Manuscript accepted on :
Published online on: 19-11-2015
Plagiarism Check: Yes
Elham Sadeghi* and Sara Sadeghi
Department of Surgery, Medicine Faculty, Islamic Azad University Medical Beranch, Tehran, Iran
DOI : https://dx.doi.org/10.13005/bpj/638
Abstract
Facts and evidence hold out a steadily increasing prevalence of breast cancer in the mid-1940s. In most cases, the disease is discovered when the disease has reached an advanced stage, therefore, early diagnosis can significantly reduce the burden of disease. Breast cancer has some risk factors such as tumor size and lymph node involvement. The aim of this study was to evaluate the correlation between tumor size and axillary lymph node involvement and the prognosis for patients with breast cancer has been surgery. The study population consisted of 100 patients with breast cancer surgery at Shohada Hospital of Tajrish during the last 10 years. The results suggest that lymph node involvement was significantly associated with prognosis in patients with breast cancer and in cases where the tumor size was less than one centimeter, it has no impact on the prognosis of breast cancer. Also, a family history of the disease among close relatives is an independent risk factor for poor prognosis, in patients with breast cancer in general it can be said that involvement of lymph nodes in patients with breast cancer is due to an unfavorable prognosis; but the number of lymph nodes involved and the size of the tumor did not have any effect on the prognosis.
Keywords
tumor size; axillary lymph nodes; the prognosis; screening; breast cancer
Download this article as:| Copy the following to cite this article: Sadeghi E, Sadeghi S. Study of the Relations Among Tumor Size and Axillary Lymph Nodes Involvement With the Prognosis of Patients With Breast Cancer Surgery in Shohada Hospital in Tehran, Tajrish. Biomed Pharmacol J 2015;8(1) |
| Copy the following to cite this URL: Sadeghi E, Sadeghi S. Study of the Relations Among Tumor Size and Axillary Lymph Nodes Involvement With the Prognosis of Patients With Breast Cancer Surgery in Shohada Hospital in Tehran, Tajrish. Biomed Pharmacol J 2015;8(1). Available from: http://biomedpharmajournal.org/?p=977 |
Introduction and articulating the importance of the issue
Breast cancer is the most common type of cancer among Iranian women, which in 70 percent of cases are discovered when the disease has reached an advanced stage and that in 50% of cases when detected that the size is of 5 cm past. 5-year survival rate of the disease in Iran is about 62 percent that is little more than other countries (1, 2). Patients with this disease because of the physical and psychological effects – grapple a reduced quality of life experience. Thus, on one hand, timely detection and prevention of breast cancer cases on the other hand are factors that can significantly reduce the burden of disease. Today, several risk factors have been identified in this area some more and some less raise the risk of (3-5). Researchers could report around the world in epidemiological studies of breast cancer risk factors that are important in terms of clinical diagnosis. Berek considers the most important risk factors for breast cancer including: Age, family history of breast cancer, high-fat diet, obesity, reproductive and hormonal factors such as early menarche, late menopause, infertility, benign breast disease, high levels of estrogen in hormone replacement therapy at menopause and uterine cancer, ovarian and colon. The risk of breast cancer is 6 times higher after pre-menopause. Early menstruation and late menopause raises the risk of breast cancer because breast for many years are more exposed to estrogen and progesterone. Among other risk factors of breast cancer, it can be mentioned such as tumor size and lymph node involvement.
Objectives of the study
The major aim of this study to identify the correlation between tumor size and axillary lymph node involvement with the prognosis of patients with breast cancer as well as to provide appropriate procedures abnormalities underlying breast cancer and prevent its progress.
Research questions
- Is there a significant relationship bbetween the involvement of lymph nodes and prognosis of patients with breast cancer?
- Has the tumor size any effect on the prognosis of breast cancer?
- Is the number of lymph nodes involved and the size of the tumor effective to prognosis in patients with breast cancer?
Literature review
Breast cancer
Breast cancer is an important epidemiological issue with a global expansion. The prevalence rate in Asian women is higher compared to America and Western Europe. The women living in industrialized countries, of course, have a higher risk in comparison with others, Japan is an exception to this. Diagnosis of Breast Cancer is one of the most unpleasant events may occur during a woman’s life. But the patient should try to overcome the disease, rather than allowing the disease to dominate. The fear of breast cancer is a normal and pandemic response perhaps part of it due to increase public awareness about the disease. While the patients, except for the physical dimension, are grappling with the psychological effects of breast cancer as well and overall quality of life has dropped (7).
Causes of breast cancer
In the disease, malignant proliferation of epithelial cells or breast lobules has occurred. Like all epithelial malignancies, the incidence of breast cancer increase with rising the age gradually, but by the outage of menstruation, the slope of the curve decreases. Age at menarche, menopause and first pregnancy are the important affecting dates on the occurrence of breast cancer in women. The lower age at menarche, older first pregnancy and menopause age increases the risk of the disease that these markers show the cancer is a sex hormone dependent. Women age at menarche was 16 years old, about 50-60% of people who are at the age of 12 years old are diagnosed with breast cancer. Similarly, risk of earlier amenorrhea in women over the age of 10 years than the average age of its natural age (52 years old) that in others is 35% or by surgical removal of the ovaries in women early menstruation is a risk of breast cancer, a third of those found in their natural menopause, occurs at the age of 50 years or more. Also, people who have experienced their first pregnancy under the age of 20, compared to nulliparous women, have 30-4 0% lower risk of breast cancer. The reason for this is continuous exposure to internal progesterone in the absence of sufficient estrogen. Thus, during the period of menstruation, and particularly that part of the course before the first pregnancy is one of the risk factors of breast cancer. This factor can be 70-80% responsible for the differences in the incidence of breast cancer among different nationalities. For example, in Iran, breast cancer patients have different patterns compared to the patients in western countries. The mean age of the patients has been reported in our country less than others. According to numerous studies, the family history of breast cancer and marital status of individuals, are two important and effective factors in Iranian patients. More young patients’ contribution can largely be explained because of the young population of our country. The first two factors, mansturation periods in older age and lower gestational age, are important protective factors against breast cancer in older ages. Thus, the presence of these two factors, the incidence of cancer is a trend toward a younger age. In the meantime, especially since the first full-term pregnancy, is the most important protective factor. Based on the research results, the risk of breast cancer at an early age than non-pregnant women reduced, and conversely, increasing the risk later in older life. Geographical differences in the incidence and mortality from breast cancer have shown that risk factors for the disease varies in different areas for breast cancer, mainly in relation to environmental factors are stronger than genetic factors (7, 8).
Other factors contributing to breast cancer can be mentioned as follows:
Genetics
a third of all people, has a history with breast cancer in one or more first- or their second- degree relatives. In people who have had a mother or sister with breast cancer, the risk is more than 4 times. But this does not mean that in the event of infection or relative of first degree with the disease, a person certainly will be affected. Breast cancer is the result of genes involved in the disease and genetic factors is observed usually at an early age (under 40 years), the number of patients and relatives in one or both breasts (though not simultaneously). Histological characteristics of identified genes can determine the severity of tumor invasion (6, 8).
Diet
foods high in fat and fried foods has doubled the risk of breast cancer. Quality and low quantity of fat in the diet, both contribute to this disease. The average alcohol consumption and the incidence of the disease has been related to its mechanism that is still unknown (8).
Hormone therapy
it is of great importance to determine the potential role of hormones in the development of breast cancer, for millions of women are regularly taking oral contraceptives or receiving hormone replacement therapy during menopause. It is believed that even long-term use of OCP, does not increase the incidence of breast cancer. But studies also favor that long-term use of combination pills can be effective in cancer in people who are very young and /or they do not experience the pregnancy. But it is suggested that the role of these factors in breast cancer even if being positive, will be very small. (In contrast, oral contraceptives have a protective role against epithelial ovarian tumors endometrial cancer). The World Health Organization survey shows that the use of an injectable contraceptives (DMPA) does not increase the risk of breast cancer (8).
Yet, it’s not clear that hormone replacement therapy (HRT), if there is a family history of breast cancer or positive findings of previous biopsies, breast cancer risk is changing or not. Some researchers believe that estrogen after menopause at an early age is associated with taking hormonal deficiencies, with a slight increase in breast cancer risk. Especially if there is a history of benign breast disease. But if he/she takes estrogen plus progestin, there is not enough information about the size of the impact. In total, the average benefit of HRT proposed for women (8).
Obesity
According to the most current information, overweight is associated with breast cancer. Risk in obese women is 1/5-2 versus others that the risk associated with the menopause (8).
History of early breast cancer
in women with a previous positive history of breast cancer, the risk of breast side is more than 3-4 times. Although ovarian cancer or a previous history of uterine, breast cancer increase about 1/3- 1/4 times more (8).
Radiation
in young women who have been exposed to radiation to the chest, higher risk have been reported for developing the disease. But at the age higher than 30 years, there is a lowest rate. The risk from several low-dose radiation, is the same with high-dose irradiation. Less than 1% of the Breast Cancer arises in radiological diagnostic procedures. It is possible that radiation treatment for breast cancer also increases the risk of the other party involved. Following radiation treatment for cervical cancer, the risk of breast cancer is reduced.
The reason for this is to reduce the amount of estrogen (7, 8).
Diagnostic Tests and examinations
Breast exam is an important part of the physical examination. Usually for these examinations, the patient is referred to gynecologist. While women should be trained and act for BSE. Although Breast Cancer in men is rare, but if there is any unilateral lesion should be examined as well as women.
Usually two categories of diagnostic tests for breast cancer are:
- Special screening test are asymptomatic for signs of disease in women.
- The use of diagnostic tests in which the disease is diagnosed or suspected.
Breast self-examination should perform monthly by women. At least the benefit of this action is to identify small tumors that can be treated by brief surgery interventions. More than 65% of breast lumps are discovered by the patients themselves. There are some special features in keeping with palpable breast lesions and masses (such as breast enlargement, skin changes, nipple discharge, nipple changes, strain or breast asymmetry, redness, firm sores, irregular mass fixed armpit) raise suspicion of malignancy. Pain, reduces the risk of malignant breast masses.
A physical examination alone cannot rule out malignancy. In pre-menopausal, suspicious lesions should be checked again within 2-4 weeks. 5 to 7 days of the menstrual cycle is the best time to do breast examination. Significant mass in women after menopause and stable mass during a menstrual cycle before menopause, should be further examination and needle biopsy (8).
Fine needle aspiration and biopsy should be performed only in centers that have skills in this method of sampling and reports the correct result. Sonography can be replaced a needle biopsy to differentiate solid from cystic masses. Breast cysts are very common and are rarely cancerous. Some women experience periodically cystic masses before the start of menstrual cycle that is safe. Using ultrasound is most convenient method to determine the problem. A sample of the fluid in the cyst with a needle drawn is sent to a pathological study. Hyperplasia observed under the microscope, is only a benign growth of breast cells. But if hyperplasia of atypical (unusual), the cancer is associated with an increased risk of conversion. Solid mass, and permanent or recurrent cysts containing blood must be evaluated by mammography and biopsy. Both the patient and the physician should be aware of the possibility of a percent false negatives of these results.
Mammography is an alternative for cases where there is clinical suspicion. Hidden cancers can be discovered before 5 mm with the help of mammography. According to current guidelines America Cancer Society, it is better to start the breast self-examination in women from the age of 20, at age 35, a mammogram as a primary criterion and from ages 40 to 50 years old also is performed mammograms on an annual basis. Screening by mammography in the detection of cancer in its early stages, decreases the mortality results. All abnormalities seen on mammography should be examined carefully. If non-palpable breast lesions look a little suspicious, it is wise to redo mammogram within 3-6 months. When a malignant lesion corresponded with the criteria, open biopsy should be done by special techniques. If the examination palpable lesions exist, the biopsy method depends on the physical properties of the tumor, its location and size, the willingness of patients and anesthesia treatment, and the program selected.
After the diagnosis, treatment and predicting longevity and survival of the patient, or staging must be done. Number of lymph nodes involved is the most important criterion for prediction of survival and relapse. In the absence of lymph node involvement, treatment failure rate over 10 years is about 20% that with 4 lymph node involvement is 71%. For the possibility of late metastasis, abdominal CT scan or MRI tests such as bone scans and radionuclide are used. After a preliminary evaluation, according to the characteristics of the tumor (T), lymph node involvement (N) and presence or absence of metastases (M) that TNM classification, the stage of the disease is determined. With late metastasis, regardless of other characteristics, cancer is put on stage 4 (IV).
Research shows that 60% of patients who have metastatic disease, will die within 2 years after surgery. Patients survive for 5 years after the onset of symptoms does not necessarily mean treatment complete eradication of the disease. According to the opinion of the National Cancer Institute, the possibility of 5 years survival for non-metastatic breast cancer is 80%. Tumor recurrence risk over time will decrease more and more. But it has been observed that sometimes even 20-30 years, metastatic foci appear after treatment of primary tumor. Because after a few initial division of malignant cells, there is a possibility of metastasis at any time. The most common sites of involvement include bone, lung, pleura, soft tissues and the liver (7 and 8).
Today, a list of different treatments is available, depending on the particular circumstances of each individual. Factors such as tumor stage and specific characteristics affect the selection. Surgery may be performed along with breast conservation. Sometimes the whole breastis removed with lymph glands. Sometimes, depending on the tumor, chemotherapy or hormone therapy will be required.
Several clinical trials have shown that breast conservation surgery that is limited only to remove the tumor, the survival rate of patients with extensive methods is equal to mastectomy. Both groups of patients have shown almost the same survival for 10 years, but keep the breast has been more involved with risk of recurrence. Breast conservation surgery for all patients is not an appropriate method. For example, tumors larger than 5 cm, with extensive intraluminal tumors that for the most part are invasive tumors involving the nipple and the adjacent, those who do not want to keep the breast or do not have access to radiotherapy after surgery, are all the items unsuitable for breast conservation methods however, include about one-third of patients. Usually, for large tumors (over 3 cm) associated with axillary metastasis, chemotherapy is used before surgery after mastectomy Radiation therapy. Radiation therapy can reduce the rate of local or regional recurrence, and it should be considered the primary tumor in women who have high-risk conditions (6-8).
Screening and its various ways
Breast cancer is a serious disease that is fatal that will kill people in the absence of proper treatment. Australian women die of breast cancer more than any cancer, and one out of every nine Canadian women during life experiences breast cancer. In Scottland, breast cancer is the second most common cause of death in women. A study, in 1996 in University of Medical Sciences of Shiraz has reported the prevalence of 100.000 females over 35 years as 670 and a research in 1998, in University of Medical Sciences of Bushehr, the prevalence of 798 in hundred thousand women with 30-65 years old was reported. According to investigations the death in four Iranian provinces in 1999, breast cancer has the sixth proriority among cancer deaths in women in 2000 and the eighth priority in the ten provinces of the country in 2001. Screening methods are described in reference books in different countries run current programs include:
- S.E) Breast Self Exam
- Clinical Breast Exam
In the context of National Breast Screening Study (NBSS2) of Canada showed in the two study groups that a CBE method and other methods were used for screening mammography and CBE, adding mammography is not effective in reducing mortality. In different researches, CBE sensitivity has been reported between 24-63% and specificity of 95to 96/5% (7, 8).
Mammography
Screening with mammography results in a 30% decrease of deaths approximately from breast cancer in women with 50 to 69 years old. The figure for women 40-50 years old is about 17 percent. In appropriate circumstances, the sensitivity of this test depends on several factors including the patient’s age, tumor size and density of breast tissue, hormones, and overall quality and image the radiologist’s skills. The rate of false negative mammogram is more in young people than the elderly. False-negative rate of 25% for women 40-50 years old for women over 50 years is 10%. For several pre-screening with mammography was recommended only for women 50-65 years old but in a recent article and some reference books, this method has been recommended for women over 40 years. According to the study of Breast Center of Iran and surgens’s idea, Cancer Institute, the age of incidence of breast cancer in Iran is lower than western countries. Also, axamining the available resources showed no activity on mammography devices in the method for screening mammography (7, 8).
So on the whole it can be said that:
- BSE testing as a screening test in the world is not perfect (because it lacks sufficient sensitivity)
- CBE even has more sensitive test, but how to do it is very effective in results. If an experienced person have substantial positive results and will not otherwise be a valid test. The validity of this test is to standardize the training and depends on skills of people.
Mammography testing has lower sensitivity for younger than 50 years but for people more than 50 years is known as the most prestigious and most sensitive test. All systems provide breast cancer screening services in the world, mammography is considered as a key test, and according to the situation, CBE is added (7, 8).
Research Methodology:
This study is a descriptive-analytical one.
Statistical population
The population consisted of all patients with breast cancer that have surgery in the last 10 years at Shohada hospital in Tehran. Thus, data collection was carried out through the whole number (100 patients).
Tools and methods for data collection
demographic and disease records extracted from the medical records and analyzed using SPSS statistical software.
Data analysis
After collecting the required information from all subjects, we have to analyze the data in this field, so we use SPSS software (version 13). Chi-square tests used in this test and Independent-Sample T and the level of significance for the interpretation of the relationship between variables were considered 0/05.
Analysis
In this section, we first assessed demographic information obtained from the patients using SPSS software and analyzed the tests listed.
Describe the data and information:
- The average age of the subjects was 57/94. The mean tumor size was 45 mm.
Chart frequency of tumor size in the studied patients
 |
Figure 1 |
- The average number of lymph nodes involved was 2/64.
 |
Figure 2 |
- 21 percent were positive based on hormone receptors.
- 84 percent had poor prognosis.
 |
Table 1 |
- 90 percent had lymph node involvement.
- 44 percent had a positive family history.
Discussion and review of the data:
In this section the results of tests carried out on information and statistics are provided
- age, number of lymph nodes involved and the prognosis for patients with tumor size was not observed (P> 0.05).
- 86/7 percent of those who had lymph node involvement and 60 percent of those who had lymph node involvement, had a poor prognosis that showed a statistically significant difference (P = 0.029).
- 75% of those with a positive family history and 91/1 percent of those who had a positive family history, had a poor prognosis showed a statistically significant difference (P = 0.030).
- 98/7 percent of those who had no hormone receptors and 28.6 percent of those who had hormone receptors, had a poor prognosis that showed a statistically significant difference (P = 0.0001).
- Prognosis of patients was not related with tumor size observed (P> 0.05).
- The age of the patients studied were not associated with prognosis (P> 0.05).
- The number of lymph nodes examined, were not in connection with the prognosis of patients (P> 0.05).
- 86/7 percent of those who had lymph node involvement and 60 percent of those who had not lymph node involvement, had a poor prognosis that showed a statistically significant difference (P = 0.029).
- 75% of those with a positive family history and 91/1 percent of those who had a positive family history, had a poor prognosis that showed a statistically significant difference (P = 0.030).
- 98/7 percent of those who had not hormone receptors and 28.6 percent of those who had hormone receptors, had a poor prognosis that showed a statistically significant difference (P = 0.0001).
 |
Table 2 |
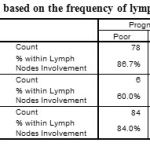 |
Table 3 |
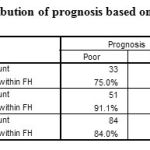 |
Table 4 |
 |
Figure 3 |
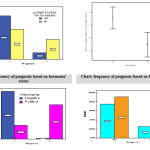 |
Figure 4 |
Summary and conclusions
The incidence of breast cancer is rising in many countries, although in some cases the death rate may be stable or declining slightly. Due to geographical differences, the rate in North America, Northern Europe and the Pacific is high and in South America, the average rate of prevalence is low compared to Africa and Asia. Most studies show that less than 5% genetic factors are inherited. Although some have mentioned to 10%.
Risk factors for breast cancer in reproductive problems of women, including: early menstruation, infertility, high age at first childbirth, late menopause, diet and physical activity and endogenous hormonal factors (high levels of free estrogen to estrogen binds to serum proteins) or exogenous (long-term use of birth control pills or hormone replacement therapy in postmenopausal women). In Iran Like many developing countries, breast cancer is the most common cancer and is considered as a very important health issue to women, and based on the incidence is on the second level after the blood and lymphatic system cancers. Accordingly, in this study, the correlation between tumor size and axillary lymph nodes involved with the prognosis for patients with breast cancer surgery were studied at Shohada hospital in Tajrish, Tehran over the last 10 years.
In this research, the mean age of the patients was 57/94 years. The mean tumor size was 45 mm, and the mean number of lymph nodes involved was 2/64. 21% of patients were positive due to hormone receptor. 84 percent had poor prognosis. 90% had lymph node involvement. 44% had a positive family history. Age, number of lymph nodes involved and the prognosis was observed for patients with tumor size (P> 0.05). 86/7 percent of those who had lymph node involvement and 60 percent of those who had not lymph node involvement, had a poor prognosis that showed a statistically significant difference (P = 0.029). 75% of those who had a positive family history and 91/1 percent of those who had not a positive family history, had a poor prognosis that showed a statistically significant difference (P = 0.030). 98/7 percent of those who had not hormone receptor and 28.6 percent of those who had hormone receptor, had a poor prognosis that showed a statistically significant difference (P = 0.0001).
- In a study that was performed in Italy and its results were published in 2007, it was announced that lymph node involvement was significantly associated with prognosis in patients with breast cancer that is consistent with the findings in this study.
- In a study that was done in America, and the results were published in 2008, it was announced that the higher number of lymph nodes involved trigger prognosis that is similar to the findings in this study.
- In a study that was done in America and its results were published in 2002, it was announced that the size of the tumor in cases where size is less than a centimeter has no impact on the prognosis of breast cancer in this study that is consistent with the findings .
- In a study conducted in Canada and the results were published in 2009, it was reported that a family history of breast cancer in first-degree relatives is an independent risk factor for poor prognosis in patients with breast cancer that is similar to the findings of this research.
In sum, based on the results of this study, compared with other studies in this area, it is suggested that the involvement of lymph nodes causes the unfavorable prognosis on breast cancer in patients, but the number of lymph nodes involved and the size of the tumor did not have an impact in the field.
References
- Harirchi I, Ebrahimi M, Zamani N, Jarvandi S, Montazeri A. Breast cancer in Iran: a review of 903 case records. Public Health. 2000 Mar;114(2):143-5.
- Vahdaninia M, Montazeri A. Breast cancer in Iran: a survival analysis. Asian Pac J Cancer Prev. 2004 Apr-Jun;5(2):223-5.
- Radice D, Redaelli A. Breast cancer management: quality-of-life and cost considerations. 2003;21(6):383-96.
- Ebrahimi M, Vahdaninia M, Montazeri A. Risk factors for breast cancer in Iran: a case-control study. Breast Cancer Res. 2002;4(5):R10.
- Singletary SE. Rating the risk factors for breast cancer. Ann Surg. 2003 Apr;237(4):474-82.
- Laster SC. The Breast. In: Robbins Stanley L, et al. Basic Pathology. 8th W.B. Saunders. 2007
- Danforth DN, et al. Danforth Obstetrics and Gynecology. 10th 2008.
- Schwartz S, et al. Schwartz Text book of Surgery. McGraw-Hill Publication. 2005.







