Manuscript accepted on :February 29, 2016
Published online on: 20-04-2016
Plagiarism Check: Yes
Mossa Ahmadi and Seyyed Javad Hosseini Shokouh
Infectious Diseases Research Center, AJA Univercity of Medical Sciences, Tehran, IR Iran. Corresponding author Email: sjavadhsh@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/933
Abstract
Inappropriate use of AB in surgeries may result in AB resistance and increased costs. Hence, we performed this study to evaluate the congruence of prescribed AB for prophylaxis before surgery with those recommended by heath ministry and army hospitals in 2009. A random sample of patients (from Cardiosurgeri, Gynecology, General surgery, Urology and Neurosurgery) in army hospitals was selected and the age, sex, AB duration, physician specialty and type and dose of AB were evaluated; if it was completely in congruence with recommendation of health ministry or not. The descriptive, central and distribution results were shown. The mean age of patients was 38.7 years and 43.7% were male. Cephalosporin, metronidazole, and aminoglycosides were prescribed 81.3%, 19.5% and 10.8% of patients respectively. For most of cases (80.3%) AB treatment period was shorter than 24 hours. Cephalosporins and Metronidazole were prescribed mostly by general surgeons (91.2% and 57% respectively) and Aminoglycosides were prescribed mostly by Gynecologist (91.2%). The prescription frequency based on physician specialty were statistically significant for all studied antibiotics. There was congruence in 79.5% in prescription, in 4.6% in AB type and in 48.2% AB treatment period. Totally 83.6% had no congruence with recommendation of health ministry. Excess and inappropriate use of AB for preoperative prophylaxis had a high rate in understudy hospitals. Therefore it is strongly recommended to pay more attention to physicians’ education about AB and the AB prescription supervisory committees and hospital infection committees act more active.
Keywords
Antibiotic; Prophylaxis; Surgery; Recommendation of health ministry
Download this article as:| Copy the following to cite this article: Ahmadi M, Shokouh S. J. H. Comparison of Antibiotic Prophylaxis Prescription Prior to Surgery Operations With National Instruction. Biomed Pharmacol J 2016;9(1) |
| Copy the following to cite this URL: Ahmadi M, Shokouh S. J. H. Comparison of Antibiotic Prophylaxis Prescription Prior to Surgery Operations With National Instruction. Biomed Pharmacol J 2015;9(1). Available from: http://biomedpharmajournal.org/?p=6765 |
Introduction
Antibiotics are among the most commonly used medicines that are utilized to treat many diseases. The most important application is to eradicate infectious diseases and preventing transmission from one to another. As the most selling medicine, misusing AB has caused many difficulties so far among of which microorganism resistance is the most important. Microorganism resistance is a global concern today and according to many observations AB overuse caused resistant strains development such as Staphylococcus aureus, Entrococ, Entrobacteriaceae and Pneumococ that have been reported in recent decades because of incorrect AB utilization strategies (1).
In order to microorganism resistance decrement it is strongly suggested that AB must be used with determined indications. This means AB should be prescribed based on cultures and antibiogram tests and for emergencies, it should be based on prescription experimental standards. This could lead to appropriate AB prescription and defined indications could decrease AB misuses and overuses.
Hospital acquired infections in association with hospitals extension, emerging and re-emerging diseases such as Aids and microbe resistance enhancement have been always one of hygiene and treatment main issues and by increscent of patient staying period the risk of morbidity and mortality enhances because of nosocomial infections thus hospital costs raises dramatically (2).
Clearly by successful identifying pathogens that cause nosocomial infections, disease transmission, microbe resistance patterns, antiseptic and sterilizing material application and prevention methods these infections could be controlled effectively.
Based on WHO’s report on October 2005, over 1.4 millions are suffering from nosocomial infections all over the world. In developed countries 5 to 10% of hospitalized patients catch nosocomial infections, while this increases up to 25% for developing countries.
Control program of nosocomial infections formed at the end of 1950’s in United States of America that initially focused on Staphylocuc infections. In next years through association of microbiology with epidemiology and statistics (3), theses programs became a determining parameter to evaluate treatment services quality in developed countries. The main role of these programs is to diminish nosocomial infections risk factors in hospitals so transmission risk of mentioned infections to patients, staffs, students and visitors are minimized. Nosocomial infections occur for at least 5% of patients in US that leads to 88000 deaths and force more than 4.5 billion dollars to healthcare treatments (4). For some countries with moderate income this economic waste increases approximately to 8 billion dollars. Therefore in 1970’s National Nosocomial Infections Surveillance System (NNIS) was founded in order to gather care information with united definition from volunteer hospitals in US (5). Hence variable strategies were taken among of which hands hygiene surveillance is the most important one (6).
Despite backgrounds of infection control since 1971 at Ahvaz and Shiraz universities and also some hospitals in Tehran, nosocomial infections control in Iran is not that long recorded (7-9). Nevertheless only in Shiraz a particular attention to control nosocomial infections since 1960 occurred and prevention and control programs have been followed seriously.
There are different kinds of nosocomial infections that in this article surgical site infection was assessed. This infection is defined as infection of any part of the body (except skin cutting location, fascia and muscle layers) that has been opened and manipulated through surgery. They are classified as follows: incision infection, organ infection and other organs that have been manipulated during the surgery. Surgical site infection is a morbidity source for patients whit surgery and using AB prior to the surgery (with indication) is a main part of surgery standard treatment (10).
Methods
Study method: This study was done as a descriptive cross-sectional assessment.
Statistical communitie: consisted of hospitalized patients in selected army hospitals in 2009.
Sampling method: was accessible type.
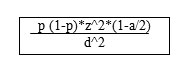
Sample volume: As it is showed bellow, according to the formula sample volume should be at least 400. In this study 600 samples were assessed.
Information gathering tools: by checklists and based on patients profile (existing data) were applied.
Inclusion and exclusion criteria: inclusion criteria was surgery and also completed patients profiles. Patients with fever occurrence and positive culture or any kind of need for AB using and also AB using prior for any reason but prophylaxis were excluded.
Description method and analyzing: after obtaining desired information, data has been analyzed by SPSS software, version 11.5. Chi-square test was used for this and significant level of 0.05 was determined to analyzing results. If AB proscription matched exactly as the national instruction it would be assumed as inconsonant otherwise inconsonant.
Variables: included age, sex, AB using period, physician specialty and type and dose of prescribed ABs.
Results
38.8 years was age average. 130 cases (21.7%) were cardiosurgeries including CABG (86 cases) and cardiovalve repair operations (44 cases), 342 cases belonged to women surgery operations (57%) including caesarian (88 cases), histerectomia (95 cases), ovary cysts (124 cases) and courtage (35 cases), 114 cases were general surgery operations (19%) including appendectomy (48 cases), hernia (35 cases), GI tumor (13 cases), cholecystectomy (18 cases) and 14 cases belonged to other operations (2.3%) including 4 cases of prostatectomy and 10 cases of craniotomy.
338 cases (56.3%) were female and 262 cases were male. Most of patients were over 60 years old (30.5%) and 20-30 years old (19.8%). The age groups frequency were 18.5%, 9.7%, 9.5%, 9%, and 3% for 10-20, 30-40, 40-50, 50-60, and 0-10 years old, respectively.
For 488 cases (81.3%) cephalosporin was prescribed. 117 cases (19.5%) were received metronidazole and aminoglycosides was prescribed for 65 cases (10.8%).
The frequency of physician specialty was evaluated in this study as well. Our results illustrated that most of physicians (57%) were gynecologist. Cardio-surgeon and General surgeon contained 21.7% and 19% of physicians, respectively. 2.3% were other specialists.
For most of cases (n=482, 80.3%) AB treatment period was shorter than 24 hours. Our results showed that 98 (16.3%), 16 (2.7), and 4 (0.7%) of patents received AB treatment for 2, 3, and 4 days, respectively.
The antibiotics prescription frequency were evaluated based on physician specialty as well. The results of this evaluation are shown in tables 1-3. According to the obtained results, Cephalosporins were prescribed mostly by general surgeons (91.2%) that there were a significant statistical value for them (P=0.0001) table 1.
Table 1: Cephalosporins prescription frequency based on physician specialty.
| Specialty | Cephalosporins utilization | Total | |
| Yes | No | ||
| Cardiosurgeon | 110
84.6% |
20
15.4% |
130
100% |
| Gynecologist | 255
77.5% |
77
22.5% |
342
100% |
| General surgeon | 104
91.2% |
10
8.8% |
114
100% |
| Other specialists | 9
64.3% |
5
35.7% |
14
100% |
| Total | 488
81.3% |
112
18.7% |
600
100% |
Our results indicated that Metronidazole were prescribed mostly by general surgeons (57.0%) that there were a significant statistical value for them (P=0.0001) table 2.
Table 2: Metronidazole prescription frequency based on physician specialty.
| Specialty | Metronidazole utilization | Total | |
| Yes | No | ||
| Cardiosurgeon | 7
5.4% |
123
94.6% |
130
100% |
| Gynecologist | 44
12.9% |
296
87.1% |
342
100% |
| General surgeon | 65
57.0% |
49
43.0% |
114
100% |
| Other specialists | 1
7.1% |
13
92.9% |
14
100% |
| Total | 117
19.5% |
483
80.5% |
600
100% |
Aminoglycosides prescription frequency based on physician specialty was evaluated as well. The results showed this antibiotic was prescribed mostly by Gynecologist (91.2%) that there were a significant statistical value for them (P=0.0001) table 3.
Table 3: Aminoglycosides prescription frequency based on physician specialty.
| Specialty | Aminoglycosides utilization | Total | |
| Yes | No | ||
| Cardiosurgeon | 0
0% |
130
100% |
130
100% |
| Gynecologist | 53
15.5% |
289
84.5% |
342
100% |
| General surgeon | 11
9.6% |
103
90.4% |
114
100% |
| Other specialists | 1
7.1% |
13
92.9% |
14
100% |
| Total | 65
10.8% |
535
89.2% |
600
100% |
At last step of this study, the AB treatment period was statistically analyzed based on the specialty of physicians. The statistical analysis did not shoq any significant relation betqeen AB treatment period frequency and physicaian specialty (P>0.05%) table 4.
Table 4: AB treatment period frequency based on physician specialty.
| Specialty | Day number | Total | |||
| 1 | 2 | 3 | 4 | ||
| Cardiosurgeon | 98
75.4% |
29
22.3% |
3
2.3% |
0
0% |
130
100% |
| Gynecologist | 272
79.5% |
54
15.8% |
12
3.5% |
4
1.2% |
342
100% |
| General surgeon | 100
87.7% |
13
11.4% |
1
0.9% |
0
0% |
114
100% |
| Other specialists | 12
85.7% |
2
14.3% |
0
0% |
0
0% |
14
100% |
| Total | 482
80.3% |
98
16.3% |
16
2.7% |
4
0.7% |
600
100% |
Discussion
Increasing bacterial resistance is linked with the volume of antibiotic prescribed, as well as missing doses when taking antibiotics (11). Inappropriate prescribing of antibiotics has been attributed to a number of causes, including people insisting on antibiotics, physicians prescribing them as they feel they do not have time to explain why they are not necessary, and physicians not knowing when to prescribe antibiotics or being overly cautious for medical and/or legal reasons (12). Up to half of antibiotics used in humans are unnecessary and inappropriate (13).
Antibiotic resistance increases with duration of treatment; therefore, as long as an effective minimum is kept, shorter courses of antibiotics are likely to decrease rates of resistance, reduce cost, and have better outcomes with fewer complications (14).
Improper use of antibiotics can often be attributed to the presence of structural violence in particular regions. Socioeconomic factors such as race and poverty affect accessibility of and adherence to drug therapy. The efficacy of treatment programs for drug-resistant strains depends on whether or not programmatic improvements take into account the effects of structural violence (15).
In this study it was revealed that AB taken by 579 cases (96.5%) included 488 cases of cephalosporins (81.33%), 117 cases of metronidazole (19.5%), 65 cases of aminoglycosides (10.8%) were prescribed in order to accomplish prophylaxis prior to the operation. Most of physicians were gynecologists (57%) and for most of cases (80.3%) AB treatment period was shorter than 24 hours. Cephalosporins and metronidazole were prescribed mostly by general surgeons while aminoglycosides were prescribed mostly by gynecologists. There was no relation between physician specialty and AB treatment period. In this study over and misusing of AB to accomplish prophylaxis prior to the operations were observed for 83.6% of cases (incompatibility with national instruction).
Similar to ours in a previous study in Shiraz by Askarian and Motaveji (2006) more than 85% incompatibility with national instruction was reported (16). Nevertheless in mentioned study 50% of patients received first dose of AB in an appropriate time while that happened for 79.3% of patients in this study. In prescribed dose number 7.3% matched with national instructions compatible to Shiraz’s. Cephalosporins prescription seems to be more frequent in Iran as it was revealed in Sari (2008) as well (16). Following study indicated that most common operations associated with AB prescription were gynecology surgeries. As it was reported by Alavi moghadam and et.al in 2005 from 200 files in Tehran, most common operations in association with AB prescription were gynecology and general surgeries (17). In this study the shortest period for AB using was 24 hours and there was no significant relation between physician specialty and AB treatment period that this subject has not been investigated in previous studies. It should be noticed that there was congruence in 79.5% in prescription, in 4.6% in AB type and in 48.2% AB treatment period. In a study by Anucha in 2006 it was indicated that the most common reason for prescribing wrong AB was inappropriate prophylaxis before the surgeries and it occurred more frequently in gynecology sections (18). This is compliant with following study in which gynecologists accompanied by cardio and general surgeons had the maximum rate of wrong AB prophylaxis prescription. In mentioned study it was concluded that consulting with infectious specialists diminishes AB inappropriate application.
Conclusion
Being cautious to identify accurate AB prescription and defined indications could lead to prescription and use decrement which causes AB resistance diminishing. Making decisions and planning in this area need assessment of AB prescription patterns in different countries primarily to indicate percentage of people who have taken incorrect AB prescription. According to this and also due to the importance of prophylactic AB prescription for surgery needed patients, this study was accomplished to compare AB prophylaxis prescription before the operations with national instructions in selected army hospitals in 2009. It should be mentioned that famous hospitals in the world in order to prevent irregular AB prescription that decreases treatment costs and resistant strains, have formed AB control strategy as a main part of their effort to control resistance.
References
- Amirthalingam S, Yi KS, Ching LT, Mun NY. Topical Antibacterials and Global Challenges on Resistance Development. Tropical Journal of Pharmaceutical Research. 2015;14(5):919-24.
- Saavedra C, Ordóñez K, Díaz J. [Nosocomial infections impact in a hospital in Bogota (Colombia): effects on mortality and hospital costs]. Revista chilena de infectologia: organo oficial de la Sociedad Chilena de Infectologia. 2015;32(1):36-40.
- Yahaghi E, Imani Fooladi AA, Amin M, Mirnejad R, Nezamzade R, Amani J. Detection of Class I Integrons in staphylococcus aureus Isolated From Clinical Samples. Iran Red Crescent Med J. 2014 November; 16(11): e16234.
- Rollins JA. Evidence-based hospital design improves health care outcomes for patients, families, and staff. Pediatric nursing. 2004;30(4):338.
- Klevens R, Edwards J, Tenover F, McDonald L, Horan T, Gaynes R. National Nosocomial Infections Surveillance System Changes in the epidemiology of methicillin-resistant Staphylococcus aureus in intensive care units in US hospitals, 1992-2003. Clin Infect Dis. 2006;42(3):389-91.
- Brunetti L, Santoro E, De Caro F, Cavallo P, Boccia A, Capunzo M, et al. Surveillance of nosocomial infections: a preliminary study on hand hygiene compliance of healthcare workers. Journal of preventive medicine and hygiene. 2015;47(2).
- McLaws ML, Momeni M, Oroei M, Danaei M, Askarian M, Palenik CJ, et al. Obstacles to Cytotoxic Waste Management Perceived by Nurses in Shiraz, Iran. Journal NI. 2015;1(2).
- Askarian M, Gooran NR. National nosocomial infection surveillance system–based study in Iran: Additional hospital stay attributable to nosocomial infections. American journal of infection control. 2003;31(8):465-8.
- Alaghehbandan R, Azimi L, Lari AR. Nosocomial infections among burn patients in Teheran, Iran: a decade later. Annals of burns and fire disasters. 2012;25(1):3.
- van Walraven C, Musselman R. The Surgical Site Infection Risk Score (SSIRS): a model to predict the risk of surgical site infections. PloS one. 2013;8(6):e67167.
- Koorosh Ahmadi, Amir Masoud Hashemian, Ehsan Bolvardi, Peyman Khadem Hosseini. Vancomycin-Resistant Pseudomonas Aeroginosa in the Cases of Trauma. Med Arch. 2016 Feb; 70(1): 57-60
- Arnold SR, Straus SE, Arnold S. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev. 2005;4(4).
- Tavasoli S, Zarnani AH, Vafa M, Moradi-Lakeh M, Pazoki-Toroudi H, Eghtesadi S. The effect of pomegranate extract on survival and peritoneal bacterial load in cecal ligation and perforation model of sepsis in rats. Int J Prev Med. 2014 Jan;5(1):104-9.
- Mashayekhi F, Moghny M , Faramarzpoor M, Yahaghi E , Khodaverdi Darian E, Tarhriz V, Dormanesh B. Molecular Characterization and Antimicrobial Resistance of Uropathogenic Escherichia coli. Iran J Biotech. 2014 June; 12(2): e16833.
- Farmer PE, Nizeye B, Stulac S, Keshavjee S. Structural violence and clinical medicine. PLoS Med. 2006;3(10):e449.
- Askarian M, Yadollahi M, Assadian O. Point prevalence and risk factors of hospital acquired infections in a cluster of university-affiliated hospitals in Shiraz, Iran. Journal of infection and public health. 2012;5(2):169-76.
- Alavi-moghadam M, Yadegarinia D, Zamiri SA. Studying the antibiotic prescription pattern in emergency department of Shahid Beheshti University of Medical Science affiliated hospital in 2009 (in Persian). Pajoohande. 2010;14(1):31-6.
- Apisarnthanarak A, Danchaivijitr S, Khawcharoenporn T, Limsrivilai J, Warachan B, Bailey TC, et al. Effectiveness of education and an antibiotic-control program in a tertiary care hospital in Thailand. Clinical infectious diseases. 2006;42(6):768-75.







