Manuscript accepted on :March 05, 2016
Published online on: 29-03-2016
Plagiarism Check: Yes
Javad Ramezani1, Mohammad Tayyebi2, Ali Eshraghi1 and Majid Jalal Yazdi3*
1Assistant Professor of Interventional Cardiology, Atherosclerosis Prevention Research Center, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran. 2Assistant Professor of Interventional Electrophysiology, Atherosclerosis Prevention Research Center, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran. 3Assistant Professor of Cardiology, Atherosclerosis Prevention Research Center, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran. Corresponding Author Email: jalalyazdim@mums.ac.ir
DOI : https://dx.doi.org/10.13005/bpj/931
Abstract
Aim of this study is to evaluate the effect of pre PCI administration of intracoronary nitroprusside on post procedural myonecrosis. Myonecrosis is a prognostically important complication of PCI. Nitric oxide is a potent vasodilator in the resistance arteriolar circulation, and plays a significant role in the control of coronary blood flow through the microcirculation. nitroprussideis a direct donor of nitric oxide. A total of 62 patients were randomized into the NTP (n= 31) or control (n= 31) group. Patients who were scheduled for non-urgent PCI in de novo native coronary arteries were eligible. All patients were pretreated with statin, aspirin and clopidogrel. Myonecrosis was measured by CK-MB elevation 24 h after PCI. The NTP group received intracoronary NTP befor PCI, whereas the control group did not. Results : All patients in NPT group received NTP for prevention of myonecrosis at a dose of at least 50 µg given intrcoronary through guiding catheter. 22 patients received 50µg,7 patients received 100µg and 3patients received 150µg. The baseline CPK-MB concentration was 16±4.89 and 16.55±6.18 in the control and NTP groups, respectively (P=0.70). The mean increase of CPK-MB concentration 24h after PCI was 20±26.64 and 10.13±14.35 in the control and NTP groups, respectively (P=0.06). Mean systolic BP before injection of NTP was 144.58±21.51mmHg and after injection of NPT was 121±21.51mm Hg. Bolus administration of NTP through the guiding catheter is associated with reduction in the occurrence of myonecrosis following non-urgent PCI in patients pretreated with dual antiplatelet agents and statins.
Keywords
Sodium Nitroprusside; Percutaneous Coronary Intervention; Periprocedural Myonecrosis
Download this article as:| Copy the following to cite this article: Ramezani J, Tayyebi M, Eshraghi A, Yazdi M. J. Effect of Intracoronary Sodium Nitroprusside Before Percutaneous Coronary Intervention on Periprocedural Myonecrosis : A Prospective Randomized Study. Biomed Pharmacol J 2016;9(1) |
| Copy the following to cite this URL: Ramezani J, Tayyebi M, Eshraghi A, Yazdi M. J. Effect of Intracoronary Sodium Nitroprusside Before Percutaneous Coronary Intervention on Periprocedural Myonecrosis : A Prospective Randomized Study. Biomed Pharmacol J 2015;9(1). Available from: http://biomedpharmajournal.org/?p=6643 |
Introduction
The use of percutaneous coronary intervention(PCl) to treat ischemic coronary artery disease (CAD) has expanded dramatically over the past three decades, In the absence of left main or diffuse multi vessel CAD, PCI is often the preferred method of revascularization. (1) Routine measurement of creatine kinase-MB isoform(CKMB) after PCI demonstrates periprocedural elevation in up to 40% of patients,which is almost always not associated with immediate clinical manifestations.(2,3) It was generally assumed that CK-MB elevation after cardiac manipulation is expected and, thus, a clear threshold above which elevation in cardiac markers is indicative of significant damage has not been accepted (4,5). It has been demonstrated that the risk of subsequent cardiac events (death or MI) is related to the extent of cardiac troponin or CK-MB increase(6,7).
Different strategies have been proposed and tested to prevent periprocedural MI (8,9). Several pathophysiological factors are implicated in myonecrosis but the majority of authors conclude that distal embolization of residual material of the unstable plaque during the procedure of percutaneous revascularization can result in myocardial necrosis (10). Nitroprusside (NTP) is a direct donor of nitric oxide(NO)(11).NO is an endothelium-derived compound that has multiple vascular functions, including vasodilation, inhibition of platelet adhesion and anti-inflammatory activity.(12) Therefore we hypothesis that NTP may be efficacious for prevention of myonecrosis through its action as a NO donor, vasodilation of microvessels, antiplatelet effects and anti-inflammatory. activity.
Methods
Trial design and randomization. This is a randomized, prospective, single-center study. Patients were randomize either to NTP and control group in a 1:1 ratio.
Patient population. From July 2010 to March 2011, 62 patients (age 40-79 years) with stable or unstable angina Who were scheduled to undergo non-urgent PCI of de novo native coronary lesions in a native coronary artery were randomized. Exclusion criteria included the following: complete occlusion resulting in Thrombolysis In Myocardial Infarction (TIMI) grade 0 antegrade flow, thrombus-laden lesions, significant left main coronary stenosis,balloon angioplasty without stenting, occurrence of myocardial infarction within one week, systolic BP<100mmHg, allergy to NTP, chronic renal failure, STEMI or stent thrombosis within 24h after PCI, intrastent restenosis, ostial lesion, lesions with extensive calcifications, positive biomarkers before PCI, Use of glycoprotein IIb/IIIa antagonists during PCI, fluoroscopy time >30 min,Side-branch compromised (TIMI flow<3) and any angiographic complications(see PCI procedure).
Adjunctive medications. All patients received a clopidogrel loading dose of 300 mg before the PCI (for loading dose administered more than 6 h prior to procedure), or 600 mg clopidogrel (for loading dose less than 6 h before procedure).
During catheterization, all patients received intravenous unfractionated heparin bolus 100U/Kg. Additional heparin boluses were given to maintain ACT>250 s. The ACT was measured 5 min after heparin administration. Post-procedural antiplatelet regimen consisted of aspirin 160 mg/day and clopidogrel 75 mg/day. All patients were on statins prior to PCI and were discharged on statins.
PCI procedure. Stents were implanted according to current clinical practice. Angiographic success was defined as a final angiographic residual stenosis of <20% by visual estimation. Procedural success was considered in cases of angiographic success and absence of any in-hospital major complication (acute MI, need for bypass surgery or repeat PCI, or death).The occurrence of angiographic complications during PCI was recorded. Angiographic complications included minor/major side branch compromise or occlusions, abrupt intraprocedural vessel closure, major arterial dissection, thrombus formation, transient and/or prolonged slow-no reflow, distal embolization, or coronary perforation. Patients randomized to the NTP group were given 50 µg of NTP (diluted into 5 ml normal saline) through the guiding catheter into the target coronary artery after guidewire advancement. For multi-vessel stenting, another 50 µg of NTP would be given after guide wire advancement for intervention of the subsequent vessel. Patients randomized to the control group did not receive NTP pretreatment, and the procedure was carried out in the usual manner
Hemodynamic analysis. Patients were continuously monitored during all procedures. Heart rates and blood pressures recorded before and after administration of NTP were determined. The data regarding any effects of intravessel NTP were analyzed to ascertain adverse clinical effects on cardiac hemodynamics.
Assessment
CK-MB (mass concentration) and cardiac troponin I (cTnI) were assessed before PCI using a radioimmunoassay analyzer. Abnormal baseline CK-MB and/or cTnI levels were exclusion criteria for enrollment into the study. CK-MB values were considered abnormal if they were elevated above the upper limit of normal (ULN). This is set at 25 mg/dl by our local laboratory.
Study end point. The primary end point of the study was to evaluate the incidence of myonecrosis (any elevation of CK-MB above25 mg/dl), in patients undergoing non-urgent PCI with or without pretreatment with intracoronary NTP. The secondary end point was any effects of intracoronary NTP to ascertain adverse clinical effects on cardiac hemodynamics.
Statistical Analysis
On the basis of a two-sided test size of 5% and a power of 80%, it was anticipated that a minimum of 62 patients would need to be recruited in each group to detect a difference in the incidence of myonecrosis of 20%. Continuous variables are presented as mean ± 1 SD or as median and interquartile ranges, as appropriate.Differences between groups in normally and non-normally distributed variables were assessed using the unpaired Student t test and the Mann-Whitney U test, respectively.Categorical variables were analyzed by chi-square test. All probability values were 2-tailed and a value of p< 0.05 was considered significant. Data were analyzed with SPSS for Windows version 16.0(SPSS Inc., Chicago,Illinois).
Results
Patient characteristics. A total of 62 patients (NTP group, n=31; control group, n= 31) were recruited into this study between July2010 to March 2011. There were no significant differences in the most relevant clinical and laboratory characteristics in the 2 groups. TG,LDL and HDL cholesterol levels at the time of the procedure were similar in the 2 groups. There were no differences in age, sex distribution, history of hyperlipidemia , smoking, diabetes mellitus, mean ejection fraction, hypertension, stable or unstable angina and history of Previous myocardial infarction between the 2 groups of patients. (Table1).
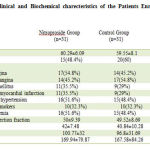 |
Table 1: Clinical and Biochemical charecteristics of the Patients Enrolled in the 2 Groups
|
Angiographic and procedural characteristics
Direct stenting was performed in 38.7% of cases in the NTP group and in 48.4% in the control group (p = 0.57). Directional or rotational atherectomy was performed in any patients in 2 group. Drug-eluting stents were implanted in 23(74.2%) and 27 (87.1%) patients in the control and NTP groups, respectively (P=0.88). Number of treated lesions/patient were 1.29±0.46 and 1.45±0.67 in the control and NTP groups, respectively (P=0.44).DES length (mm)/patient was 24.1±19.04 and 26.16±17.09 in the control and NTP groups, respectively (P=0.66). BMS length (mm)/patient was 4.74±8.52 and 6.03±9.04 in the control and NTP groups, respectively (P=0.54). All the other angiographic and procedural characteristics were similar in the 2 groups (Table2).
 |
Table 2: Baseline angiographic and procedural characteristics of patients by treatment
|
NTP Administration
All patients in NPT group received NTP for prevention of myonecrosis at a dose of at least 50 µg given intrcoronary through guiding catheter. 22 patients received 50µg,7 patients received 100µg and 3 patients received 150µg. Hemodynamic effects of NTP. Analysis of the hemodynamic data showed no evidence that NTP significantly altered patient blood pressure at the doses used (50 µg per injection).Mean systolic BP before injection of NTP was 144.58±21.51 mmHg and after injection of NPT was 121±21.51mmHg
Cardiac markers increase. The baseline CPK-MB concentration was 16±4.89 and 16.55±6.18 in the control and NTP groups, respectively (P=0.70). Patients undergoing NTP pretreatment tended to have lower myonecrosis than those without NTP. The mean increase of CPK-MB concentration 24h after PCI was 20±26.64 and 10.13±14.35 in the control and NTP groups, respectively (P=0.06)( Figure 1).
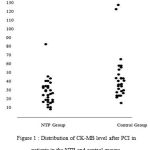 |
Figure 1: Distribution of CK-MB level after PCI in patients in the NTP and control groups.
|
This is the first randomized trial investigating the impact of NTP bolus pretreatment on the incidence of myonecrosis after non-urgent PCI. The power of this study for detecting difference between NPT and control group is 43%(α=0/05). The principle finding reported in this study was that intracoronary administration of NTP decreases the severity of myonecrosis after non-urgent PCI. Myonecrosis is a common sequel of percutaneous coronary intervention (PCI) (13). However, the incidence (3.6% to 48.8%) and magnitude of myocardial damage after PCI is highly variable, depending on the patient’s clinical, angiographic, and procedural characteristics; adjunctive pharmacotherapy; and the biomarker and thresholds applied to detect its presence (13).Possible mechanism of myonecrosis are prolonged balloon inflation ,side branch occlusion ,no reflow, distal embolization and coronary dissection.(14,15,16).Multilesion stenting, longer lesions, angulated lesion, prolonged inflation times, higher inflation pressure and number of stents are associate with increase cardiac enzyme in several studies.
(17,18,19,20). Pretreatment with statin and antiplatelet agents are straregies proven to reduce post-PCI myonecrosis.(21,22,23). Briguori et al. reported the lower rate of myonecrosis after a single high (80 mg) loading dose of atorvastatin administered within 24 h before stent implantation(Naples II Trial) (23). Patti et al. reported that loading with 600 mg of clopidogrel before PCI was associated with a significant reduction in the incidence of myonecrosis from 26 to 14%, compared with 300 mg loading(21). Chen et al. reported that despite adequate pretreatment with clopidogrel, patients with aspirin resistance as measured by a point-of-care assay have an increased risk of myonecrosis following non-urgent PCI (24). also lee et al. showed that Bolus administration of 50 mg of adenosine through the guiding catheter is associated with a 77% reduction in the occurrence of myonecrosis following non-urgent PCI in patients pretreated with dual antiplatelet agents and statins(25). Troponin is more sensitive than CK-MB in detecting smaller amounts of periprocedural myonecrosis, the prognostic implications of troponin elevation after PCI are less certain (26,27). In a study by Cavallini et al. troponin elevation was detected in 44% of patients undergoing PCI (vs. 16% CK-MB elevation) but, unlike CK-MB, did not predict 2-year mortality.
Is CK-MB elevation synonymous with myonecrosis
Recently, magnetic resonance scans of patients with peri-PCI CK-MB elevation demonstrated discrete areas of hyperenhancement (necrosis) in the PCI territory, which did not occur in patients without CK-MB elevation(28).Nitric oxide is an endothelium-derived compound that has multiple vascular functions, including vasodilation, inhibition of platelet adhesion and anti-inflammatory activity. Nitric oxide has been shown to act as a physiological inhibitor of leukocyteendothelial cell interaction by suppressing up-regulation of several endothelial cell adhesion molecules, including P-selectin, vascular cell adhesion molecule-1, and intercellular adhesion molecule-1 (29).Nitric oxide is a potent vasodilator in the resistance arteriolar circulation (12) and plays a significant role in the control of coronary blood flow through the microcirculation (30). Although nitrates have traditionally been used as donors of nitric oxide to maximally dilate coronary arteries, significant differences between epicardial arteries and resistance arterioles have been described with respect to the metabolism of vascular wall is necessary to derive nitric oxide. However, resistance arterioles are unable to metabolize nitroglycerin to nitric oxide as do large nonresistance vessels (31), and nitroglycerin is relatively less efficacious in eliciting dilation in microvessels compared with large, epicardial vessels. On the other hand, nitroprusside (NTP) is a direct donor of nitric oxide and is reported to require no intracellular metabolism to derive nitric oxide (11).NTP is a drug with short half-life(50 to 70 seconds)(32) and there are evidences that NTP does not significantly altered patient blood pressure and heart rate at the doses 50 to 200 µg per injection (33) Therefore we hypothesis that NTP may be efficacious and safe for prevention of myonecrosis through its action as a NO donor, vasodilation of microvessels, antiplatelet effects and anti-inflammatory activity. Yeh et al.reported that that NTP increased the caliber of both normal and stenosed coronary arteries in man and did not cause significant changes in heart rate or blood pressure(34). Parham et al. reported that intracoronary NTP (at doses up to 0.9 µg/kg) could produce coronary hyperemia (with increases in coronary blood flow) equivalent to that found with intracoronary adenosine. The hyperemic response to NTP was fast (peak coronary blood flow within 20 seconds from NTP bolus),and even more prolonged than with adenosine (up to 1 minute with NTP compared with 25 seconds with adenosine)(35). Interestingly, the decrease in systemic blood pressure observed in our study was similar to or smaller than that reported in previous studies using lower NTP doses delivered through the guiding catheter (36,37).
Study limitations. The study was not blinded. We can only speculate on the possible cardio protective mechanisms
of intracoronary NTP. The sample size is relatively small. If we had a larger sample size our result would be more significant. The Route of administration of NTP in this study was via guiding catheter. Route of administration via distal balloon delivery for selectively administrating NTP into the distal coronary bed is more reliable.
Conclusions
Bolus administration of NTP through the guiding catheter is associated with reduction in the occurrence of myonecrosis following non-urgent PCI in patients pretreated with dual antiplatelet agents and statins. Further studies are required to investigate the reduction of myonecrosis with NPT and short and long term morbidity and mortality.
Acknowledgement
The author thank for our colleagues in cardiac catheterization laboratory of shahid modarres hospital,shahid beheshti university of medical science.
References
- J.Poma J et al.Precutaneous Coronary and Valvular Intervention,Libby P,O.Bonow R,L.Mann D,P.Zipes D,Braunwald E, .Braunwald’s heart Disease A Textbook of Cardiovascular Medicine SAUNDERS ELSEVIER Philadelphia,PA,USA8th ed,2005,1419
- Califf RM, Abdelmeguid AE, Kuntz RE, et al. Myonecrosis after revascularization procedures. J Am Coll Cardio 1998;31:241–51.
- Topol EJ, Ferguson JJ, Weisman HF, et al, for the EPIC Investigator Group. Long-term protection from myocardial ischemic events in arandomized trial of brief integrin beta3 blockade with percutaneous coronary intervention. Evaluation of Platelet IIb/IIIa Inhibition for Prevention of Ischemic Complications. JAMA 1997;278:479–84.
- Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986;314:1–6.
- Hake U, Iversen S, Sadony V, Jakob HG, Neufang A, Oerlert H.Diagnosis of perioperative myocardial necrosis following coronary artery surgery—a reappraisal of isoenzyme analysis. Eur J Cardiothorac Surg 1990;4:79–84. .
- Kong TQ, Davidson CJ, Meyers SN, Tauke JT, Parker MA, Bonow RO. Prognostic implication of creatine kinase elevation following elective coronary artery interventions. JAMA 1997;277:461– 6.
- Ellis SG, Chew D, Chan A, Whitlow PL, Schneider JP, Topol EJ.Death following creatine kinase-MB elevation after coronary intervention: identification of an early risk period: importance of creatine kinase-MB level, completeness of revascularization, ventricular function, and probable benefit of statin therapy. Circulation 2002;106: 1205–10.
- Steinhubl SR, Lauer MS, Mukherjee DP, et al. The duration of pretreatment with ticlopidine prior to stenting is associated with the risk of procedure-related non–Q-wave myocardial infarctions. J Am Coll Cardiol 1998;32:1366 –70.
- Ellis SG, Brener SJ, Lincoff AM, et al. Beta-blockers before percutaneous coronary intervention do not attenuate postprocedural creatine kinase isoenzyme rise. Circulation 2001;104:2685–8.
- Topol EJ, Yadav JS. Recognition of the importance of embolization in atherosclerotic vascular disease. Circulation 2000;101:570– 80.
- Bates J, Baker M, Guerra R, Harrison D. Nitric oxide generation from nitroprusside by vascular tissue— evidence that reduction of the nitroprusside anion and cyanide loss are required. Biochem Pharmacol 1991;42:S157– 65.
- Myers PR, Bannitt P, Guerra R, Harrison D. Characteristics of canine coronary resistance arterioles: importance of the endothelium. Am J Physiol 1989;257:H603–10 .
- Herrmann J. Peri-procedural myocardial injury: 2005 update. Eur Heart J 2005;26:2493–519.
- Califf RM, Abdelmeguid AE, Kuntz RE, Popma JJ, Davidson CJ,Cohen EA, Kleiman NS, Mahaffey KW, Topol EJ, Pepine CJ,Lipicky RJ, Granger CB, Harrington RA, Tardiff BE, CrenshawBS, Bauman RP, Zuckerman BD, Chaitman BR, Bittl JA, Ohman EM. Myonecrosis after revascularization procedures. J Am Coll Cardiol 1998;31:241–51.
- Erbel R, Heusch G. Coronary microembolization. J Am Coll Cardiol 2000;36:22-4.
- Bahrmann P, Werner GS, Heusch G, et al. Detection of coronary microembolization by Doppler ultrasound in patients with stable angina pectoris undergoing elective percutaneous coronary interventions.Circulation 2007;115:600–8.
- Amit Segev, Lorne E. Goldman, Warren J. Cantor, Aiala Barr, Bradley H. Strauss, Luke D. Winegard, Kim A. Bowman, Robert J. Chisholm. Elevated troponin-I after percutaneous coronary interventions: Incidence and risk factors Cardiovascular Radiation Medicine 5 (2004) 59– 63.
- Bertinchant JP, Polge A, Ledermann B, Genet L, Fabbro-Peray P,Raczka F, Brunet J, Poirey S, Wittenberg O, Pernel I, Nigond J.Relation of minor cardiac troponin-I elevation to late cardiac events after uncomplicated elective successful percutaneous coronary angioplasty for angina pectoris.Am J Cardiol 1999;84:51 – 7.
- Cantor WJ, Newby LK, Christenson RH, Tuttle RH, Hasselblad V,Armstrong PW, Moliterno DJ, Califf RM, Topol EJ, Ohman EM,SYMPHONY and 2nd SYMPHONY Cardiac Markers Substudy Investigators. Prognostic significance of elevated troponin I after percutaneous coronary intervention. J Am Coll Cardiol 2002;39: 1738–44.
- La Vecchia I, Bedogni F, Finocchi G, Mezzena G, Martini M, Sartori M, Castellani A, Soffiati G, Vincenzi M. Troponin T, troponin-I and creatine kinase-MB mass after elective coronary stenting. Coron Artery Dis 1996;7:535 – 40.
- Patti G, Colonna G, Pasceri V, Pepe LL, Montinaro A, Di Sciascio G.Randomized trial of high loading dose of clopidogrel for reduction of periprocedural myocardial infarction in patients undergoing coronary intervention: results from the ARMYDA-2 (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty) study. Circulation 2005;111:2099–2106.
- Pasceri V, Patti G, Nusca A, Pristipino C, Richichi G, Di Sciascio G, ARMYDA Investigators. Randomized trial of atorvastatin for reduction of myocardial damage during coronary intervention: results from the ARMYDA(Atorvastatin for Reduction of MYocardial Damage during Angioplasty) study. Circulation 2004;110:674–678.
- Carlo Briguori, MD, PHD, Gabriella Visconti, MD, Amelia Focaccio, MD, Bruno Golia, MD, Alaide Chieffo, MD, Alfredo Castelli, MD, Marco Mussardo, MD, Matteo Montorfano, MD,Bruno Ricciardelli, MD, Antonio Colombo, MDNovel Approaches for Preventing or Limiting Events (Naples) II Trial Impact of a Single High Loading Dose of Atorvastatin on Periprocedural Myocardial Infarction Journal of the American College of Cardiology 2009;07: 2157–63.
- Wai-Hong Chen, MBBS, Pui-Yin Lee, MBBS, William Ng, MBBS, Hung-Fat Tse, MD, FACC, Chu-Pak Lau, MD, FA Aspirin Resistance Is Associated With a High Incidence of Myonecrosis After Non-Urgent Percutaneous Coronary Intervention Despite Clopidogrel Pretreatment2004;12: 1122–6.
- Chi-Hang Lee, Adrian Low, Bee-Choo Tai, Melissa Co, Mark Y. Chan, Jimmy Lim,Yean-Teng Lim, and Huay-Cheem Tan Pretreatment with intracoronary adenosine reduces the incidence of myonecrosis after non-urgent percutaneous coronary intervention: a prospective randomized studyEuropean Heart Journal 2007; 28: 19–25.
- (b3-19) Cantor WJ, Newby LK, Christenson RH, et al. Prognostic significanc of elevated troponin I after percutaneous coronary intervention. J Am Coll Cardiol 2002;39:1738–44.
- Miller WL, Garratt KN, Burritt MF, Lennon RJ, Reeder GS, Jaffe AS. Baseline troponin level: key to understanding the importance of post-PCI troponin elevations. Eur Heart J2006;27:1061–9.
- Ricciardi MJ, Wu E, Davidson CJ, et al. Visualization of discrete microinfarction after percutaneous coronary intervention associatedwith mild creatine kinase-MB elevation. Circulation 2001;103: 2780–3. .
- Kubes P, Suzuki M, Granger DN. Nitric oxide: an endogenous modulator of leukocyte adhesion. Proc Natl Acad Sci U S A 1991;88: 4651–5.
- Kuo L, Chilian W, Davis M. Interaction of pressure-induced and flow-induced responses in porcine coronary resistance vessels. Am J Physiol 1991;261:H1706–15.
- Kurz M, Lamping K, Bates J, Eastham C, Marcus M, Harrison D.Mechanisms responsible for the heterogeneous coronary microvascular response to nitroglycerin. Circ Res 1991;68:847–55.
- Parham WA, Bouhasin A, Ciaramita JP, Khoukaz S, Herrmann SC, Kern MJ. Coronary hyperemic dose responses of intracoronary sodium nitroprusside. Circulation 2004;16:1236 –1243.
- William B. Hillegass, MD, MPH, Neal A. Dean, BA, Laurence Liao, MD, Rodney G. Rhinehart, MD, Paul R. Myers, MD, PHD, FACC, FSCAI Treatment of No-Reflow and Impaired Flow With the Nitric Oxide Donor Nitroprusside Following Percutaneous Coronary Interventions: Initial Human Clinical Experience Journal of the American College of Cardiology 2001;5: 1335–43.
- Billy K. Yeh, M.D., Ph.D.Arthur J. Gosselin, M.D. Paul S. Swaye, M.D.Parry B. Larsen, M.D.Thomas O. Gentsch, M.D.Ernest A. Traad, M.D.Anthony R. Faraldo, M.D. Sodium nitroprusside as a coronary vasodilator in manI. Effect of intracoronary sodium nitroprusside on coronary arteries, angina pectoris, and coronary blood flow1977; 5:610-616.
- Parham WA, Bouhasin A, Ciaramita JP, Khoukaz S, Herrmann SC, Kern MJ.Coronary hyperemic dose response of intracoronary sodium nitroprusside. Circulation 2004;109:1236 –1243.
- Hillegass WB, Dean NA, Liao L, Rhinehart RG, Myers PR. Treatment of no-reflow and impaired flow with the nitric oxide donor nitroprusside following percutaneous coronary interventions: initial human clinical experience. J Am Coll Cardiol 2001;37:1335–1343.
- Pasceri V, Pristipino C, Pelliccia F, Granatelli A, Speciale G,Roncella A, Pironi B, Capasso M, Richichi G. Effects of the nitric oxide donor nitroprusside on no-reflow phenomenon during coronary interventions for acute myocardial infarction. Am J Cardiol2005;95:1358–1361.







