Manuscript accepted on :May 17, 2016
Published online on: 04-08-2016
Plagiarism Check: Yes
Saleh Maleki1, Parisa Falsafi2, Farzaneh Pakdel2, Hosein Eslami2, Ulduz Zamani Ahari1, Milad Ghanizadeh3 and Firouz Pouralibaba2*
1Post Graduate Student of Oral Medicine, Dental Faculty of Tabriz University, Tabriz, Iran.
2Department of Oral Medicine, School of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran. 3Post-graduated student of oral and maxillofacial surgery,Dental faculty, Tabriz university of medical sciences,Tabriz,Iran.*Corresponding Author E-mail: fpuralibaba@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/959
Abstract
The prevalence of diabetes and its complications encouraged the researchers to find effective ways with minimal side effects in order to diagnose and cure diabetes. The alpha-amylase and catalase are salivary enzymes which could be effective in this area. The salivary alpha-amylase inhibitors reduce the absorption of complex carbohydrates and so are effective in the diagnosis of diabetes by controlling blood sugar and measurement of the concentration level of salivary alpha-amylase. Besides, the catalase deficiency is associated with oxidative effects of diabetes. The improvement in the level of catalase reduces the diabetes complications. Due to lack of studies and conflicting results regarding this topic, the present study aims to compare the level of catalase and salivary alpha- amylase in patients with diabetes type I with non-diabetic people. In the present descriptive analytic study, the unstimulated saliva belong to 40 patients affected by type 1 diabetes and 40 non-diabetic people was gathered. The amount of alpha-amylase and salivary catalase in diabetic and non-diabetic people was separately evaluated. The data obtained from the study was analyzed by descriptive analytical approaches. The T-test and SPSS.21 were also applied for independent groups. The average of salivary catalase enzyme was 447.9 ± 143 KU/I in patients affected by diabetes and 283.7 ± 229.7 KU/I in non-diabetic patients. The average of salivary alpha-amylase enzyme was 150075 ± 158356.8 IU/mI in diabetic patients and 81825 ± 66742.2 IU/mI in non-diabetic patients (p<0.05). The level of salivary alpha-amylase and catalase in people affected by type 1 diabetes was higher than the non-diabetic people.
Keywords
Type 1 diabetes; saliva; catalase; alpha-amylase
Download this article as:| Copy the following to cite this article: Maleki S, Falsafi P, Pakdel F, Eslami H, Ahari U. Z, Pourali baba F, Ghanizadeh M. A Comparison Between Catalase and Salivary Alpha-Amylase Level in Patients with Type I Diabetes and Non-Diabetic People. Biomed Pharmacol J 2016;9(2). |
| Copy the following to cite this URL: Maleki S, Falsafi P, Pakdel F, Eslami H, Ahari U. Z, Pourali baba F, Ghanizadeh M. A Comparison Between Catalase and Salivary Alpha-Amylase Level in Patients with Type I Diabetes and Non-Diabetic People. Biomed Pharmacol J 2016;9(2). Available from: http://biomedpharmajournal.org/?p=7403 |
Introduction
Diabetes is a group of common metabolic disorders with hyperglycemia phenotype which leads to an initial decrease of insulin, reduced biological effect of insulin or both of them., The pancreatic β cell destruction or dysfunction occur in type I diabetes which leads to full or almost full deficiency of insulin (1, 2). With the increasing incidence of diabetes and its complications, the researchers’ efforts to find effective ways with minimal side effects for diagnosis and treatment of diabetes are still advancing (1, 3). The saliva as an accessible clinical sample has been in the spotlight of the researchers’ attention due to it’s the possession of different enzymes and molecules and distinctive function for the diagnosis and treatment of various diseases and their complications (6-3). Moreover, the evaluation of salivary samples has many advantages over serum since it is easy and cost-effective to collect and store and bears the minimal risk compared to other methods. It could be an economical and non-invasive method for screening of large populations (4, 5).
The alpha-amylase is a salivary enzyme belonging to glycoside hydrolase family which is topically produced in the oral cavity by salivary glands and mainly parotid gland and its biological function is digestion of macromolecules such as carbohydrates and starch (3, 6, 7).Various studies have indicated that the use of salivary alpha-amylase inhibitor with reduced absorption of complex carbohydrates could be effective in controlling blood sugar (6, 8, 9) and measurement of salivary concentration of alpha-amylase and so the diagnosis of diabetes (3, 4). The results of various studies on the changes of this enzyme in saliva of patients effected by diabetes is different. Panchbhai noted in a study that the level of salivary alpha amylase is reduced in controlled diabetic patients (3). Aydin indicated in another study that the concentration of this enzyme increases in diabetic patients (4). However in another study Kim said that the amount of this enzyme in the saliva of experimental rats under diabetic conditions reduces (10). Carda indicated that the level of salivary alpha- amylase of diabetic patients remained unchanged (5).
On the other hand, certain evidences showed that complications of diabetes is associated with oxidative stress induced by production of free radicals (11, 12). Oxidative stress which is caused by an imbalance in antioxidant status is mainly defined as changes in balance of prooxidants and antioxidants to form prooxidants which eventually lead to tissue damage (12, 13). The body’s defense mechanisms of antioxidant enzyme in saliva such as catalase usually encounter these effects (11, 14, 15). Catalase is a haemoprotein with four groups of peroxidase activities (16). Earlier studies showed that catalase deficiency is associated with complications of oxidative diabetes and catalase improvement reduces subsequent complications (14, 15, 17). The scientific examination of electronic resources and data banks of Pubmed, Ebsco and Google Scholar detected no study on the determination of salivary catalase level in diabetic people affected by type 1 diabetes. Mussavira et al. showed that the level of salivary catalase in patients affected by type 2 diabetes is less than non-diabetic people (12). Ibuki et al. (11) as well as Leite et al. (12) indicated in a separate study that level of salivary catalase amongst experimental rats under induced diabetic conditions would increase. With regard to the above examples and limited and contradictory studies in this era, it seems that precise evaluation of salivary samples in diabetic people in terms of enzyme changes such as salivary alpha-amylase enzyme and changes in the defense mechanism of anti-oxidant could be helpful in diagnosis, prognosis and treatment of diabetes. Therefore the present study was planned and conducted with the purpose of comparative examination of salivary catalase and alpha-amylase level between people affected by type 1 diabetes and non-diabetic people
Materials and Methods
The present analytic-descriptive study included a statistical population of 20-50 years individuals referred to Department of Oral Medicine, School of Dentistry in Tabriz. Among the total population, 40 people affected by type 1 diabetes and 40 non-diabetic people were randomly selected. The people under study were uniformed in terms of age and sex. The type of diabetes was determined on the basis of medical treatment history of patients, disease control methods, average glucose level and history of smoking and alcohol through study of medical records and interviews with people. However, all patients were insulin dependent due to the nature of their disease. The periodontal inflammation and other pathological conditions, systemic diseases that affect the salivary glands or saliva secretions, drug usage or oral or systematic diseases during the last three months, smoking or alcohol were criteria for exclusion of patients. The salivary samples were collected by Spitting method. In this way, the patient was allowed to collect saliva in the mouth and put it into a special sterile plastic tubes (falcon).This is usually done every 60 seconds for 15-5 minutes. The subject was asked to avoid eating, drinking or any oral stimulation for 90 minutes prior to the collection of sample so that an unstimulated sample will be obtained. Approximately 5 mL of saliva was collected using this method. The saliva was collected for all subjects between 8 to 9 a.m. (fasting) in order to avoid the circadian changes (6, 18). The saliva collected was immediately placed on ice and transported to the laboratory. It was centrifuged at 4 ° C for 10 min at 800 g so that the squamous cells and cellular debris were separated. The samples were frozen at -80 ° C until preparation of all samples is terminated (7, 18). Once all the samples were collected, necessary tests were implemented using prepared kits and atomic absorption spectrophotometry. The data was analyzed by descriptive statistical methods (mean± Standard deviation). The T-test and SPSS.21 were also applied for independent groups. The values lower than P<0.05 were statistically significant.
Results
The results of the present study showed that the average salivary catalase enzyme was 447.9± 143 KU/I for patients affected by type 1 diabetes and 283.7± 229.7 KU/I for non-diabetic people. The T-test for independent groups showed that this difference is statistically significant (P=0.13) and the patients affected by type 1 diabetes have higher level of salivary catalase. The average alpha-amylase level was 150075± 158356.7 IU/mI for patients affected by type 1 diabetes and 81825± 66742.2 IU/mI for non-diabetic people. The T-test conducted for independent groups also showed that this difference is statistically significant (P=0.001). The level of salivary alpha-amylase is higher in patients with type 1 diabetes.
Table 1: Comparison of salivary catalase and alpha-amylase level in diabetic and non-diabetic people
| Number | Catalase Enzyme | Alpha-amylase Enzyme | |
| Diabetic People | 40 | 143 ± 9/447 | 8/158356 ± 150075 |
| Non-diabetic People | 40 | 7/229 ± 7/283 | 2/66742 ± 81825 |
 |
Figure 1: Comparison of salivary catalase level in diabetic and non-diabetic people
|
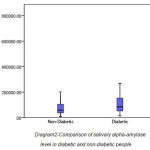 |
Figure 2: Comparison of salivary alpha-amylase level in diabetic and non-diabetic people
|
Discussion
The salivary glands function, molecular level and salivary enzymes experience changes in diabetic people. Therefore, the patients’ salivary compounds especially enzymes could be reliably considered in the diagnosis and prognosis of diabetes (19). Different studies with various results have been conducted on salivary compounds of people with diabetes based on the type of diabetes, their different metabolic control and other factors (3, 5, 12, 17, 20). The present study compares the unstimulated salivary sample of 40 people with type 1 diabetes and 40 non-diabetic people in terms of catalase enzyme and alpha-amylase level. The results showed that the level of salivary alpha-amylase level in patients with type 1 diabetes was significantly higher than non-diabetic people. Panchbhai et al. (2010) conducted a study on 80 people affected by IDDM and NIDDM. They found that the level of salivary alpha amylase in controlled diabetes will decrease (3). Aydin et al. (2007) conducted a study on 20 people affected by type 2 diabetes and reported that the concentration of alpha-amylase enzyme in diabetic patients will increase (4). Lopez et al. (2003) studied 20 children in 3-15 age range affected by type 1 diabetes. Rezinck et al. (2006) examined the 13-19 years patients affected by type 1diabetes and reported similar results (21, 22). Kim et al. showed that the level of this enzyme in saliva of experimental rats under induced diabetic condition will decrease (10). Carda et al. (2006) also conducted another study on 17 patients affected by type 2 diabetes and found that the level of alpha-amylase in diabetic people exhibited no change compared to control group (5).
Recent studies have shown that increased permeability of the base membrane in salivary glands especially parotid in diabetic patients leads to the penetration of salivary proteins such as amylase (23). Piras showed that annular receptor expression levels of amylase in diabetic patients will increase (24).These aforesaid cases could be considered as possible causes of increasing salivary amylase amongst diabetes people.
The present study also indicates that the level of salivary catalase enzyme in people affected by type 1 diabetes was significantly higher than non-diabetic people. This finding confirms the presence of oxidative stress in diabetic patients and increased function of saliva antioxidant defense system to deal with stress. Reznick et al. (2006) conducted a study on 20 patients affected by type 1 diabetes in 13-19 age range. They came to the conclusion that the level of salivary antioxidant (peroxidase, superoxide dismutase and total antioxidant capacity) increased. They reported that increment of HbA1C level leads to the increased level of antioxidant (22). Ibuki et al. (2010) as well as Leite et al. (2010) (14) implemented separate studies and found that the level of salivary catalase in experimental rats under induced diabetic condition will increase. However, the study by Gümüş et al. (2009) conducted on 60 diabetic people indicated that the level of antioxidant activity (Glutathione oxidase) in the saliva of diabetic people was lower than healthy people (25). Mussavira et al. showed that the level of salivary catalase in patients affected by type 2 diabetes was lower than non-diabetic people (12). Such differences could be due to the different methods of saliva sampling (unstimulated or stimulated with paraffin), different ways of examining the laboratory salivary samples, different age averages amongst patients, different affliction time required to be affected by diabetes and different metabolic control in patients. The restrictions of present study include impossibility of making the samples uniform in terms of physiological, hormone, nutrition and environmental conditions, local oral status, state of disease control, medication and level of blood sugar. In addition, diabetes is a multifactorial disease and a variety of factors including genetics, nutrition and environmental conditions play important role in its development. Also, the quantity and quality of saliva compositions could be influenced by individual genetic basis, amount and type of food, smoking, physical activity level, hormone structure and level of stress. Accordingly, implementation of further studies with larger population and further consideration of confounding factors is recommended in order to achieve diagnostic and therapeutic protocols for diabetic patients.
Conclusion
The level of alpha-amylase and catalase enzyme in patients affected by type 1 diabetes is higher than non-diabetic people.
References
- Association AD. Diagnosis and classification of diabetes mellitus. Diabetes care. 2010;33(Supplement 1):S62-S9.
- Mellitus D. Diagnosis and classification of diabetes mellitus. Diabetes care. 2005;28:S37.
- Panchbhai AS, Degwekar SS, Bhowte RR. Estimation of salivary glucose, salivary amylase, salivary total protein and salivary flow rate in diabetics in India. Journal of oral science. 2010;52(3):359-68.
- Aydin S. A comparison of ghrelin, glucose, alpha-amylase and protein levels in saliva from diabetics. Journal of biochemistry and molecular biology. 2007;40(1):29-35.
- Carda C, Mosquera-Lloreda N, Salom L, Gomez de Ferraris ME, Peydro A. Structural and functional salivary disorders in type 2 diabetic patients. Medicina oral, patologia oral y cirugia bucal. 2006;11(4):E309-14.
- Tundis R, Loizzo MR, Menichini F. Natural products as alpha-amylase and alpha-glucosidase inhibitors and their hypoglycaemic potential in the treatment of diabetes: an update. Mini reviews in medicinal chemistry. 2010;10(4):315-31.
- Ademiluyi AO, Oboh G. Soybean phenolic-rich extracts inhibit key-enzymes linked to type 2 diabetes (alpha-amylase and alpha-glucosidase) and hypertension (angiotensin I converting enzyme) in vitro. Experimental and toxicologic pathology : official journal of the Gesellschaft fur Toxikologische Pathologie. 2013;65(3):305-9.
- Melzig MF, Funke I. [Inhibitors of alpha-amylase from plants–a possibility to treat diabetes mellitus type II by phytotherapy?]. Wiener medizinische Wochenschrift (1946). 2006;157(13-14):320-4.
- Rayar A, Manivannan R. IN-VITRO ALPHA-AMYLASE AND ALPHA-GLUCOSIDASE INHIBITION ACTIVITY OF UMBELLIFERONE AND BETA-IONONE ISOLATED FROM CORIANDRUM SATIVUM LINN. 2015.
- Kim SK, Cuzzort LM, McKean RK, Allen ED. Effects of diabetes and insulin on alpha-amylase messenger RNA levels in rat parotid glands. Journal of dental research. 1990;69(8):1500-4.
- Ibuki FK, Simoes A, Nogueira FN. Antioxidant enzymatic defense in salivary glands of streptozotocin-induced diabetic rats: a temporal study. Cell biochemistry and function. 2010;28(6):503-8.
- Mussavira S, Dharmalingam M, Omana Sukumaran B. Salivary glucose and antioxidant defense markers in type II diabetes mellitus. Turkish journal of medical sciences. 2015;45(1):141-7.
- Dickinson D, DeRossi S, Yu H, Thomas C, Kragor C, Paquin B, et al. Epigallocatechin-3-gallate modulates anti-oxidant defense enzyme expression in murine submandibular and pancreatic exocrine gland cells and human HSG cells. Autoimmunity. 2014;47(3):177-84.
- Leite MF, Lima AM, Massuyama MM, Otton R. Astaxanthin restores the enzymatic antioxidant profile in salivary gland of alloxan-induced diabetic rats. Archives of oral biology. 2010;55(7):479-85.
- Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. The international journal of biochemistry & cell biology. 2007;39(1):44-84.
- Shaikh MA. Enzymes: a revaluation in textile processing. Pakistan Textile J. 2010:48-51.
- Rahimi R, Nikfar S, Larijani B, Abdollahi M. A review on the role of antioxidants in the management of diabetes and its complications. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 2005;59(7):365-73.
- Bakhtiari S, Bigom Taheri J, Bakhshi M, Mortazavi H, Shah Hoseini A, Vahid Dastjerdi E, et al. Effect of vitamin C on salivary total antioxidant capacity in smokers. Iranian journal of pharmaceutical research : IJPR. 2012;11(4):1045-9.
- Lawrence HP. Salivary markers of systemic disease: noninvasive diagnosis of disease and monitoring of general health. Journal. 2002;68(3):170-4.
- Bakianian Vaziri P, Vahedi M, Mortazavi H, Abdollahzadeh S, Hajilooi M. Evaluation of salivary glucose, IgA and flow rate in diabetic patients: a case-control study. Journal of dentistry. 2010;7(1):13-8.
- Lopez ME, Colloca ME, Paez RG, Schallmach JN, Koss MA, Chervonagura A. Salivary characteristics of diabetic children. Brazilian dental journal. 2003;14(1):26-31.
- Reznick AZ, Shehadeh N, Shafir Y, Nagler RM. Free radicals related effects and antioxidants in saliva and serum of adolescents with Type 1 diabetes mellitus. Archives of oral biology. 2006;51(8):640-8.
- Border MB, Schwartz S, Carlson J, Dibble CF, Kohltfarber H, Offenbacher S, et al. Exploring salivary proteomes in edentulous patients with type 2 diabetes. Molecular bioSystems. 2012;8(4):1304-10.
- Piras M, Hand AR, Mednieks MI, Piludu M. Amylase and cyclic amp receptor protein expression in human diabetic parotid glands. Journal of oral pathology & medicine : official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology. 2010;39(9):715-21.
- Gumus P, Buduneli N, Cetinkalp S, Hawkins SI, Renaud D, Kinane DF, et al. Salivary antioxidants in patients with type 1 or 2 diabetes and inflammatory periodontal disease: a case-control study. Journal of periodontology. 2009;80(9):1440-6.







