Manuscript accepted on :July 05, 2016
Published online on: --
Plagiarism Check: Yes
Maryam Dadashpour1 and Seyed Morteza Bagheri2*
1Resident of Radiology , Iran University of Medical Sciences, Tehran, Iran.
2Department of Radiology, Hasheminejad Kidney Center (HKC), Iran University of Medical Sciences, Tehran, Iran.
*Corresponding Author E-mail: smb_53@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/977
Abstract
Transrectal ultrasound-guided prostate biopsies (TRUSBx) are common and increasingly performed procedure. As this procedure can be complicated by infections, antibiotic prophylaxis is widely used around the world to minimize these complications, but there is no consensus on the most appropriate prophylaxis regimen. A total number of 412 patients who were referred fo TRUSBx, was devided randomely into two groups. Group 1 received routine antibiotic prophylaxis and Group 2 did not received Amikacin. Other premedications in both groups include ciprofloxacin, metronidazole, ceftazidime and povodine iodine gel. 2 days after biopsy, all patients were investigated about significant fever(≥38ºC). febrile patients were referred to urology clinic for further evaluation about acute prostatitis or septicemia. There was 210 patients in group A and 202 patients in group B. No significant difference was detected in mean age, prostatic volume, serum PSA level, re-biopsy rate and pathology report between two groups. Acute prostatitiswas developed in 2 patients (0.9%) in group A and 1 patient (0.5%) in group B that was not statistically significant.(P>0.05) Removing amikacin from ciprofloxacin-based antibiotic prophylaxis along with local povodine iodine would not put our patients in increased risk for infectious complications after TRUSBx.
Keywords
Transrectal Ultrasound; Prostate Needle Biopsy; Antibiotic Prophylaxis; Amikacine; Povodine Iodine
Download this article as:| Copy the following to cite this article: Dadashpour M, Bagheri S. M. Acute Prostatitis After Transrectal Ultrasound-guided Prostate Biopsy: Comparing Two Different Antibiotic Prophylaxis Regimen. Biomed Pharmacol J 2016;9(2). |
| Copy the following to cite this URL: Dadashpour M, Bagheri S. M. Acute Prostatitis After Transrectal Ultrasound-guided Prostate Biopsy: Comparing Two Different Antibiotic Prophylaxis Regimen. Biomed Pharmacol J 2016;9(2). Available from: http://biomedpharmajournal.org/?p=7664 |
Introduction
Transrectal ultrasound-guided prostate biopsy (TRUSBx) is currently the gold-standard method for diagnosis prostate cancer.(1) Using this test, early detection of prostate cancer have been possible and this has a role indecreasing death rates from prostate cancer in recent years.(2,3)
The most common indication for TRUSBx is elevated serum prostatic specific antigen (PSA) level.(4) Since using PSA as a markerin early detection of prostate cancer, the number of TRUS- guided biopsies have dramatically increases.(5,6)Extended core biopsy technique provided taking at least 10 core biopsies transrectally, so Infectious complications could occure after TRUSBx,including fever, UTI, acute prostatitis, epididymo-orchitis and even life-threatening septicemia.(8,7) Antibiotic prophylaxis before TRUSBx had been shown to reduce the infection rate significantly.For this reasons, antibiotic prophylaxis is now routinelyprescribed.(9,1)
Although there is no consensus about the drug of choice and duration of antibiotic prophylaxis, flouroquinolons especially ciprofloxacin are widely used berore TRUSBx because of their good penetration into prostatic parenchyma, wide coverage on colonic flora and coliforms,ease of use and abscense of major complications.other drugs such asaminoglycosides, metronidazole and coamoxiclave had been used as alternative or in addition to flouroquinolons.(2,3,10)The incidence of infectious complications have been minimized by these protocols, However they could not completely eliminate infection.(11,12)
Use of povodine iodine as local gel or suppository with other medications in some researches was successful to induce significant decrease of infection rate.(4,13)In our experience, as well, just after adding Povodine iodine to our multiple-drug regimen the infection rate after TRUSBx reached near zero. We concluded that Povodine iodine is the most effective part of regimen, along with its ease to use and lower price. On the other hand there is a possibility that using multiple IV and oral antibiotics could raise antibiotic prophylaxis beside their adverse effects (especially nephrotoxicity for Amikacin) and more expensive price. So this study was scheduled to adjust antibiotic prophylaxis regimen, maintaining the same low infection rate.
Patients and Methods
This was a double blind randomized clinical trial study that was performed on 412 patients in our hospital from April 2012 to February 2013 who had referred for prostate biopsy due to an elevated PSA or abnormal digital rectal findings. At first we enrolled all patients with a prostate biopsy in this time period(513)but a total of 119 patients didn’t come back for follow up, so were excluded from the study.
All patients received ciprofloxacine 500 mg two times per day and metronidazole 250 mg three times per day per oral from 3 days before and 500 mg intravenous ceftazidime at the morning of the biopsy.Patients then randomly were divided into two groups, one group received additional 500 mg intravenous amikacin as routine prophylaxis regimen in our hospital (group A) and the other group did not received it.(group B) We allocated the first day for routine regimen and the day after for new regimen and this was repeated respectively, so all patients in a certain day, was received the same prophylaxis regimen.For all patients 20 mg lidocaine 2% and 30 mgpovodine iodine 10% as local gelinjected into the rectum by a 5o ml gavage syringe and 5 minutes later, TRUSBx were done for them. Patients and the radiologist responsible for biopsy were blind about the type of prophlaxis regimen.
According to our biopsy protocol, each prostate systematic biopsy included 10 core needle biopsiesor 12 if prostate volume was more than 50 ml. If a suspicious hypoechoic mass was found during TRUS, then 1 to 2 targeted biopsies would be added. All biopsies were done by a 18 guage needle and automatic gun using a biopsy attachment on a transrectal5-9 MHz probe.Patients were followed-up for 2 days later for possible signs of infection including fever (oral temperature ≥38ºC), chills, dysuria and frequent urination. Patients with temperature ≥38ºC with or without other symptoms were referred to urology department to investigate about acute prostatitis.Diagnosis of acute prostatitis was made by significant fever after transrectal prostate biopsy and correlated rectal exam (large, warm and tender prostate) with or without WBC in U/A or positive U/C. Diagnosis of septicemia was made by positive blood culture.
All patients were provided with informed consent before the biopsy and all personal informations reserved private. According to multiple studies Povodine Iodine would decrease infection rate sufficiently and Amikacine is not an essential part of prophylaxis regimen for prostate biopsy worldwide. So we did not put our patients in an additional risk for infectious complications,Howeverthe study protocol was approved by the Ethics Committee. Data analysis performed by SPSS 16.0 (SPSS Inc., Chicago, Illinois, USA)using paired sample t-test and chi2 test.
Results
A total of 412 patients (210 in group A and 202 in group B) were included.Mean age of patients in group A and B was66.4 ± 9 and 65.9 ± 9 respectively. There was no significant difference in mean age as well as mean prostate volume and mean serum PSA level between two groups.(P>0.05) (table1)
Re-biopsy had been done in 6 patients of group A and 4 patients in group B and in other patients this was the first prostate biopsy. The mean number of cores obtained in two group was nearly similar.Additionally pathology reports showed that 36% of patient in group A and 35% in group B was diagnosed as adenocarcinoma. These differences were not significant as well.(table1)
Table 1: Demographic data of patients
| Group A | Group B | P-value | |
| Mean age | 66.4 ± 9 | 65.9 ± 9 | 0.3 |
| Mean prostatic volume | 58 ± 31 | 56 ± 26.6 | 0.39 |
| Mean PSA(ng/ml) | 17.7 ± 33.6 | 17.14 ± 40.6 | 0.92 |
| Mean biopsy cores | 12 ± 2 | 12.2 ± 2 | 0.22 |
| Re-biopsy | 2% | 3% | 0.52 |
| Positive for Malignancy | 0.36 | 0.35 | 0.45 |
Fever more than 38ºC was detected in 2 patients in group A (0.9%) and in 1 patient in group B (0.5%) That was not significant.(p=0.58) (figure 1) Both 3 patients were referred to urology clinic and all of them were admitted in hospital. Mean age of affected patients was 62.6 years and one of them in routine prophylaxis group had been undergone re-biopsy.Blood and urine cultures were negative and rectal examination, fever and urine analysis in these patients was compatible with diagnosis of “Acute prostatitis”. Medical treatment was done with intravenous ciprofloxacin successfully and after mean hospitalization time of 5 days, all three patients left hospital with good general condition.
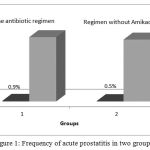 |
Figure 1: Frequency of acute prostatitis in two groups |
Discussion
Early prostate cancer detection programs with serum PSA have surprisingely increased the number of prostate biopsies.(2)TRUS-guided biopsy(TRUSBx) is generally a less invasive and safe method with some mainly minor complications. Infection is the most sever one that can caused hospitalization due to acute bacterial prostatits or septicemia. But fortunately the most common infectious complication is low grade fever due to transient bacteremia. The rate of infectious complications reported in different series ranges from 0.8% to 17% .(17,16,15)
Antibiotic prophylaxis before transrectal prostate biopsy is now a routine premedication and many researches revealed that it has significantly decreased the infection rate after prostate biopsy.(14,15) Although TRUSBx is a widely-used method, there is not a definite guideline about the type of antibiotic regimen and its duration. Fluoroquinilons are the most important part of prophylaxis and ciprofloxacin is the most used antibiotic as it quickly diffused in prostatic tissue to achieve concentrations several fold greater than the minimum inhibitory concentration for most coliforms.(14) Nevertheless the duration of ciprofloxacine usage is controversial and recent series has been shown that the therapeutic effect of a single dose ciprofloxacine is equivalent to 3 or 5-day regimen.(3,17,18)
Comparing the rate of infectious complications with other studies is rather difficult, as their different definition of infection and variety of antibiotics used for prophylaxis. In the study of AbuGhosh et al. rectal cleansing with povodine iodine in addition to ciprofloxacin caused 42% decrease in the risk of infectious complications including fever, urinary tract infection or sepsis comparing with ciprofloxacin alone, but it was not statistically significant.(19) However significant reduction has been published by park et al.(4) and Ghafoori et al. using povodine iodine suppository and gel respectively.In the study of park et al., a single intravenous injection of a 3rd generation cephalosporin just before biopsy and oral administration of cefixime (100 mg two times per day) begining at morning of the day of biopsy and for more 5 days.infectious complications was defined as fever, sepsis, acute prostatitis and UTI that developed in o.3% of patients with antibiotic prophylaxis and povodine iodine suppository. This result is quite similar to our study, noting this fact that our prophylaxis regimen was mainly different except of 3rd generation cephalosporin and use of povodine iodine.(4)
Madden et al. compare five different antibiotic regimen three of them contained ciprofloxacin and the other two did not. They demonstrated that eliminating ciprofloxacin from prophylaxis, would lead to significant increase in infection rate, as with 3 or 5-day ciprofloxacin alone, only 0.9% of patients were admitted for sever infective complications and just one patient out of 454 by sepsis,but in patients who received co-amoxiclave and gentamycin the rate of hospital admission was 4.7% and 7 patient developed sepsis.(14) on the other hand, adding amikacin to ciprofloxacin-based regimen significantly reduced the rate of infection (bacteremia and UTI) from 3.9% to 1.4%, but this was significant just for UTI. Authors concluded that adding amikacin to fluoroquinolone-based antimicrobial prophylaxis significantly reduces infection rate after prostate biopsy, particularly in populations where ciprofloxacin resistance is common. However, further studies would be done to confirm these findings.(12)
In our experience, ciprofloxacine was the main antibiotic that was administered for several years as prophylaxis, but two years ago our investigation revealed the rate of infectious complications was as high as 20% with two reports of septicemia so Hospital-acquired infection control committee decided to change the prophylaxis regimen as described above.Povodine iodine was included in our prophylaxis protocol since 1 year ago and due to our practice, as well as other studies,(13,4)rate of acute prostatitis reached to zero. This result along with nephrotoxicity of aminoglycosides especially in older patients (like patients referred for prostate biopsy) persuade us to investigate whether it is necessary to continue using amikacin. The result of this study proposed that removing amikacin from a prophylaxis regimen containing ciprofloxacin, ceftazidim and metronidazol in addition to povodine iodine would not increase the infection rate after prostate biopsy. The rate of acute prostatitis and hospitalization in our study was at the lowermost of range of the other studies. This could be justified by multiple antibiotics exists in our protocol and the low ratio of re-biopsy in our patients. More investigations is still needed to achieve the same low rate of infection but with the least systemic antibiotics.
References
- Adibi M, Pearle MS, Lotan Y. Cost-effectiveness of standard vs intensive antibiotic regimens for transrectal ultrasonography (TRUS)-guided prostate biopsy prophylaxis. B J U International. 2 011; 110 (2): 86-91.
- McConnell JD. Walsh PC, Wein AJ., Kavoussi p., Novik A.c., Partin A.W., Peters C.A, Campbell-Walsh Urology. 10th ed. Philadelphia: Elsevier Saunders; 2012:.
- Applewhite JC, Matlaga BR, McCullough DL, Craig Hall M, Transrectal Ultrasound and Biopsy in the Early Diagnosis of Prostate Cancer. Cancer Control March/April 2001; 8(2): 141-50.
- Park DS, Oh JI, Jin Ha Lee JH, et al. Simple Use of the Suppository Type Povidone-Iodine Can Prevent Infectious Complications in Transrectal Ultrasound-Guided Prostate Biopsy. Adv Urol. 2009;56:54-9.
- Mc Gahan JP, Goldberg BB. Diagnostic ultrasound. 2nd ed., Newyork: Informa Healthcare. 2008.
- Joseph C, Presti, Jr. Prostate Biopsy: Current Statusand Limitations. Reviews in urology. 2007; 9(3): 93-8.
- Zani EL, Clark OAC, Rodrigues Netto Jr N., Antibiotic prophylaxis for transrectal prostate biopsy (Review), The Cochrane Collaboration, 2011.
- Shigehara K, Miyagi T, Nakashima T, Shimamura M Acute bacterial prostatitis after transrectal prostate needle biopsy: clinical analysis. Infect Chemother. 2008 Feb;14(1):40-3.
- ARON M., RAJEEV T.P., GUPTA N.P., Antibiotic prophylaxis for transrectal needle biopsy of the prostate: a randomized controlled study, BJU International 2000, 85, 682-685.
- Lindert KA, Kabalin JN, Terris MK. Bacteremia and bacteriuria after transrectal ultrasound guided prostate biopsy. J Urol. 2000 Jul;164(1):76-80.
- Adibi M, Pearle MS, Lotan Y. Cost-effectiveness of standard vs intensive antibiotic regimens for transrectal ultrasonography (TRUS)-guided prostate biopsy prophylaxis. B J U International. 2 011; 110 (2): 86-91.
- Batura D, Rao GG, Nielsen PB, Charlett A. Adding amikacin to fluoroquinolone-based antimicrobial prophylaxis reduces prostate biopsy infection rates. BJU International.2010; 10 7: 760-64.
- Ghafoori M, Shakiba M, Seifmanesh h, Hoseini SK. Decrease in infection rate following use of povidone-iodine during transrectal ultrasound guided biopsy of the prostate: A double blind randomized clinical trial. Iran J Radiol. 2012; 9(2): 67-70.
- Madden T, Doble A, Aliyu SH, Neal DE. Infective complications after transrectal ultrasound-guided prostate biopsy following a new protocol for antibiotic prophylaxis aimed at reducing hospital-acquired infections. BJU International.2011; 108: 1597–602.
- Hori S, Sengupta A, Joannides A, Balogun-Ojuri B, Tilley R, McLoughlin J. Changing antibiotic prophylaxis for transrectal ultrasound-guided prostate biopsies: are we putting our patients at risk? BJU International.2010; 10 6: 1298 –1302.
- Wagenlehner FME, Oostrum EV, Tenke P, Tandogdu Z, Cek M, Grabe M. et al., Infective Complications After Prostate Biopsy: Outcome of the Global Prevalence Study of Infections in Urology (GPIU) 2010 and 2011, A Prospective Multinational Multicentre Prostate Biopsy Study. European Urology.2013; 6 3: 521–7.
- Tobias-Machado M., Corree TD, De Barros EL, Wroclawski ER. Antibiotic prophylaxis in prostate biopsy: A comparative randomized clinical assay between Ciprofloxacin and Chloramphenicol. International Braz J Urol. 2003; 29 (4): 313-19.
- Patel U, Kirby R. Infections after prostate biopsy and antibiotic resistance. B J U international. 2008 :1201-2.
- Puig J, Darnell A, Bermúdez P, Malet A, Serrate G, Baré M, et al. Transrectal ultrasound-guided prostate biopsy: is antibiotic prophylaxis necessary? Eur Radiol 2006; 16: 939–43.







