 4: Sum of allergen-specific atopic patients with poor and good quality of life |
AQLQ Scores in Mild, Moderate and Severe Asthma
Data analyses revealed that patients who rated their asthma as mild had higher total QoL score, as well as scores for all four domains. No associations between QoL and moderate and severe form were noted (Figure 5).
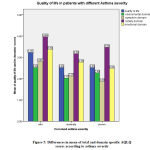 |
Figure 5: Differences in mean of total and domain specific AQLQ scores according to asthma severity |
Quality of Life in Patients Receiving Different Pharmacological Treatment
The findings revealed that long-acting inhaled β2-agonist (LABA) and/or oral short-acting β2-agonist use was non-significantly associated with low total QoL score as well as domain scores. On the other hand, inhaled corticosteroids (ICS) was significantly associated with low overall QoL score, as well as those for emotional and symptoms domains (p < 0.05) (Figure 7). In the studied sample, the most common pharmacological treatments were inhaled long-acting β2-agonists (LABAs), followed by ICSs, and finally oral β2-agonist (Table 2).
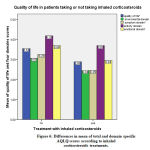 |
Figure 6: Differences in mean of total and domain specific AQLQ scores according to inhaled corticosteroids treatments. |
Risk Factors for Poor Quality of Life in Asthma Patients
Univariate analysis revealed that age > 55 years, poor asthma control, presence of allergic rhinitis, presence of atopy, and receiving pharmacological treatment (mainly ICS) were the main risk factors associated with poor QoL. Subsequent multiple logistic regression (MLR), after adjusting for the confounding variables, showed that the factors that best predict poor QoL were positive allergy test (B = -0.203; 95% CI = -0.413−0.007; p = 0.05), low ACT (B = -0.164; 95% CI = -0.279−0.048; p < 0.001) and taking ICS (B = -0.192; 95% CI = -0.373−-0.011; p < 0.001) (Table 3).
Table 3: Risk factors for poor asthma-specific quality of life among asthma patients
| Factor | Ba | SEb | Bc | t | p-value | 95% CId |
| Atopy | -0.203- | 0.106 | -0.210- | -1.924- | 0.05 | -0.413-0 .007 |
| Asthma control | -0.164- | 0.058 | -0.308- | -2.817- | 0.006 | -0.279–0.048- |
| Taking Inhaled corticosteroids | -0.192- | .0910 | -0.195- | -2.098- | .0390 | -0.373- -0.011 |
Discussion
Asthma is a chronic respiratory disease associated with significant limitation of the patients’ daily activities.
In recent years, many investigations has focused on health-related quality of life in asthmatic patients. As it is an important tool in the estimation of patient health condition and to help in the management of asthma.12
This study was conducted to assess quality of life in asthmatic patients and its associated risk factors using Mini-AQLQ, as this tool can determine patients’ perceptions of physical limitation and mental impairment related with their disease.10 The main advantages of the Mini-AQLQ over other questionnaires are its shorter length and it represents different environmental, emotional, activity and symptoms domains.
In the present study, age < 55 years was significantly associated with better total AQLQ score and scores across all domains, except for emotional domain, which could be due to religious factors prompting patients to accept their destiny. Studies on quality of life and age provide different results. Previous studies showed that older asthmatics had a poorer quality of life compared with younger asthma patients and one of the causes for that is fixed airflow obstruction (FAO) .13, 14 On the other hand, Juniper reported that older asthmatics had adapted to their lifestyle more than the young patients so they had a better life.15
Risk factors associated with FAO in older asthmatic adults include increased asthma duration [14]. This is in agreement with our finding that shorter asthma duration (< 10 years) was associated non-significantly with higher overall QoL score as well as scores in all four domains.
Regarding domains of AQLQ, there was strong correlation between ACT and total QoL and activity domain, symptoms domain, and lower correlation with emotional domain, which may be due to religious beliefs of the study participants. Our study was in agreement with a study conducted by Schatz[5]. In a recent Jordanian study, most of the recruited patients had not achieved optimal asthma control and this was associated with low quality of life.16 One study showed that the ACT correlated significantly with the AQLQ and with each of the four specific domains (activity, emotions, symptoms, and environment).17
Sex has been shown to affect the quality of life in patients with asthma. In the present study, total AQLQ was higher in males than in females but the difference was not statistically significant, which is in agreement with the findings reported for Saudi Arabia.18 The total AQLQ score as well as scores for all four domains were insignificantly higher in male patients compared to female patients, which may be due to the protective role of male sex hormones, given that estrogen fluctuations have been found to cause asthma exacerbation in women.19 Moreover, as women are the main part in the society and at home and they have great role in there, so that a morbid disease like asthma has an additive role in QoL impairment.20
Asthma can be either atopic or non-atopic.13 In this sense, our results indicate that 58% of our patients were atopic, and atopy was associated significantly with poor QoL. The specific allergen that significantly affected QoL in our study was olive pollens. It is well known that the relevant seasonal allergens of the geographical area can cause more deteriorated QOL in the allergic patients while perennial allergens such as dust mite produce less effects that are more tolerable for patients.8 A recent study in Italy.21 indicated that asthma patients sensitized to olive pollen had poorer QoL than those sensitized to grass or house dust mite. These results may be related to different allergen levels and duration in the environment, as the pollens may intensely increase for long time, whereas house dust mite allergens remain in the air in less levels only when turbulence is produced, thus reducing the total amount of allergen inhaled.22
Patients with allergic rhinitis (AR) reported significantly lower overall QoL and achieved lower scores in the environmental and symptoms domains. A previous study using QoL questionnaire showed that patients with both asthma and AR experienced more limitations in QOL than did those suffering from asthma alone.12
Higher levels of perceived asthma severity were not associated with a lower total QoL scores, possibly because patients perceive asthma severity differently from doctors, as lower levels of asthma severity tend to be reported by patients.23 Furthermore, perception of asthma severity tends to differ by gender. Wijnhoven and colleagues24 have reported that men tended to report lower perceived asthma severity.23 Furthermore, some studies showed a different relationship between perceived asthma severity and quality of life. Our findings highlight the need for the physician-assessed severity of disease to prevent underestimation of asthma severity and as a result insufficient management and more morbidity.25
Inhaled corticosteroids (ICS) are considered as the mainstay of controlling airway inflammation in asthma. They have proved their ability to improve asthma control and quality of life exacerbation in patients with asthma.26-28 Asthma is a complex disease and its treatment requires patients’ full cooperation and participation. In our study, ICS significantly decrease the overall QoL score, as well as those for the emotional and symptoms domains, likely because patients with asthma may not respond as expected to therapy because of factors that include poor adherence, improper inhaler technique and treatment with low-dose ICS29 as well as limitations of current IgE- mediated allergic rhinitis disease, as ICS therapy do not directly treat the IgE-mediated component of the asthma disease.30
Conclusion
Uncontrolled asthma, being atopic and taking ICS were significant predictors of poor QoL in the examined sample of asthmatic patients. Our findings revealed considerable differences in the associations between the overall QoL score and those related to four domains and different factors. Thus, AQLQ questionnaire should be used as a routine assessment tool in asthmatic patients, as it supports the results of objective assessments done by the physician to get an efficient indicator of asthma patient health status.
Acknowledgments
The research team is thankful to all school directors and teachers who helped us in data collection.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Written informed consent was obtained from all of the patients who participated. All of the researchers conducted the study in accordance with the Declaration of Helsinki.
Financial Disclosure or Funding
Not applicable, no funding.
Author Contributions
All authors participated to review, and were involved in writing and revising the article prior to submission.
References
- Coban, H. and Y. Aydemir, The relationship between allergy and asthma control, quality of life, and emotional status in patients with asthma: a cross-sectional study. Allergy, Asthma & Clinical Immunology, 2014. 10(1): p. 67.
CrossRef - Jones, P.W., et al., A self-complete measure of health status for chronic airflow limitation. Am Rev Respir Dis, 1992. 145(6): p. 1321-1327.
CrossRef - Gonzalez-Barcala, F.-J., et al., Factors associated with health-related quality of life in adults with asthma. A cross-sectional study. Multidisciplinary respiratory medicine, 2012. 7(1): p. 32.
CrossRef - Ford, E.S., et al., Determinants of quality of life among people with asthma: findings from the Behavioral Risk Factor Surveillance System. Journal of asthma, 2004. 41(3): p. 327-336.
CrossRef - Schatz, M., et al., The relationship between asthma-specific quality of life and asthma control. Journal of Asthma, 2007. 44(5): p. 391-395.
CrossRef - Stucky, B.D., et al., Understanding asthma-specific quality of life: moving beyond asthma symptoms and severity. European Respiratory Journal, 2015. 46(3): p. 680-687.
CrossRef - Vandenplas, O., et al., The impact of concomitant rhinitis on asthma‐related quality of life and asthma control. Allergy, 2010. 65(10): p. 1290-1297.
CrossRef - Thomas, M., et al., The Asthma Control TestTM (ACT) as a predictor of GINA guideline-defined asthma control: analysis of a multinational cross-sectional survey. Primary Care Respiratory Journal, 2009. 18(1): p. 41.
CrossRef - Juniper, E.F., et al., Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respiratory medicine, 2005. 99(5): p. 553-558.
CrossRef - Juniper, E., et al., Development and validation of the mini asthma quality of life questionnaire. European Respiratory Journal, 1999. 14(1): p. 32-38.
CrossRef - Dreborg, S. and A. Frew, Position paper: allergen standardization and skin tests. Allergy, 1993. 48: p. 49-54.
CrossRef - Leynaert, B., et al., Quality of life in allergic rhinitis and asthma: a population-based study of young adults. American journal of respiratory and critical care medicine, 2000. 162(4): p. 1391-1396.
CrossRef - Spiriæ, V.T., et al., Assessment of the asthma quality of life questionnaire (AQLQ): Serbian translation. Croat Med J, 2004. 45(2): p. 188-94.
CrossRef - Bennett, G.H., et al., Risk factors and clinical outcomes associated with fixed airflow obstruction in older adults with asthma. Annals of Allergy, Asthma & Immunology, 2018. 120(2): p. 164-168. e1.
CrossRef - Juniper, E.F., et al., Measuring health-related quality of life in adults during an acute asthma exacerbation. Chest, 2004. 125(1): p. 93-97.
CrossRef - Almomani, B.A., et al., Asthma insights from Jordan: cross-sectional observational study. Journal of Asthma, 2016. 53(4): p. 349-355.
CrossRef - Kwon, H.-S., et al., Correlation between the Korean version of Asthma Control Test and health-related quality of life in adult asthmatics. Journal of Korean medical science, 2008. 23(4): p. 621-627.
CrossRef - Torchyan, A.A., et al., Asthma quality of life in Saudi Arabia: Gender differences. Journal of Asthma, 2017. 54(2): p. 202-209.
CrossRef - Baldaçara, R.P.d.C. and I. Silva, Association between asthma and female sex hormones. Sao Paulo Medical Journal, 2017. 135(1): p. 4-14.
CrossRef - Koper, I., K. Hufnagl, and R. Ehmann, Gender aspects and influence of hormones on bronchial asthma–Secondary publication and update. World Allergy Organization Journal, 2017. 10(1): p. 46.
CrossRef - Accordini, S., et al., The cost of persistent asthma in Europe: an international population-based study in adults. International archives of allergy and immunology, 2013. 160(1): p. 93-101.
CrossRef - Exchange of ideas and information on the issue of Competitive Change in the Electric Power Industry. Topic: What are the issues involved in competition?, in Committee on Energy and Natural Resources1997, Bureau of National Affairs: Washington, D.C. p. 17.
- Allen, G.M., Bats: biology, behavior, and folklore2004, Mineola, N.Y.: Dover Publications. x, 368, [26] p. of plates.
- Carlstrom, L. and M. Castro, Severe asthma: what makes it so hard to manage? Current allergy and asthma reports, 2009. 9(5): p. 393-400.
CrossRef - Sullivan, P.W., et al., Asthma in USA: its impact on health-related quality of life. Journal of Asthma, 2013. 50(8): p. 891-899.
CrossRef - Demarche, S.F., et al., Effectiveness of inhaled corticosteroids in real life on clinical outcomes, sputum cells and systemic inflammation in asthmatics: a retrospective cohort study in a secondary care centre. BMJ open, 2017. 7(11): p. e018186.
CrossRef - Barnes, P.J., Efficacy of inhaled corticosteroids in asthma. Journal of allergy and clinical immunology, 1998. 102(4): p. 531-538.
CrossRef - Louis, R., F. Schleich, and P.J. Barnes, Corticosteroids: still at the frontline in asthma treatment? Clinics in chest medicine, 2012. 33(3): p. 531-541.
CrossRef - Roberts, J. and A. Williams, Quality-of-life and asthma control with low-dose inhaled corticosteroids. British journal of nursing, 2004. 13(19): p. 1124-1129.
CrossRef - Hayden, M.L., Immunoglobulin E‐mediated airway inflammation is active in most patients with asthma. Journal of the American Academy of Nurse Practitioners, 2007. 19(9): p. 439-449.
CrossRrf







