Manuscript accepted on :26-Oct-2018
Published online on: 05-11-2018
Plagiarism Check: Yes
Reviewed by: Akshat Pandey
Second Review by: Joshua Zadro
Final Approval by: Mohamed Abdel-Daim
Department of Neurosurgery, Udayana University / Sanglah Hospital, Bali, Indonesia.
Corresponding Author E-mail: tjokmahadewa@unud.ac.id
DOI : https://dx.doi.org/10.13005/bpj/1586
Abstract
Brachial plexus injury is an injury of the shoulder nerve that often happens in young adult. It has a relatively high disability rate. The clinical outcomes of brachial plexus surgery to date are still disappointing, especially for the total plexus injury that affects the C5-T1. However, expectations remain with the advance of technology and more recent surgery techniques, specifically the emergence of distal neural transfer. This was a retrospective study with 9 brachial plexus injury patients, since 2012-2017. The aim to evaluate surgical strategies outcome of the management. The principle of handling brachial plexus palsy when conservatives fail is surgery, like autologous graft, neural transfer, neurolysis, and direct suture. Improvement of elbow flexion is the utmost priority and shoulder stabilization as well. Various techniques are used lately, but to date, they have not been able to improve the functioning of the patient's fingers.
Keywords
Neural Transfer; Outcome; Shoulder Nerve; Surgical Management
Download this article as:| Copy the following to cite this article: Tjokorda M. Surgical Management of Brachial Plexus Injury. Biomed Pharmacol J 2018;11(4). |
| Copy the following to cite this URL: Tjokorda M. Surgical Management of Brachial Plexus Injury. Biomed Pharmacol J 2018;11(4). Available from: http://biomedpharmajournal.org/?p=23869 |
Introduction
Traumatic brachial nerve injury is a peripheral nerve injury that often occurs in the arms of young adult patients and results in severe disability. The surgical results in this case are generally unsatisfactory which leads surgeons to tend to be choosing conservative treatment or limb amputations in order for the patient to be free of severe neuropathic pain.1 This surgical reconstruction was popularized in 1970 by Millesi and Narakas. Currently, the technology is advanced in the form of a surgical microscope, intraoperative monitoring, special suture thread, biological glue products, and others. The outcome of the surgery began to show a glimmer of hope.2
The author’s aim is to refresh information on surgery strategies on the brachial plexus and its outcome. In this study, the author reports 9 brachial nerve injury patients with minimal 6 months time of follow-up.
Methods
The study was retrospective based on 9 brachial plexus injury patients, at Sanglah Hospital in Bali, from 2012–2017. This study was approved by the Committee of Research Ethics of Udayana University/Sanglah Hospital.
Electromyography evaluation was performed in all patients to evaluate the type of brachial plexus injury. The subject characteristics, length of stay, side effect, types of brachial plexus injury, donor site, target site, approaches, graft source, improvement, and other underwent procedures were recorded. The side effects were observed for vascular injury, pleural injury, neurological compromised, and surgical site infection.
Shoulder radiological examinations and EMG were taken in all patients. If there is a preganglionic injury, avulsion of the spinal nerve root, surgery for neural transfer is performed immediately (Figure 1). However, for postganglionic injury, it is advisable to observe for 3-4 months of the natural healing process.3 Patients have the best chance of recovery in the first 3 months of the injury. Surgical time is the most important factor in predicting the final results of operations.4
Patients are followed up clinically and physiotherapy is still recommended. The Manual Muscle Test (MMT) for evaluating muscle strength or as a grading system (0 for no muscle contraction; 1 for muscle tone power, 2 for being able to shift, 3 for being able to resist gravity, 4 for being able to resist moderate strength from the examiner and 5 for normal strength). Independent assessors evaluate the preoperative status and record improvements.
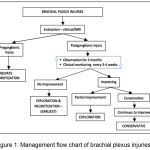 |
Figure 1: Management flow chart of brachial plexus injuries.3
|
Neurotization
Neurotization means functional donor nerve transfer to the more important distal recipient nerve. The concept was first introduced by Harry and Low in 1903, then in 1913 Tuttle introduced the use of spinal accessory nerve (SAN). The surgery indication is for preganglionic injury, or when the patient is referred late. The purpose of this operation is to restore more important nerve function, by placing the regeneration axons closer to the paralyzed motor nerves.3,5
Strategies for Total Plexus Injury (C5-T1)
A common injury is preganglionic root avulsion. In this case, a gradual approach using an extra brachial plexus donor is the only option. In the first stage, spinal accessory anastomosis to suprascapular nerve (SAN-SSN) is performed to improve abduction of the shoulder, this technique can be done by anterior or posterior approaches.
The next stage, elbow flexion improvement can be achieved by performing the 2nd to 4th intercostal nerve to musculocutaneous nerve (ICN-MCN) anastomosis and then is performing the 5th to 6th intercostal nerve to radial nerve (ICN-RN) anastomosis to improve elbow extension. (Figure 2).
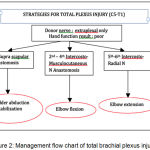 |
Figure 2: Management flow chart of total brachial plexus injury.3
|
Strategies for Partial Brachial Plexus Injury (C5-7)
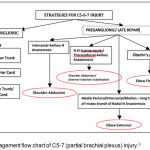 |
Figure 3: Management flow chart of C5-7 (partial brachial plexus) injury.3
|
For preganglionic injury, the most commonly used as a donor source is a medial pectoral nerve and intercostal nerves with promising reports.6 The donor nerve can be either intercostal, medial pectoral, thoracodorsal, phrenic, axillary, or ulnar nerves.
In the postganglionic injury, with a reasonable cervical root stump, brachial plexus may be repaired by these following options:
C5: for elbow flexion
C6: for abduction of the shoulder
C7: Middle trunk / posterior cord.
Results
Total plexus injury in 6 patients (C5-Th1) and 3 patients were diagnosed with partial plexus injury (C5-C7) (Table 1). In all total plexus injury patients, the author performed 2nd to 4th intercostal nerve to musculocutaneous nerve (ICN-MCN) anastomosis using sural nerve graft. One patient underwent additional spinal accessory nerve anastomosis to suprascapular nerve (SAN-SSN) via posterior approach and 1 patient had the 5th to 6th intercostal nerve to radial nerve (ICN-RN) anastomosis to improve elbow extension.
Table 1: Patients characteristic.
| Characteristic | Cases (n=9) |
| Sex | |
| Male, n(%) | 6 (66) |
| Female, n(%) | 3 (33) |
| Age, year old (y.o), mean
10-20 y.o, n (%) 21-30 y.o, n (%) 31-40 y.o, n (%) 41-50 y.o, n (%) Length of stay, days, mean Complications, n (%) |
32.7
1 (11) 4 (44) 1 (11) 3 (33) 7 0 (0) |
All three patients with partial plexus injury were compromising C5-7. All patients improved muscle strength of shoulder abduction and elbow flexion in 6 months after surgery, all patients using sural nerve as a donor (Table 2). There were no acute surgical complications after the follow-up period.
After surgery, the patients were checked for vital signs in the recovery room and then delivered to the room and the next day they received an exercise program prepared by the physiotherapist. Patients can be discharged when they can mobilize independently and all patients are scheduled for physiotherapy and follow-up for at least 6 months.
Table 2: Procedures and outcome.
| DX Preganglion |
Donor | Target | Sex/Age | Approach | Donor | MMT | Other procedure |
| TP | ICN | MCN | M/32 | Anterior | SN | 3 | – |
| TP | ICN | MCN | M/17 | Anterior | SN | 2 | – |
| PP | ICN | AXN | M/25 | Anterior | SN | 2 | – |
| TP | ICN | MCN | M/27 | Anterior | SN | 3 | – |
| PP | ICN | AXN | M/43 | Anterior | SN | 2 | – |
| TP | ICN | MCN | F/41 | Anterior | SN | 2 | – |
| PP | ICN | AXN | F/46 | Anterior | SN | 3 | SAN-SSN(posterior) |
| TP | ICN | MCN | M/26 | Anterior | SN | 2 | ICN-RN(posterior) |
| TP | ICN | MCN | F/24 | Anterior | SN | 3 | SAN-SSN(posterior) |
Dx = diagnose, MMT = manual muscle test, TP = total plexus injury, PP = Partial plexus injury, ICN = intercostal nerve, MCN = musculocutaneus nerve, AXN = axillary nerve, SN = sural nerve, SSN = suprascapular nerve, SAN = spinal accessory nerve, RN = radial nerve.
 |
Figure 4: Intraoperative views of SAN-SSN anastomosis via right posterior approach (black arrow).
|
Discussion
The operative handling time of a brachial plexus injury depends on the mechanism, type, and location of the injury. In a global avulsion injury of damaged preganglionic nerve roots C5-Th1, it requires immediate neurotization within the first 3 months. The main target of neurotization is trying to restore the abduction of the shoulder and elbow flexion. Immediate treatment of no more than 3-4 weeks is indicated for open injuries such as stab wounds, open fractures, gunshot wounds, accompanied by vascular injury, or severe deafferentiation pain. The immediate operative benefit is that the anatomy of the wound is still clear and can be immediately assigned to the rehabilitation program. Meanwhile, neuropraxia injuries are self-repair depend on time so that the need for the nerve surgery is minimal.7
Neurotization of nerves has several principles, like early neural transfer, reinnervation as close to the target organ, direct repair is better than the use of graft, intraplexal nerve transfer is better than ekstraplexal, the peripheral nerve transfers is better than medial, ipsilateral nerve transfer is better, and all nerve transfer patients need induction exercise.8
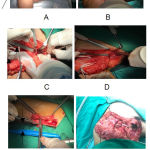 |
Figure 5(A-F): Intraoperative view performing the 2nd– 4th intercostal nerve to musculocutaneus nerve (ICN-MCN) anastomosis using sural nerve graft.
|
A. Skin Mark anterior approach; B. Identification musculocutaneous nerve; C-D. Identification intercostal nerve 3rd-4th right side; E.Sural nerve graft harvesting; F. Final ICN-MCN anastomosis.(black arrows).
There are no guidelines in the literature regarding the priority or urgency of the various functions that we must restore unless there are two indications. The priority in surgery for the brachial plexus is, the sequence is, (1) elbow flexion because it allows the hand to fold in a better position and can be bent toward the mouth to eat, followed by (2) shoulder stabilization, and supination. Then (3) elbow extension, (4) wrist movements and finger extension, and (5) finger movements. The function of the hand muscles is the last priority because the distance from the donor is further and the prognosis is worse for recovery. Sensory nerve repair is also a priority, if possible, and many surgeons seek to also conduct sensory transfers in the surgical plan to restore the sensation of the hand nerve (median nerve).9-10
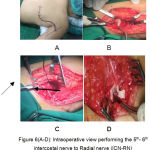 |
Figure 6(A-D): Intraoperative view performing the 5th-6th intercostal nerve to Radial nerve (ICN-RN) anastomosis using sural nerve graft.
|
A. Skin mark in a prone position; B. posterior intercostal 5-6th preparation; C. sural nerve graft connected to intercostal nerve 5-6th (right directed arrow); D. Sural nerve graft final anastomosis to the radial nerve (left directed arrow).
The results of neurotization depend on many factors, including distance to the donor nerve, presence or absence of graft, length of injury, rehabilitation program and others. This has an effect on healing or restoration of imperfect arm muscle strength. However, even the slightest change in arm muscle strength will be the patient’s dream compared to being completely paralyzed.
In the case of postganglionic injury, and the spinal nerve stump is still present, we prioritize C5 for elbow flexion and C6 for shoulder abduction.9-11 In the case of preganglionic injury, no spinal nerve stump is present, or in neglected patients, or elderly patients, for neurotization to achieve elbow flexion and shoulder abduction, we prepared SAN-SSN to achieve shoulder abduction and external rotation and long head of triceps nerve to anterior division of axillary nerve (Somsak’s procedure).12-14 Single suprascapular or axillary nerve neurotization can be performed for shoulder abduction, but in several reports on multiple nerve procedures, it is more effective in restoring shoulder abduction, external rotation, and stability.10,11
Conclusion
Nerve surgery in brachial plexus lesions has made great progress over the last few decades due to technological advances and reconstruction techniques, including distal neural transfer. Partial injury of the plexus has a good outcome in most cases, while the outcome of total lesions of the brachial plexus is not very satisfactory even today in Sanglah Hospital. Immediate handling and by a reliable team is an obligation and plays an important role in improving outcomes.
Acknowledgments
The author thanks Prof. Sri Maliawan, MD, Ph.D., who taught the author the first time to operate peripheral nerves in Sanglah Hospital.
Conflict of Interests
The author stated that there was no conflict of interest in the publication of this article.
References
- Seddon H. J. Nerve grafting. J Bone Joint Surg Br. 1963;45:447-61.
CrossRef - Robotti E., Longhi P., Verna G., Bocchiotti G. Brachial plexus surgery. An historical Hand Clin. 1995;11:517-33.
- Sumit S., Mehdi K., Nasim M., Rajiv M. Adult brachial plexus injuries: Surgical strategies and approaches. Neurology India. 2016;64(2):289-96.
CrossRef - Ferrante M. A. Electrodiagnostic assessment of the brachial plexus. Neurol Clin. 2012;30:551-80.
CrossRef - Kline D. G., Hudson A., Kim D. H. Atlas of Peripheral Nerve Surgery. Philadelphia: WB Saunders. 2001.
CrossRef - Flores L. P. Triceps brachii reinnervation in primary reconstruction of the adult brachial plexus: Experience in 25 cases. Acta Neurochir (Wien). 2011; 153:1999-2007.
CrossRef - Kline D. G. Timing for exploration of nerve lesions and evaluation of the neuroma-in-continuity. Clin Orthop Relat Res. 1982;163:42-9.
CrossRef - Samardzic M. M., Grujicic D. M., Rasulic L. G., Milicic B. R. The use of thoracodorsal nerve transfer in restoration of irreparable C5 and C6 spinal nerve lesions. Br J Plast Surg. 2005;58:541-6.
CrossRef - Toussaint C. P., Zager E. L. The double fascicular nerve transfer for restoration of elbow flexion. Neurosurgery. 2011;68:64-7.
- Leechavengvongs S., Witoonchart K., Uerpairojkit C., Thuvasethakul P., Ketmalasiri W. Nerve transfer to biceps muscle using a part of the ulnar nerve in brachial plexus injury (upper arm type): A report of 32 cases. J Hand Surg Am. 1998;23:711-6.
CrossRef - Estrella E. P., Favila A. S Jr. Nerve transfers for shoulder function for traumatic brachial plexus injuries. J Reconstr Microsurg. 2014;30:59-64.
- Ray W. Z., Murphy R. K., Santosa K., Johnson P. J., Mackinnon S. E. Medial pectoral nerve to axillary nerve neurotization following traumatic brachial plexus injuries: Indications and clinical outcomes. Hand (NY). 2012;7:59-65.
CrossRef - Lee J. Y., Kircher M. F., Spinner R. J., Bishop A. T., Shin A. Y. Factors affecting outcome of triceps motor branch transfer for isolated axillary nerve injury. J Hand Surg Am. 2012;37:2350-6.
CrossRef - Bertelli J. A., Santos M. A., Kechele P. R., Ghizoni M. F., Duarte H. Triceps motor nerve branches as a donor or receiver in nerve transfers. Neurosurgery. 2007;615(2):333-8.








