Manuscript accepted on :December 24, 2016
Published online on: --
Plagiarism Check: Yes
Mehrnaz Asadi Gharabaghi1*, Masoud Ehtesham1 , Reza Mollazadeh2 , Shahram Firouzbakhsh1 and Enayat Safavi1
1Advanced Thoracic Research Center, Department of Pulmonary Diseases, Tehran University of Medical Sciences, Tehran, Iran.
2Department of Cardiology, Tehran University of Medical Sciences, Tehran, Iran.
Corresponding Author Email: asadi_m@tums.ac.ir
DOI : https://dx.doi.org/10.13005/bpj/1031
Abstract
Temporary cessation of breathing or obstructive sleep apnea is a known risk factor for cardiovascular diseases. Autonomic cardiac measurement by HRV indexes is a known identification methods for heart condition during sleep that identifying their relationship with AHI index can help to detect those indexes relationship with disease severity. In addition to help to estimate the risk of heart problems to begin treatment of the diseases, according to the HRV indexes and in mild cases AHI, reducing the risk of cardiovascular problems in patients. This cross sectional study contained 36 patients suffered from obstructive sleep apnea whom referred to the sleep clinic of Imam Khomeini hospital, Tehran, Iran, in 2015. Apnea syndrome in these patients was confirmed by polysomnography. Participants were divided into two groups, severe (AHI≥30) and non-severe (AHI=5-29). Age, BMI, resting heart rate and obtained HRV indexes by a sleep test (polysomnography) were recorded for each patients. Statistical analysis was done by SPSS ver. 19. Statistical analysis did not show any significant differences for age and BMI between two groups. The results showed that only SDNNi index (P-value= 0.026) and ODI index (P-value= 0.001) had significant difference between the two groups. AHI had the most correlation with HRV-triangular index (P=0.022, rp=0.371) between HRV indexes and with ODI (P=0.001, rp=0.63) among all parameters. According to the results of this study, HRV indexes had not significant different between the two groups and only ODI index differed significantly. Therefore, it seems clinical judgment cannot be done based on adnexal data in all societies.
Keywords
Obstructive Sleep Apnea (OSAS); Heart Rate Variability (HRV); Apnea Hypopnea index (AHI); Oxygen Desaturation Index (ODI)
Download this article as:| Copy the following to cite this article: Gharabaghi M. A, Ehtesham M, Mollazadeh R, Firouzbakhsh S, Safavi E. Comparative Study of HRV Indexes Between Severe and Non-Severe Obstructive Sleep Apnea Patients. Biomed Pharmacol J 2016;9(3). |
| Copy the following to cite this URL: Gharabaghi M. A, Ehtesham M, Mollazadeh R, Firouzbakhsh S, Safavi E. Comparative Study of HRV Indexes Between Severe and Non-Severe Obstructive Sleep Apnea Patients. Biomed Pharmacol J 2016;9(3). Available from: http://biomedpharmajournal.org/?p=11789 |
Introduction
Sleep apnea is a sleep disorder characterized by pauses in breathing or instances of shallow or infrequent breathing during sleep. Each pause in breathing, called an apnea, can last for several seconds to several minutes, and may occur, by definition, at least 5 times in an hour. (1) Sleep apnea is classified as a dyssomnia, meaning abnormal behavior or psychological events occur during sleep. (2) There are three forms of sleep apnea: central (CSA), obstructive (OSA), and complex or mixed sleep apnea (i.e. a combination of central and obstructive) constituting 0.4%, 84%, and 15% of cases, respectively. (3)
Apnea syndrome (OSAS) during sleep is a common disorder that suffered about 7 percent of comminutes and this syndrome is more common in men than women. (4) Symptoms of this syndrome are poor sleep and sometimes severe snoring and daytime sleepiness and fatigue. Complications of this syndrome include depression, lack of glycemic control, heart attacks, arrhythmias, and cardiovascular complications such as high blood pressure. (5-9) Also, its association with vascular pathology especially atherosclerosis has been recognized. Alternating and frequent decline blood oxygen saturation and increased respiratory effort to open the sympathetic tone collapsed airway and the renin-angiotensin-aldosterone system (RAAS) will be the most probable pathophysiological mechanism of this syndrome in order to progress cardiovascular diseases. According to this, evaluation of cardiovascular function in these patients is a necessary action. In 1981, Akselrod et al proved the relationship between HRV (Heart Rate Variability) and autonomic nervous system. (10)
HRV is the physiological phenomenon of variation in the time interval between heartbeats. It is measured by the variation in the beat-to-beat interval. (11) Index analysis of HRV is a non-invasive method known in the evaluation of cardiac autonomic nervous system, and also the relationship between disturbances of HRV indexes have been demonstrated with increased mortality of animals and this method became a predictive tool for angina and MI. (12, 13) Reduced HRV has been shown to be a predictor of mortality after myocardial infarction (14) although others have shown that the information in HRV relevant to acute myocardial infarction survival is fully contained in the mean heart rate. (15) A range of other outcomes/conditions may also be associated with modified (usually lower) HRV, including congestive heart failure, diabetic neuropathy, depression, post-cardiac transplant, susceptibility to SIDS and poor survival in premature babies.
HRV indexes changes in OSAS were evaluated in some studies (16-18) and even suggested this method is a proper technic for screening.(19) Therefore, the cardiovascular status could be evaluated by determination of these indexes relation with severity of this syndrome which classified based on AHI (Apnea Hypopnea index). Also it can be determined which of the indexes have better relationship with disease severity to be more helpful in clinical assessment and treatment. Meanwhile, these indexes can be used to evaluate the starting time and follow up treatment such as CPAP. (20)
Considering to finding changes in patients HRV indexes based on the severity of the disease and finding the best differentiate index or indexes will be helpful for the next clinical judgments, This study was conducted to compare the HRV indexes in patients with severe and non-severe obstructive sleep apnea in patients referred to the sleep clinic of Imam Khomeini hospital in 2015.
Methods
In this cross sectional study 39 patients suffered from obstructive sleep apnea referred to the sleep clinic of Imam Khomeini hospital, Tehran, Iran, were recruited. The sampling was census and the total volume of the sample was calculated according to Formula 1. Patients with cardiac arrhythmias, hypertension, IHD history (known coronary disease), and thyroid function disorders and in patients treated with beta-blocker drugs, calcium blockers, anti-arrhythmic and autonomic nervous system drugs either inhaled or oral such as bronchodilators and addicted to narcotics or drugs affecting autonomic dysfunction, were excluded.
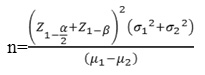
Formula 1- This formulas was used to calculate volume of sample. n= Number of samples, α=0.05, β=0.2, µ1=17.3, µ2=21.6, σ1=4.7, σ2=7.8, Z1-α/2=1.961150776, Z1-β=0.841623031
Patients with symptoms of obstructive sleep apnea syndrome were examined by polysomnography with Embla N7000 and medcare embla Reykjavik, Iceland software. Patients with obstructive sleep apnea was diagnosed by analyzing EEG and respiratory movements. Participants were divided into two groups, severe (AHI≥30) and non-severe (AHI=5-29), according to the number of apnea episodes (=apnea for at least 10 seconds) and hypopnea (=decrease in respiratory flow for at least 10 seconds) per hour of sleeping.
Age, BMI, resting heart rate and obtained HRV indexes by a sleep test (polysomnography) were recorded for each patients. Code sheet and master sheet data was entered into SPSS software ver. 19 for statistical analysis. For qualitative variables frequency (frequency) and for quantitative variables, the mean, range and standard deviation were calculated. T-test and chi-square test were used for statistical analysis and P-value<0.05 was considered as a significant level.
It notable the principles of the Helsinki Declaration was considered in this study.
Results
Patients contained 26 male and 13 female. Participants were divided into two groups, severe (AHI≥30) and non-severe (AHI=5-29), in this study. The sever group were contained 19 participants and the mean age and BMI were 52.29±13.64 and 34.23±9.22, respectively. Meanwhile, the non-sever group were contained 20 patients whom their mean age and BMI were 53.43±9.59 and 31.08±7.29, respectively. Statistical analysis showed no significant differences between two groups for these parameters. (P-value for age=0.51, P-value for BMI=0.24)
Time domain and frequency domain parameters were evaluated in this study. The results showed that only SDNNi index (P-value= 0.026) and ODI index (blood oxygen desaturation index) (P-value= 0.001) had significant difference between the two groups and differences between other indexes were not significant. (Table 1)
Table 1: Time domain and frequency domain of HRV indexes and oxygen desaturation index (ODI) in patients with severe and non-severe obstructive sleep apnea
| Variables | Sever | Non-sever | P-value | ||
| Mean | SD | Mean | SD | ||
| SDNN | 117.29 | 63.95 | 87.41 | 55.09 | 0.184 |
| SDNNi | 101.59 | 65.26 | 61.32 | 36.37 | 0.026 |
| SDANN | 86.06 | 70.58 | 88.23 | 88.23 | 0.835 |
| NN50 | 6161.35 | 7412.16 | 3481.14 | 3943.58 | 0.343 |
| HF | 5146.95 | 3932.2 | 4151 | 2032.8 | 0.395 |
| LF | 20075.94 | 25549.68 | 14581.5 | 9046.8 | 0.361 |
| VLF | 28228.12 | 31437.5 | 17755.82 | 9507.29 | 0.118 |
| Total | 53953.24 | 55921.5 | 38366.91 | 19480.47 | 0.230 |
| LF/HF | 4.83 | 4.46 | 4.75 | 6.13 | 0.448 |
| HRV | 17.41 | 7.25 | 14.59 | 7.1 | 0.401 |
| Desat(ODI) | 60.29 | 26.19 | 19.45 | 19.91 | 0.001 |
Analyzed data for AHI and HRV time dependent indexes relation showed SDNN (P-value= 0.038, rp=0.337), SDDNi (P-value=0.016, rp=0.338), and HRV-triangular (P-value=0.022, rp=0.371) indexes had direct and significant correlation with AHI. On the other hand, SDANN (P-value=0.745, rp=0.054) and NN50 (P-value=0.182, rp=0.221) had direct correlation with AHI, but they were not significant. (Table 2)
Table 2: Time domain HRV indexes relation with AHI in OSAS patients
| Variables | AHI | |
| P-value | rp | |
| NN50 count | 0.182 | 0.221 |
| SDNNi | 0.016 | 0.388 |
| SDANN | 0.745 | 0.054 |
| SDNN | 0.038 | 0.337 |
| HRV triangular index | 0.022 | 0.142 |
AHI relation with frequency domain HRV indexes are shown in Table 3. Statistical analysis showed there is no significant relation between them. Meanwhile, our results illustrated that LF (P-value=0.445, rp=0.125), VLF (P-value=0.332, rp=0.162), and Total power (P-value=0.395, rp=0.142) indexes had direct and HF (P-value=0.360, rp= -0.153) had reverse relation with AHI.
Table 3: Frequency domain HRV indexes relation with AHI in OSAS patients
| Variables | AHI | |
| P-value | rp | |
| LF/HF | 0.794 | 0.044 |
| Power HF | 0.360 | – 0.153 |
| Power LF | 0.455 | 0.125 |
| Power VLF | 0.332 | 0.162 |
| Power total | 0.395 | 0.142 |
Also, AHI relation with blood oxygen desaturation index (ODI), age, and BMI was statistically analyzed which is shown in Table 4.
Table 4: ODI index, Age, and BMI relation with AHI in OSAS patients
| Variables | AHI | |
| P-value | rp | |
| ODI | 0.001 | 0.633 |
| Age | 0.903 | – 021 |
| BMI | 0.323 | 0.165 |
Discussion
The aim of this study was comparison of HRV indexes such as SDNN, SDNNi, NN50 count, SDANN, HRV Triangular Index between sever and non-sever obstructive sleep apnea patients referred to a sleep test section of Imam Khomeini hospital, Tehran, Iran, in 2015. Also we tried to find these parameters relation with AHI.
In a number of studies changes in indices of HRV in OSAS have examined and the relationship between the severity of OSAS, and the HRV parameters have been found. Roche et al analyzed time domain parameters on 39 patients whom divided into two groups according to their AHI. Due to their results these adnexal generally considered as a screening tool and they found a significant correlation between disease severity and time indexes. (19) Narkiewics et al compared three groups of patients with normal controls. they found that the parameters of the LF/HF ratio and HF power and LF power in moderate and severe groups is higher compared to the control group and of LF/HF ratio in these groups is higher in comparison to mild group. (21) Gula et al stated that the LF/HF ratio in patients with moderate OSAS is even higher than the severe and the control groups. (22)
In other research, Aydin et al studied three groups of participants, control, sever, and non-sever. They reported frequency domain HRV parameters are higher in patients groups. Meanwhile, LF index and LF/HF ratio were higher on sever group. (23) Like our results, Yang et al reported that blood oxygen desaturation index had significant differences between sever and non-sever patients. (24) Park et al, in a study conducted on 59 patients with untreated OSAS in Korea reported all indexes in the severe group was higher in comparison to non-severe and frequency domain indexes, especially LF/HF ratio had better associated with the severity of AHI. (25)
In this study, obtained results did not show any significant differences between two groups for age and BMI. According to this, it can be concluded that these two factors do not have any effect of internal autonomy system and analyzed data.
Our results about HRV indexes were against some other studies. As an example, Park et al demonstrated that most of parameters were significantly higher on sever group and considered these parameters as a criterion for decision-making. (25) While in this study, none of the HRV indices except SDNNi had not significant different between the two groups of patients with OSAS, but ODI index, like most studies, was significantly different (Table 1). Like our results, Yang et al showed lake of differences between sever and non-sever groups as well. It can be concluded that HRV indexes are not reliable for clinical decision and treatment procedure instead of AHI. (24)
These parameters similarity would have various reasons such as, time domain indexes difference according to sleep phases, ethnic differences in autonomic disorders, latent diseases (e.g. Impaired Fasting Glucose (IFG)), HRV assessment method (overnight instead of 24 hours holter monitoring), and the most important one, impaired autonomic status in patients with low AHI. According to Table 2 and 3, in this study, except HF power index, the most of HRV parameters had direct relation with AHI index and this relation was significant for SDNN, SDNNi, and HRV triangular. Therefore, it seems, according to the results of this study and other studies these adnexal can be proposed as an indicator of disease severity. In addition this test can be suggested as the effects of OSAS on cardiovascular system, despite to other normal diagnostic procedures, particularly in patients with severe AHI.
In spite of lack of significant differences between HRV indexes on sever and mild group in a study by Yang et al, ODI index had significant and direct relation between those two groups. Our results illustrated the significant difference for ODI index as well.
Conclusion
According to the results of this study, it can be concluded that SDNN, SDNNi, and HRV triangular can be proposed as an indicator of obstructive sleep apnea severity in our samples. Meanwhile, by comparing our results with other studies it can be concluded that HRV indexes are not reliable for clinical decision and treatment procedure instead of AHI.
References
- Health UDo, Services H. Sleep apnea: what is sleep apnea. Health Information for the Public NHLBI. 2010.
- Green S. Biological Rhythms, Sleep and Hypnosis: Palgrave Macmillan; 2011.
- Morgenthaler TI, Kagramanov V, Hanak V, Decker PA. Complex sleep apnea syndrome: is it a unique clinical syndrome? SLEEP-NEW YORK THEN WESTCHESTER-. 2006;29(9):1203.
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. New England Journal of Medicine. 1993;328(17):1230-5.
- Powell NB, Schechtman KB, Riley RW, Li K, Guilleminault C. Sleepy driving: accidents and injury. Otolaryngology–Head and Neck Surgery. 2002;126(3):217-27.
- Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. New England Journal of Medicine. 1999;340(11):847-51.
- Pashayan AG, Passannante AN, Rock P. Pathophysiology of obstructive sleep apnea. Anesthesiology Clinics of North America. 2005;23(3):431-43.
- Peker Yk, Hedner J, Norum J, Kraiczi H, Carlson J. Increased incidence of cardiovascular disease in middle-aged men with obstructive sleep apnea: a 7-year follow-up. American journal of respiratory and critical care medicine. 2002;166(2):159-65.
- Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. New England Journal of Medicine. 2000;342(19):1378-84.
- Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger A, Cohen RJ. Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. science. 1981;213(4504):220-2.
- Bruser C, Winter S, Leonhardt S, editors. Unsupervised heart rate variability estimation from ballistocardiograms. proceedings of the 7th International Workshop on Biosignal Interpretation; 2012.
- Barron HV, Viskin S. Autonomic markers and prediction of cardiac death after myocardial infarction. The Lancet. 1998;351(9101):461-2.
- Tsuji H, Larson MG, Venditti FJ, Manders ES, Evans JC, Feldman CL, et al. Impact of reduced heart rate variability on risk for cardiac events The Framingham Heart Study. Circulation. 1996;94(11):2850-5.
- Bigger JT, Fleiss JL, Steinman RC, Rolnitzky LM, Kleiger RE, Rottman JN. Frequency domain measures of heart period variability and mortality after myocardial infarction. Circulation. 1992;85(1):164-71.
- Abildstrom SZ, Jensen BT, Agner E, TORP‐PEDERSEN C, Nyvad O, Wachtell K, et al. Heart rate versus heart rate variability in risk prediction after myocardial infarction. Journal of cardiovascular electrophysiology. 2003;14(2):168-73.
- Dixon JB, Schachter LM, O’Brien PE, Jones K, Grima M, Lambert G, et al. Surgical vs conventional therapy for weight loss treatment of obstructive sleep apnea: a randomized controlled trial. Jama. 2012;308(11):1142-9.
- Eckert DJ, White DP, Jordan AS, Malhotra A, Wellman A. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. American journal of respiratory and critical care medicine. 2013;188(8):996-1004.
- Phillips CL, Grunstein RR, Darendeliler MA, Mihailidou AS, Srinivasan VK, Yee BJ, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. American journal of respiratory and critical care medicine. 2013;187(8):879-87.
- Roche F, Gaspoz J-M, Minini P, Pichot V, Duverney D, Costes F, et al. Screening of obstructive sleep apnea syndrome by heart rate variability analysis. Circulation. 1999;100(13):1411-5.
- Kufoy E, Palma J-A, Lopez J, Alegre M, Urrestarazu E, Artieda J, et al. Changes in the heart rate variability in patients with obstructive sleep apnea and its response to acute CPAP treatment. PLoS One. 2012;7(3):e33769.
- Narkiewicz K, Montano N, Cogliati C, van de Borne PJ, Dyken ME, Somers VK. Altered cardiovascular variability in obstructive sleep apnea. Circulation. 1998;98(11):1071-7.
- Gula LJ, Krahn AD, Skanes A, Ferguson KA, George C, Yee R, et al. Heart rate variability in obstructive sleep apnea: a prospective study and frequency domain analysis. Annals of Noninvasive Electrocardiology. 2003;8(2):144-9.
- Aydin M, Altin R, Ozeren A, Kart L, Bilge M, Unalacak M. Cardiac autonomic activity in obstructive sleep apnea: time-dependent and spectral analysis of heart rate variability using 24-hour Holter electrocardiograms. Texas Heart Institute Journal. 2004;31(2):132.
- Yang A, Schäfer H, Manka R, Andrié R, Schwab JO, Lewalter T, et al. Influence of obstructive sleep apnea on heart rate turbulence. Basic research in cardiology. 2005;100(5):439-45.
- Park D-H, Shin C-J, Hong S-C, Yu J, Ryu S-H, Kim E-J, et al. Correlation between the severity of obstructive sleep apnea and heart rate variability indices. Journal of Korean medical science. 2008;23(2):226-31.







