Manuscript accepted on :June 25, 2016
Published online on: --
Plagiarism Check: Yes
Bahram Fariborz Farsad1, Naser Hadavand1*, Hanieh Salehi2 and Farzaneh Shekari2
1Pharm.D, BCPS, Assistant Professor, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical sciences, Tehran, Iran.
2Department of Pharmacology , Pharmaceutical Sciences Branch , Islamic Azad University , Tehran , Iran.
Corresponding Author E-mail: Hadavandn@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/968
Abstract
The Aim of this study is to access the number of inappropriate usages of post CABG antibiotics such as, Carbapenems, Teicoplanin and Linezolid in Shahid Rajaie Hospital and to apply antibiotic practice guidelines and strategies to reduce inadequate treatment while determining their impact on patient outcomes. This retrospective study was performed at special wards of Shahid Rajaie Hospital. The program was conducted since March to August 2015. All of the patients which were on Imipenem, Meropenem, Linezolide or Teicoplanin as an empiric treatment or based on culture results were considered in the study. The results of this study indicated that among 136 in-patients who had taken at least one of these antibiotics including Imipenem, Meropenem, Linezolide or Teicoplanin, antimicrobial prescription assumed inappropriate for 63 patients (46.32%), The most common reason was incorrect dosage (16.39%)and the least one was not being drug of choice(2.4%).this inappropriateness was occurred mostly in diagnosis of respiratory infection , skin infection and sepsis. The results of this study demonstrates the need for revision in program of prescribing antibiotics in the direction of using antibiotic practice guidelines especially regarding usage of Teicoplanin and Meropenem in specific complication such as respiratory infection and skin infection.
Keywords
Carbapenems; Linezolid; Teicoplanin; Utilization; Evaluation
Download this article as:| Copy the following to cite this article: Farsad B. F, Hadavand N, Salehi H, Shekari F. Carbapenems, Linezolid, Teicoplanin Utilization Evaluation in a Large Teaching Based Hospital (Shahid Rajaie Heart Center, Tehran): A Quality Improvement Study. Biomed Pharmacol J 2016;9(2). |
| Copy the following to cite this URL: Farsad B. F, Hadavand N, Salehi H, Shekari F. Carbapenems, Linezolid, Teicoplanin Utilization Evaluation in a Large Teaching Based Hospital (Shahid Rajaie Heart Center, Tehran): A Quality Improvement Study. Biomed Pharmacol J 2016;9(2). Available from: http://biomedpharmajournal.org/?p=7617 |
Introduction
Drug Utilization Evaluation (DUE) studies are designed to evaluate appropriate drug usage. (1)These evaluations have been mostly focused on drugs with narrow therapeutic index ,high consumption rate and price, and also broad spectrum antibiotics such as Carbapenems, Linezolid and Teicoplanin. (2)In these evaluations, after identification of drug usage problems, interventions are implemented to improve the defects. New data need to be collected to determine if the identified drug use has been improved as a result of intervention then these finding will be available to the hospital staff .(3,4)
Irrational use of antibiotics has been a global concern. Especially in developing countries (5), numerous studies reported the inappropriateness use of 41-91% of all antibiotic prescriptions in teaching hospitals. (6)The factors that physicians should consider in selecting appropriate antibiotics include proper detecting source of infection, implementation of microbiological culture for definitive treatment, having enough information regarding antibiotics spectrum of actions, considering antibiotic with reasonable price in duration of therapy , considering host features and possible complication caused by antibiotics.(7) It is considerable to inform health care provider about antimicrobial stewardship for more cooperation. (8)
Prophylaxis or overuse of broad spectrum antibiotics may contribute to the emergence of bacterial drug resistance.(9) Increased antimicrobial resistance could be responsible for severe infections which doesn’t respond effectively to the antibiotics, complications, and increased length of hospital stays and mortality.(10) Several strategies have been presented to improve rational antibiotic usage in the hospitals,These include a restricted drug program, stop orders plan , antibiotic order forms, antibiotic therapy based on guidelines,and drug utilization evaluation. (11,12)
In this study, drug utilization was evaluated based on patients’ medical records with an objective to assess appropriate usage of critical antibiotics such as Carbapenems, Linezolid and Teicoplanin which have been identified as the last resort drugs. The other objective of this study was to identify prescriptions errors and to help reduce these errors.
Material and Method
This retrospective study was performed at special wards of Shahid Rajaie Hospital, Tehran, Iran. The program was conducted from March to August 2015. Post CABG adults older than 18 years in five different units including one ICU and four CCUs were included in this study. The selection of patients were according to their treatment with Imipenem, Meropenem, Linezolide or Teicoplanin as an empiric treatment or based on culture results. Ertapenem dosenot evaluated in this study. Patients who were identified to have allergy to studied medications, psychiatric illness, history of seizure, ClCr<20, pregnant and patients taking MAOI were excluded from this study. DUE forms were designed considering number of ordered and prescribed antibiotics, dosage and frequency of administration, indication for each antibiotic based on Mandell and IDSA and CDC guidelines and information about the patients such as serum creatinine,smoking,past medication history about studied antibiotics,past medical history such as heart or kidney disease. Medical records of patients investigated and necessary information were extracted.and some parameter such as ClCr calculated. Appropriate or inappropriate antibiotic prescriptions were evaluated according to factors such as dosage or duration (separately or combined), dosage adjustment in patients with renal impairment, antibiotic choice and indication. Descriptive analyses of clinical data were performed using SPSS statistical analysis software 20.
Results
A total of 136 in-patients were evaluated during a five month study,.demographic characterization of patients include general information , medical history ,antibiotic history ,duration of therapy and serum creatinine, has been presented in Table 1. 66.9%of population are males .almost half of patients had history of heart disease(46.32%).These patients were hospitalized at five special wards and they had taken at least one of the antibiotics including Imipenem, Meropenem, Linezolid or Teicoplanin . In this study, 14 patients who had known antibiotics usage indications were considered despite lack of sufficient data on dosage and duration of prescriptions.
Table 1: Demographic information
| Variables(N=136) | Results |
| Gender(M/F) | 91/45 |
| Mean AgeSD(years) | 55.519 |
| Mean WeightSD(kg) | 65.211.1 |
| Duration of Imipenem therapy | 6.674.07
|
| Duration of Meropenem therapy | 9.377.38 |
| Duration of Linezolid therapy | 8.84.3 |
| Duration of Teicoplanin therapy | 7.844.6 |
| Serum creatinine | 1.67 ± 1.58 |
| Smoking and Addiction | 45(33.08%)
|
| History of heart disease | 63(46.32%)
|
| History of MI | 9(6.61%)
|
| History of embolism | 18(13.23%)
|
| History of Dibetes mellitus | 14(10.29%) |
| History of kidney disease | 16(11.76%) |
| COPD | 4(2.94%)
|
| History of Carbapenems, linezolid or Teicoplanin exposure in hospital in past 3months | 37(27.2%) |
| Death/Alive | 62/74 |
The usage frequency and amount of studied antibiotics according to duration of treatment among 122 patients with sufficient data about prescribing state ,are shown in Table 2. These data demonstrate that Meropenem with 1028 consumed vial was the most frequent antibiotic used among the patients compared to the other antibiotics such as Imipenem, Teicoplanin and Linezolid which are ranked in the following places. The ratio of prescribed daily dose to DDD was also calculated according to Anatomic and therapeutic chemical classification system (ATC/DDD). Defined Daily Dose is the average maintenance dose of a drug used in a day as its main indication. Lower amount of prescribed daily dose to DDD can be seen obviously that means insufficient usage in all antibiotics.
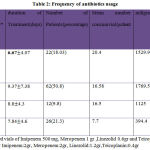 |
Table 2: Frequency of antibiotics usage
|
* Considered vials of Imipenem 500 mg, Meropenem 1 gr ,Linezolid 0.6gr and Teicoplanin 0.4gr
**DDD for Imipenem:2gr, Meropenem:2gr, Linezolid:1.2gr,Teicoplanin:0.4gr
Data presented in Table 3 shows that almost half of the drugs prescribed appropriately (n=59, 48.36%) while the rest of them were prescribed inappropriately (n=63, 51.63%) which means rate of consistency with reliable guidelines in each aspect of prescribing mentioned in this table. These data does not include the 14 patients with insufficient data on their method of prescription (n=14, 10.29%).There are significant differences in reasons of inappropriateness (p<0.05).The most common reason of inappropriate prescribing was improper dosage (n=20, 16.39%) which is more frequent in Meropenem (n=13,20.9%) compared to other antibiotics. Data also showed higher level of inappropriateness in duration of therapy individually (n=17, 13.93%)compared to dosage and duration of therapy together (n=13, 10.65%). Unreasonable dosing were identified in patients with renal insufficiency (n=8, 6.55%), mostly due to Teicoplanin (n=5.19.23%).Other reasons were incorrect drug choice (n=3, 2.4%) which is true only about imipenem(n=3,13.6%) and incorrect indication (n=5, 4.09%) .This table also includes the percentage of studied antibiotics inappropriateness in patients taking each drug.
Table 3: Prescription error reasons
| Causes
Antibiotics |
Imipenem%
(n=22) |
Meropenem%
(n=62) |
Linezolid%
(n=12) |
Teicoplanin%
(n=26) |
Total%
(n=122) |
| Appropriate prescription | 68.18 | 41.9 | 66.7 | 38.46 | 48.36 |
| Dosage and duration | 13.6 | 12.9 | – | 7.69 | 10.65 |
| Only Dosage | 4.5 | 20.9 | 16.7 | 15.38 | 16.39 |
| Only Duration | 9.09 | 14.51 | 8.3 | 19.23 | 13.93 |
| Dose adjustment in renal impairment | 4.5 | 3.2 | – | 19.23 | 6.55 |
| Indication | – | 6.45 | 8.3 | – | 4.09 |
| Choice | 13.6 | – | – | – | 2.4 |
| P=0.01 | |||||
Although there were not significant differences between wards (p=0.176),
data presented in Table 4 shows that almost half of the prescribing were inappropriate in all wards except PCCU-A (n=2,15.38%) which is likely due to few investigated patients. The most common inappropriate prescribing were observed in CCU-F (n=24, 53.33%) followed by ICU-A (n=17, 51.51%).
Table 4: The comparison of antibiotic prescribing in different wards
| Wards | Number of patients | Appropriate % | Inappropriate% | Insufficient data % |
| ICU-A | 33 | 39.39 | 51.51 | 9.09 |
| CCU-B | 23 | 52.17 | 43.47 | 4.34 |
| CCU-C | 22 | 54.54 | 45.45 | – |
| CCU-F | 45 | 37.7 | 53.33 | 8.8 |
| PCCU-A | 13 | 38.46 | 15.38 | 46.15 |
| P=0.176 | ||||
Overall condition of antibiotics prescribing can be seen in Table 5.meropenem has the most consumption among other antibiotics, this nessecitates more attention to be paid to its usage.There were not any significant differences among 4 studied antibiotics regarding inappropriateness (p=0.542), whereas it can be seen that the most inappropriate prescribing belongs to Teicoplanin (n=16,55.17%), followed by Meropenem (n=36,51.42%), Imipenem (n=10,41.6%) and Linezolid (n=4,30.76%) in the order of significance. It should be noted that evaluating guidelines adherence are based on number of errors rather than number of patients.
Table 5: Antibiotics usage overview
| Antibiotics | Appropriate % | Inappropriate % | Insufficient data % | Total consumption%
(n=136) |
| Imipenem
(n=24) |
62.5 | 41.6 | 8.3 | 17.64 |
| Meropenem
(n=70) |
37.14 | 51.42 | 11.42 | 51.47 |
| Linezolid
(n=13) |
61.53 | 30.76 | 7.69 | 9.55 |
| Teicoplanin
(n=29) |
34.48 | 55.17 | 10.34 | 21.32 |
| P=0.542 | ||||
Data in table 6 shows that among 136 patients, the majority of inappropriateness for Imipenem, Meropenem, Teicoplanin, were observed in respiratory infection indication, while sepsis ,abscess and UTI with equal percentages(4.16%) ,considered as the second place for Imipenem. Moreover Sepsis and skin infection held the second place for Meropenem and Teicoplanin,respectively For Linezolid, inappropriateness relates to diagnosis of respiratory infection, sepsis, chest infection (mediastinitis) and phlebitis with equal percentages
(7.69%).Overall, incorrect prescribing concerns are mostly in diagnosis of respiratory infection (n=24, 17.64%), sepsis (n=12, 8.82%) and skin
Infection (n=9, 6.61%) which have the most inconsistency with guidelines.
On the other hand the low rates of inappropriateness in Prophylaxis (n=2,1.47%) , Neutropenic fever (n=1,0.73%)and Phlebitis(n=1,0.73%)were due to limited prescribing in these indications.
Table 6: Antibiotics Inappropriateness rate according to pathogenesis
| Pathogenesis
Antibiotics |
Imipenem%
(n=24) |
Meropenem%
(n=70) |
Linezolid%
(n=13) |
Teicoplanin% (n=29) | Total inappropriateness%
(n=136) |
| Respiratory infection | 16.6 | 18.57 | 7.69 | 20.68 | 17.64 |
| Abdominal related infection* | – | 1.42 | – | 3.44 | 1.47 |
| Skin infection | – | 7.14 | – | 13.79 | 6.61 |
| Sepsis | 4.16 | 10 | 7.69 | 10.34 | 8.82 |
| Abscess | 4.16 | 1.42 | – | – | 2.2 |
| Urinary tract infection | 4.16 | 4.28 | – | – | 2.94 |
| Chest related infection ** | – | 4.28 | 7.69 | 3.44 | 3.67 |
| Prophylaxis | – | 2.85 | – | – | 1.47 |
| Neutropenic fever | – | – | – | 3.44 | 0.73 |
| Phlebitis | – | — | 7.69 | – | 0.73 |
*Abdominal infection includes: pancreatitis and cholesystitis
**Chest infection includes: endocarditits and mediastinitis
Table 7 shows prescribing condition of studied antibiotics,and distribution of total consumption of them in each infections .These antibiotics mostly prescribed in Respiratory infection (n=51,37.5%) with an equal percentage of adherenece and negligence to guidelines.(47.05%)
While usage of mentioned antibiotics in the prophylaxis was rare (n=2, 1.47%).
On the other hand ,consumption of antibiotics in abscess (n=3,100%),and prophylaxis(n=2,100%),had complete inconsistency with guidelines.This may be due to less prescribing in these indication. As well among 18 patients who took antibiotics for diagnosis of sepsis, most of prescribing was not according to guidelines(n=12,66.6%) this is also true about 5 out of 7 patients with mediastinitis Or endocarditis(n=5,71.42%).
Table 7: Antibiotics usage according to pathogenesis
| Pathogenesis
Appropriateness |
Appropriateness% | Inappropriateness% | Insufficient data % | Total consumption%
(n=136) |
| Respiratory infection(n=51) | 47.05 | 47.05 | 5.88 | 37.5 |
| Abdominal related infection * (n=11) | 45.45 | 18.18 | 36.36 | 8.08 |
| Skin infection(n=21) | 47.61 | 42.85 | 9.52 | 15.44 |
| Sepsis(n=18) | 27.7 | 66.6 | 5.55 | 13.23 |
| Abscess(n=3) | – | 100 | – | 2.2 |
| Urinary tract infection(n=15) | 60 | 26.6 | 13.3 | 11.02 |
| Chest related infection **
(n=7) |
28.57 | 71.42 | – | 5.14 |
| Prophylaxis(n=2) | – | 100 | – | 1.47 |
| Neutropenic fever(n=5) | 60 | 20 | 20 | 3.67 |
| Phlebitis(n=3) | 33.3 | 33.3 | 33.3 | 2.2 |
*Abdominal infection in appropriate prescribing includes pancreatic and ascites; for inappropriate prescribing includes cholecystitis and pancreatitis
**Chest infection includes mediastinitis and endocarditis
Discussion
The aim of this study is evaluating the way of prescribing of restricted and broad spectrum antibiotics such as Meropenem ,Imipenem,Linezolid and Teicoplanin according to standard guidelines ,and detecting fields of inappropriateness to help health care providers where to focus and therefore reducing the rapid emergence of resistant bacteria. Epidemiological studies have revealed that there was correlation between antibiotic consumption and emergence and spreading of resistant bacteria strains (13,14). Antimicrobial stewardship programs (ASPs) has important role in eradicating resistance strains (15).
In our study rate of inappropriate prescribing regarding Imipenem (n=10,41.6%) has been due to lack of consistency with antibiotics usage guidelines in selecting appropriate antibiotic and both dosage and duration of therapy (13.6%).On the other hand Meropenem wrong dosage (20.9%) is responsible for most unreasonable prescribing of this drug (n=36,51.42%). The most cases suffer from respiratory infections.
In a study conducted in Imam Hossein Hospital,in Tehran ,the rate of irrational use of Meropenem(59.3%)and Imipenem(53.4%) were similar to our study ,however inaccuracy is mostly due to unnecessary using of these antibiotics. Although this study uses the same guidelines(IDSA and Mandell),percentages of all causes of inappropriateness had not been mentioned distinctly as our study(16).
In Amir Hospital,in Zabol ,rate of imipenem inconsistency with indications that has been mentioned in AHFS guideline (92 %) was higher than all causes of inconsistency in our study (41.6%). Similar to our results, most frequent diagnosis for imipenem was pneumonia administered 1540mg/day in 8.08 ± 4.67days,which is near to our calculating (1529.9mg/day in 6.674.07days).
Compared to low rate of wrong imipenem dose adjustment in our studied renal patients (4.5%), there was 16% dosing error in this group of patients in Zabol Hospital (17). It can concluded that imipenem prescribing state in Rajaei Hospital is better than Zabol Hospital.
DUE which has been done in Shariati hospital in Tehran, demonstrates that 28% of critically ill patients have consumed inappropriate dose of carbapenems in CNS infections and menegitis, according to empric or culture based treatment (2). This rate is lower than our results about carbapenems inappropriateness (48.93%)among patients taking Imipenem and Meropenem .Differences compared to our study were; fewer evaluated wards (3ICUs), extended duration of study (1year) , type of study and studied population. In 3 months assessment of carbapenems utilization conducted in Abbotsford Regional Hospital, British Columbia, reveals that the rate of inappropriateness in empiric therapy of carbapenems is almost the same as our results (37%) mostly due to prescribing carbapenems without obvious infections. Meropenem most commonly used compared to other carbapenems.(85%).(18) As the same as our results that meropenem had higher rate of utilization (n=70.51.47%).Ertapenem has not been evaluated in our study despite of mentioned study.
Moreover meropenem had the second place in irrational usage (51.42%) after Teicoplanin(55.17%) mostly due to lack of consistency with available guidelines in dosage(20.9%)and duration of therapy (14.51%).Inattention to guideline indications had low rate (6.45%).Results extracted from Khan MU et al study which have evaluated meropenem utilization in teaching based hospital in Pakistan shows that meropenem usage as empirical therapy in 57%of cases was the major problem,whereas most adherence to the standard guideline was related to indication (97.52%) which is higher than our results (19). This study only evaluated meropenem with more attention to side effects of this drug on renal patients, also population and used guidelines differ from our study.
Evaluation of prescribing in our survey was based on frequency and amount of each antibiotic in duration of therapy.According to diagnosis and renal condition of Post CABG patients in special wards , there were different variables ,groups of patients and wards which has not been investigated like this in the past ,but we could not estimate the rate of emprical or according to culture treatment.
Linezolid has the least common antibiotic usage (n=13,9.55%) and the least inappropriateness (30.76%) among four studied antibiotics, mostly due to the lack of consistency with available guidelines in dosage (16.7%) and in diagnosis of respiratory infection,sepsis,chest infection(mediastinitis )and phlebitis with equal percentages (7.69%).
In study which was done in selected Canadian provinces by Walker S et al,
linezolid has been prescribed appropriately in approximately 50% of 95 patients , most commonly in Skin and soft tissue infections (32%) (20).The difference of this study is focusing in linezolid appropriateness but our study evaluated inappropriateness and their reasons. Certain comments about linezolid prescribing state was not possible due to few number of studied patients.
Most inappropriateness was seen in teicoplanin with 55.17% irrational usage mostly due to error in both dose adjustment in renal patients and duration of antibiotic treatment(19.2%) in pneumonia pathogenesis.These results can be compared with Hamishehkar et al study ,which teicoplanin consumption considered irrational in febrile neutropenic cancer patients due to unnecessary utilization in patients without renal impairment(47%) (21).The mean number of vials consumed per patient for meropenem and teicoplanin was the same (16.5) considering vial1gr for meropenem in 9.377.38 duration of treatment and vial 400 mg for teicoplanin in 7.844.6 duration of treatment, which is higher than mean number of 200mg vials of teicoplanin consumed per patient had been evaluated in the hospital at spain ( 30.8) in longer period of treatment(13.94 ± 10.82 ) used for gram-positive infections (22). The results of this study demonstrated higher teicoplanin cost of therapy compared to vancomycin.As in Iran higher price of teicoplanin makes vancomycin more cost effective (21). Utilization of more amount of teicoplanin in lower duration of treatment can be the reason of microbial resistance outbreak (23). On the other hand the most errors in renal dose adjustment among four studied antibiotics belong to teicoplanin therefore we can conclude that strict policies and strategies need to be implemented for teicoplanin use and dose adjustment specially in renal impairment patients according to standard guidelines.
Conclusion
Drug Utilization Evaluation (DUE) was found to be an effective approach to identify inappropriate prescribing and to improve rational use of antibiotics. Consumption of broad spectrum antibiotics especially meropenem should be restricted in dosage and duration and also it should be justified according to guidelines. Most inconsistency regarding teicoplanin was in renal dosage adjustment and this issue needs ASPs. Although linezolid had lowest degree of consumption and incorrect prescribing, usage of this drug should be with caution due to its special place as the last resort antibiotics.
More inadherence to guidelines were observed in respiratory infection, sepsis and skin infection .Based on these observations, it is advisable to use antibiotics with adherence to standard guidelines and microbiology culture after empiric therapy.
References
- Mousavi S et al, Drug utilization evaluation of imipenem and intravenous ciprofloxacin in a teaching hospital, Iran J Pharm Res. 2013 Winter;12(Suppl):161-7.
- Mahini S et al, Carbapenem Utilization in Critically Ill Patients,Journal of Pharmaceutical Care 2013. 1(4):141-144.
- Brown EM, Guidelines for antibiotic usage in hospitals, J. Antimicrob. Chemother. (2002) 49 (4): 587-592.
- Grégoire JP et al,Effect of drug utilization reviews on the quality of in-hospital prescribing: a quasi-experimental study, BMC Health Services Research, 2006 Mar 14;6:33.
- Mao W et al, Systematic Review on Irrational Use of Medicines in China and Vietnam, PLoS One. 2015; 10(3): e0117710.
- Hogerzeil HV, Promoting rational prescribing: an international perspective, Br J Clin Pharmacol. 1995 Jan; 39(1):1-6.
- Leekha S et al,General Principles of Antimicrobial Therapy, Mayo Clin Proc. 2011 Feb; 86(2): 156–167.
- Doron S,Antimicrobial Stewardship, Mayo Clin Proc. 2011 Nov; 86(11): 1113–1123.
- Sutradhar K et al, Irrational Use of Antibiotics and Antibiotic Resistance in Southern Rural Bangladesh:Perspectives from Both the Physicians and Patients, Annual Research & Review in Biology, ISSN: 2347-565X,Vol.: 4, Issue.: 9 (01-15 May)
- Llor C et al, Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem, Ther Adv Drug Saf. 2014 Dec; 5(6): 229–241.
- Diamond Sh et al, Strategies for controlling antibiotic use in a tertiary-care paediatric hospital, Paediatr Child Health. 1997 May-Jun; 2(3): 181–186.
- Victor R et al, The Valium Project: Diagnostic restrictions as a utilization control in a Medicaid drug program, Health Care Financ Rev. 1984 Spring; 5(3): 133–138.
- Lee Ventola C, the Antibiotic Resistance Crisis, P T. 2015 Apr; 40(4): 277–283.
- Davies J, Davies D,Origins and Evolution of Antibiotic Resistance, Microbiol Mol Biol Rev. 2010 Sep; 74(3): 417–433.
- CR L et al,Strategies to minimize antibiotic resistance, Int J Environ Res Public Health.2013 Sep 12; 10(9):4274-305.
- Shoaei S et al, Vancomycin and Five Broad-spectrum Antibiotic Utilization Evaluation in an Educational Medical Center in One Year, Journal of Pharmaceutical Care 2014. 2(4):154-161.
- Mousavi S et al, Drug utilization evaluation of imipenem and intravenous ciprofloxacin in a teaching hospital, Iran J Pharm Res. 2013 Winter;12(Suppl):161-7.
- Janssen J, CARBapenem utilization evaluation in a large community hospital (CARBON): A Quality Improvement Study, Can J Hosp Pharm. 2015 Jul-Aug; 68(4): 327–331.
- Khan MU et al, Drug utilization evaluation of meropenem and correlation of side effects with renal status of patients in a teaching based hospital, Pak J Pharm Sci. 2014 Sep;27(5 Spec no):1503-8.
- Walker S et al, An Assessment of Linezolid Utilization in Selected Canadian Provinces, Can J Infect Dis Med Microbiol. 2006 May-Jun; 17(3): 177–182.
- Hamishehkar H et al, Utilization Evaluation of Antimicrobial Agents in Neutropenic Cancer Patients in a Teaching hospital: Urgent of Drug Utilization Evaluation Studies, Journal of Pharmaceutical Care 2014. 2(1):3-9.
- Portolés A et al, Health economics assessment study of teicoplanin versus vancomycin in Gram-positive infections, Rev Esp Quimioter. 2006 Mar;19(1):65-75.
- Patterson JE,Antibiotic utilization: is there an effect on antimicrobial resistance?, Chest. 2001 Feb;119(2 Suppl):426-30.
(Visited 1,191 times, 1 visits today)







