Manuscript accepted on :
Published online on: 18-12-2015
Plagiarism Check: Yes
Mohammad Ali Ghavimi1*, Koroushtaheritalesh1, Arezou Ghoreishizadeh2, Masoomeamani3 and Aylardivband4
1Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran.
2Department of Pediatric Dentistry, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran.
3Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran.
4Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, East Azerbaijan, Iran.
DOI : https://dx.doi.org/10.13005/bpj/410
Abstract
Preservation of bone volume after tooth loss is necessary for successful implant placement. The aim of the present study is to compare changes in bone height and pathological problems using autogenous bone with collagen material as well as surgicel alone. This is a clinical trial study in which 39 patients requiring implants in the posterior maxilla were selected. Patients were randomly divided into control and treatment groups. In the control group, autogenous tuberosity bone was used to increase alveolar height after sinus shift. In the case of sinus membrane rupture, a resorbable collagen membrane along with autogenous bone was used. In treatment group, surgicel was used alone to shift sinus membrane. T-test was used for statistical comparison. In control group, pathological abnormalities in the nasal passages were more than the treatment group. Statistical analysis revealed a significant difference between the mean bone height after surgery in the control (10.4±2.6) and treatment groups (12.5±2.7) (p=0.02). According to the results of present study, the use of surgicel has a greater effect on bone growth compared with autogenous bone and collagen membrane.
Keywords
Maxillary Sinus; Surgicel; Autogenous Bone; Membrane
Download this article as:| Copy the following to cite this article: Ghavimi M. A, Koroushtaheritalesh, Ghoreishizadeh A, Masoomeamani, Aylardivband. Autogenous Bone with Collagen Material and Surgicel for Maxillary Sinus Membrane Elevation (Sinus Lift) in Human Subjects. Biomed Pharmacol J 2013;6(2) |
| Copy the following to cite this URL: Ghavimi M. A, Koroushtaheritalesh, Ghoreishizadeh A, Masoomeamani, Aylardivband. Autogenous Bone with Collagen Material and Surgicel for Maxillary Sinus Membrane Elevation (Sinus Lift) in Human Subjects. Biomed Pharmacol J 2013;6(2). Available from: http://biomedpharmajournal.org/?p=2707 |
Introduction
Maxillary sinus development is normally stopped after the eruption of permanent teeth. With loss of teeth, sinuses floor gradually spread to the roof of mouth and become close to it, so that over time only a thin bone layer will separate the oral cavity from the nasal passages (sinus). Sinus lift involves lifting the lower Schneiderian membrane covering inner surface of maxillary sinus and filling the gap between the membrane and the inner surface of sinuses with autogenous bone or biomaterial. Alveolar bone resorption occurs following teeth loss. If the time between tooth loss and attempt to place an implant is long, maxillary sinus pneumatization into edentulous alveolar remains will often occur. In this case, to insert a dental implant with an appropriate length, the maxillary sinus floor should be reinforced by elevating the sinus floor [1]. To reduce bone resorption after tooth extraction, it is recommended to use synthetic bone graft materials and autologous graft materials of patient [2].
So far, numerous graft materials have been used for sinus augmentation including autogenous bone, alloplast, allograft, xenograft and surgicel, alone or in combination with autogenous bone [3-6]. However, there is still uncertainty in choosing the best method [7]. Therefore, the present study used autogenous bone with collagen material in patients who required sinus lift. The results were compared with surgicel performance.
Materials and Methods
The sample consisted of 39 patients including 16 males and 23 females with an age range of 41-68 years who admitted author’s private clinic for insertion of implants in posterior maxilla. The inclusion criteria included: the need for implants in posterior maxilla, a residual bone height of at least 6 mm so that the implant placement along with sinus membrane elevation is not possible and having a normal sinus with no morphological and pathological abnormalities. Exclusion criteria included sinus pathology and bone width less than 5 mm where implant placement with sinus membrane elevation is not possible.
Among 53 patients, 14 patients required bilateral maxillary sinus membrane elevation (sinus lift). These patients were excluded and finally 39 patients were enrolled. Following sample selection, the patients were given a full explanation and a written consent was taken.
Patients were divided into two groups. The control group consisted of 23 patients. In this group, resorbable collagen membrane (Implantium, South Korea) with autogenous bone was used in the case of sinus mucosa rupture. In all cases, membrane elevation was carried out as follows: after local anesthesia with lidocaine and epinephrine 1/80000, crestal incision was made on the alveolar ridge. Mucoperiosteal flap with anterior release was given. Then, bone window was removed slowly by round milling without maxillary sinus membrane rupture. Maxillary sinus membrane was driven slowly upward. In 23 cases, autogenous bone tuberosity was used to increase alveolar height and sinus elevation. Before placing autogenous bone, membrane was carefully examined and resorbable collagen membrane along with autogenous bone was used in the case of sinus membrane rupture.
In treatment group which consisted of 30 cases, after a crestal incision and osteotomy of lateral wall of the maxillary sinus, surgicel was used alone for sinus lift. Collagen membrane was not used in the case of sinus membrane rupture and only surgicel (hemostatic agents made of oxidized cellulosic polymer which is made in Turkey- Skyteks) was used. In both groups, “Cone Beam CT” was prepared after 6 months to assess bone height and sinus pathology. The mean and standard deviation of bone height was calculated. Paired t-test was used for statistical analysis. A significance level of p<0.05 was considered. Prism software was used for statistical analysis.
Results
Bone height was measured 6 months after surgery to evaluate and compare the effects of surgicel, autogenous bone and membrane. Moreover, all patients were examined for sinus pathology including mucosal thickening or postoperative fluid. Bone height in control group was 4.13±0.97 which showed no statistical significant difference with treatment group (3.8±0.98). Statistical analysis showed a significant difference between bone heights before and after surgery in the control group (p<0.0001) (Fig. 1).
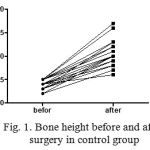 |
Figure 1: Bone height before and after surgery in control group
|
Furthermore, paired T-test showed a significant difference between bone heights before and after surgery in treatment group (p<0.0001) (Fig. 2).
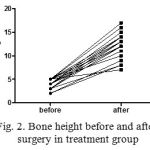 |
Figure 2: Bone height before and after surgery in treatment group
|
The mean postoperative bone height in control group was 10.4 ± 2.6 mm. The statistical analysis showed a significant difference between control and treatment group with mean bone height of 12.5±2.7 mm (p=0.02). Of 23 cases in the control group, sinus pathology (2 cases with sinus pathology and 3 cases with sinus thickening) was observed in 5 patients. Of 30 cases in treatment group, only one case with sinus thickening was observed and other patients showed no pathological problems.
Discussion
In this study, the autogenous bone along with collagen material was used for patients who underwent maxillary sinus membrane elevation surgery and the results were compared with surgicel application. Bone height measurements and pathological studies were carried out 6 months after the surgery. However, other studies have chosen different times, for example Senel et al. selected 3 months to examine bone growth [8], or Gray et al. examined bone size after 10 weeks. It seems that 6 months is an appropriate duration in terms of bone growth or pathological changes [9].
In the control groups, postoperative sinus fluid was observed in two patients. No postoperative fluid was found in treatment group. Moreover, mucosal thickening was found in 13% of cases in the control group. The frequency of mucosal thickening in treatment group was 3%. Fewer cases of mucosal thickening were observed in the treatment group in terms of pathology factor. This may confirm better performance of surgicel compared with autogenous bone and collagen as a graft material. These results are consistent with the results of Simunek et al. who found the use of surgicel led to very little microbial contamination of the surgical site. They suggested that the surgicel has no contraindication in maxillary membrane [10].
A significant difference was found between bone height before and after surgery in both groups. This indicates that both methods led to satisfactory results in terms of bone height. Consequently, graft materials have a stimulatory effect on new bone formation. The results of the present study are consistent with previous studies. For example, Adeyemo et al. and Zubery and colleagues found that the use of collagen graft material reduces the rate of bone resorption [11, 12]. Senel and colleagues also demonstrated that after 3 months, vertical bone growth was significant [8].
But given that the bone height prior to surgery was not significantly different, detailed analysis should be performed after surgery to calculate difference between the teeth height in both groups. The results showed a significant difference between two groups such that bone growth was higher in the treatment group. Gray and colleagues also demonstrated that surgicel is an appropriate graft material for bone growth in sinus lift [3]. Smiler et al. suggested similar conclusions on the effectiveness of surgicel in sinus lift [13]. Given the results of the present study and also due to the cheap, fast and safeness, surgicel is recommended as a graft material in maxillary sinus elevation surgeries.
Acknowledgments
We would like to appreciate Tabriz University of Medical Sciences Research Vice-Chancellor.
References
- Shillingburg, H.T., et al., Fundamentals of fixed prosthodontics. Vol. 194. 1997: Wiley Online Library.
- 2. Fonseca, R.J., Oral and maxillofacial surgery: Orthognathic surgery. Vol. 2. Vol. 2. 2000: Elsevier Health Sciences.
- Gray, C.F., et al., Magnetic resonance imaging assessment of a sinus lift operation using reoxidised cellulose (SurgicelR) as graft material. Clinical oral implants research, 2001. 12(5): p. 526-530.
- Rickert, D., et al., Maxillary sinus lift with solely autogenous bone compared to a combination of autogenous bone and growth factors or (solely) bone substitutes. A systematic review. International journal of oral and maxillofacial surgery, 2012. 41(2): p. 160-167.
- 5. BOYNE, P.J., Grafting of maxillary sinus floor with autogenous marrow and bone. Oral Surg., 1980. 38: p. 613-616.
- 6. Tidwell, J.K., et al., Composite grafting of the maxillary sinus for placement of endosteal implants. A preliminary report of 48 patients. International journal of oral and maxillofacial surgery, 1 21(4): p. 204-209.
- Jensen, O.T., The sinus bone graft. 1999: Quintessence Publishing Company Chicago.
- Cizmeci Senel, F., et al., Assessment of the sinus lift operation by magnetic resonance imaging. British Journal of Oral and Maxillofacial Surgery, 2006. 44(6): p. 511-514.
- 9. Gray, C., et al., Assessment of maxillary sinus volume for the sinus lift operation by three-dimensional magnetic resonance imaging. Dentomaxillofacial Radiology, 2000. 29(3): p. 154-158.
- Simunek, A., D. Kopecka, and M. Cierny, The use of oxidized regenerated cellulose (Surgicel®) in closing Schneiderian membrane tears during the sinus lift procedure. West Indian Medical Journal, 2005. 54(6): p. 398-399.
- Adeyemo, W., et al., Healing of onlay mandibular bone grafts covered with collagen membrane or bovine bone substitutes: a microscopical and immunohistochemical study in the sheep. International journal of oral and maxillofacial surgery, 2008. 37(7): p. 651-659.
- Zubery, Y., et al., Ossification of a novel cross–linked porcine collagen barrier in guided bone regeneration in dogs. Journal of periodontology, 2007. 78(1): p. 112-121.
- Smiler, D.G., et al., Sinus lift grafts and endosseous implants. Treatment of the atrophic posterior maxilla. Dental Clinics of North America, 1992. 36(1): p. 151-86; discussion 187-8.







