Humam M. Al-Somaiday, Mohammed Moudhaffer and Abdalbseet A Fatalla
Department of Prosthodontics, College of Dentistry, University of Baghdad, Iraq.
Corresponding Author E-mail: humammahmoud@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/1370
Abstract
Following the rapid development of denture base material and the invention of new materials that used to construct dentures, many studies aimed to test and compare the mechanical and physical properties of the newly developed materials as well as the effect of adding some additive to acrylic resin. As the denture placed in oral environment and subjected to many chemical materials and multiple forces, the denture base materials should have specific properties to full fill as much as possible the needed requirement to made dentures. Flexibility and high impact resistance considered as limitation in conventional heat cured acrylic resin; therefore, new techniques and materials have been introduced to overcome this limitation. In this study, impact strength, and transverse flexural strength and elastic modulus at maximum load of three dentures base materials (heat cured acrylic, polycarbonate and injectable acrylic) were compared. A total of (60) specimens of polycarbonate, injectable acrylic and conventional heat cured acrylic were fabricated according to manufacturer’s instructions and divided into (2) groups, (30) specimens for each testing group i.e. the impact strength and transverse flexural strength at maximum load except for the elastic modulus test at maximum load which was measured concurrently with transverse flexural strength (10 specimens for each testing material). Highly significant differences (P≤ 0.01) between all the (3) experimental materials were noticed after analyzing each test's results with descriptive statistical analysis, one-way ANOVA and post-hoc LSD. The Polycarbonate has the highest mean values of impact strength (233.43 KJ/M2) followed by the (injectable acrylic) with (29.89 KJ/M2) mean value while the lowest mean value was for the (heat cure acrylic) (7.53 KJ/M2). While the heat cured acrylic has the highest transverse flexural strength (77.03 MPa and elastic modulus (4.541 N/M2) at the maximum load, followed by Polycarbonate (69.12 MPa); (2.684 N/M2), then the injectable acrylic (60 MPa); (2.366 N/M2). Scanning electron microscope of fracture line after Charpy's impact test shows that both Polycarbonate and injectable acrylic had ductile fracture, while heat-cured acrylic exhibit brittle fracture. All injectable materials included in this study exhibit higher flexibility, elasticity, ductility and impact resistance. While heat cured acrylic exhibit higher rigidity, brittleness and low impact resistance.
Keywords
Denture Base; Polycarbonate; Thermoplastic Resins; Poly (Methyl Meth Acrylate)
Download this article as:| Copy the following to cite this article: Al-Somaiday H. M, Moudhaffer M, Fatalla A. A. Comparing the Impact Strength and Transverse Flexure Strength of Three Different Dentures Base Materials. Biomed Pharmacol J 2018;11(1). |
| Copy the following to cite this URL: Al-Somaiday H. M, Moudhaffer M, Fatalla A. A. Comparing the Impact Strength and Transverse Flexure Strength of Three Different Dentures Base Materials. Biomed Pharmacol J 2018;11(1). Available from: http://biomedpharmajournal.org/?p=19375 |
Introduction
Lost teeth compensation is one of the most substantial problems that dentists face, they need ideal material in order to provide effective dental services to patients. These materials should be biologically compatible, easily available, un expensive, and easy to manipulate with controlled technical procedures to develop an efficient prosthesis with satisfactory appearances.1 The denture should be aesthetically satisfactory or pleasing, function effectively, and be biocompatible with surrounding oral tissues that support it. A successful denture should be consistent dimensionally to enhance chewing efficiency, be comfortable for patients, and prevent oral tissues irritation.2 Many materials are used to fabricate dentures and each type of materials that used in denture base processing had an effect on denture base dimension during fabrication, and on other factors related to clinical use such as stability, support, retention, flexibility, impact resistance, and surface roughness etc… During the denture processing, the properties of the finished denture were mostly affected by the type of the material that used in denture manufacturing and other factors like polymerization shrinkage or stresses that resulted by cooling of flask, amount of the residual monomer and type of the processing technique.3
In 1937, Poly (methyl methacrylate) (PMMA) was introduced as denture base material.4 It is widely used material owning to its favorable properties. PMMA are produced synthetically, it can be packed and modeled, or injected into molds. also, it could be cured either by heat curing, chemically curing or light curing.5 Poly (methyl methacrylate) (PMMA) can be considered as the most widely used material in processing denture base regarding its many advantages, for example good aesthetics, acceptable fitness and stability in the oral environment, easy laboratory and clinical manipulation, and inexpensive equipment.6 On the other hand, poly (methyl methacrylate) has many limitations such as weak mechanical resistance (impact and flexural strength) which makes the dentures easily break down in clinical uses and repair them will impair denture strength over a short period of time thus, reduces the performance of the denture clinically.7,8
Additionally, the dimension of the denture made from PMMA may be altered and deformed throughout processing and/or during its uses.6 These dimensional alteration will lead to inadequate denture base adaptation to the oral tissue, reduction in denture stability, and incorrect positions of the artificial teeth.5 The concentration of residual monomer may consider as an additional factor that could have a drawback effect on the mechanical properties of the PMMA such as modulus of elasticity, surface hardness, impact strength, surface roughness and tensile strength, which founded to be the lowest mechanical properties of the PMMA with higher concentration of the residual monomer.8 Also, residual monomer may cause irritation and damage to the oral mucosa.10
Thermoplastic materials have been used to fabricate complete and partial dentures because of their many advantages such as the rarity of solubility in solvents, high strength, toughness, flexibility, ductility, abrasion resistance, high thermal resistance, and resistance to chemicals effects.11 The utilization of heat molding instead of chemical polymerization will provide dimensional stability and reduce the polymerization shrinkage and deformation of the resultant denture, in addition, making the denture biocompatible through monomer free nature.12
The poly (Bisphenol A) carbonate (also known as polycarbonate PC), is amorphous polymer with evidence of some areas of crystallinity.13 It is light in weight, transparent, and high-quality plastic. Also, it has outstanding mechanical properties, dimensional stability, excellent impact resistance,14 high plastic deformation without break or crack,15 high thermal resistance and it can retain its properties through a wide range of temperature change range from 140°C to –20°C. Under –20°C16 On the other hand, PC has some shortages in their properties, such as poor chemical resistance, limited scrapes resistance, and highly sensitive to UV rays which cause color changes. Proper additives or blending PC with other polymers can improve its limitation.14
Materials and Methods
This study investigated some mechanical properties of (3) different denture base materials: polycarbonate (A) (Extra Rigid M10 polymer. Deflex, Argentina), injectable acrylic (B) (ACRILITO Injectable acrylic. Deflex, Argentina) and conventional Heat cured acrylic (C) (MR.Dental, MEADWAY, England). A total of sixty bar shaped specimens were fabricated according to manufacturer’s instructions and divided into (2) groups, each containing thirty specimens according to the conducted tests i.e. the impact strength, and flexural strength (where n=10) except for the elastic modulus test which was measured concurrently with the flexural strength test. The dimensions of the impact strength test were (80 x10 x 4 mm)[17], while those for the transverse flexural strength test were (65 x 10 x 2.5 ± 0.1 mm).18
The laser cutting machine was used to prepare the acrylic bar pattern (Glass-look acrylic, Clairvaux les Lacsrance, France) after being designed by (Auto CAD 2015) computer software. The traditional complete dentures processing technique was followed during the mold preparation. The acrylic patterns were first coated with separating medium (Isodent Gypsum separating solution) and left to be dry. Dental stone (Kimberlit Extra Hard High Density Die Stone) mixed according to the manufacturer’s instructions and filled the lower part of the metal flask. Approximately one-half of the acrylic patterns were invested in dental stone in order to make a mark representing half of acrylic patterns depth after been measured by vernier (Fig. 1). After dental stone completely set, a second layer of the separating medium was applied and left to dry. The upper part of the flask was properly positioned and filled with stone. The same procedure was used in fabricating thermoplastic specimens (polycarbonate and injectable acrylic) with an additional step where wax tubes was attached to the acrylic pattern to allow the injection of the material(Fig.1); the wax elimination process done to remove the wax pattern by immersed the flask into hot bath 100oC for 10 min.18
Packing and curing of the heat cured specimens was performed according to ADA 1999 Specification No.12 in 1999),18 while the injection of the thermoplastic resins was done according to manufacturer’s instruction under (5-7 Bar) for (15 min) (for Polycarbonate, the injection temperature is (305oC ± 10oC) while the injectable acrylic temperature is (265oC ± 10oC) ) . Finally, each test specimens group was gathered and placed in plastic containers and filled with distalled water and were placed in incubator for 48 hours at 37oC ).18 The Charpy impact strength of unnotched specimen was calculated in KJ/m2 by the following equation).19
![]()
Where
E: is the impact absorbed energy in joules.
B: is the width in millimeters of the specimens.
D: is the thickness in millimeters of the specimens.
The transverse flexural strength was calculated using the following equation: ).19
![]()
Where
P: is the peak load (N)
l: is the span length(mm)
b: is the sample width (mm)
d: is the sample thickness(mm)
The elastic modulus (λ) was calculated in the elastic deformation region using the following equation: ).20
![]()
Results
SEM and FTIR tests
SEM results of Heat cured acrylic, polycarbonate and injectable acrylic are shown in (Fig 2) By examining the fracture line of the samples, we found that polycarbonate and injectable acrylic are ductile materials; while Heat cured acrylic is brittle material. 21
FTIR spectral results of two materials (Extra rigid polymer M10 and Acrylito ) were shown in (Fig.3 and 4) The results indicate that the major component of Extra rigid polymer M10 is polycarbonate and the major component of ACRILITO injectable acrylic is PMMA.
 |
Figure 1: molds fabrication. A: Heat cured molds; B: thermoplastic Materials molds
|
 |
Figure 2: 50 um magnification pictures were taken by SEM of the fracture line as following: A: heat cured acrylic; B: Injectable acrylic; C: Polycarbonate
|
 |
Figure 3: FTIR spectral results of Extra rigid polymer M10 showed that the major component is polycarbonate.
|
 |
Figure 4: FTIR spectral results of Acrylito showed that the major component of is PMMA
|
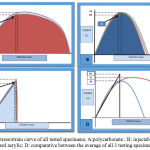 |
Figure 5: stress/strain curve of all tested specimens; A:polycarbonate ; B: injectable acrylic; C: heat cured acrylic; D: comparative between the average of all 3 testing specimens curves
|
Impact strength, transverse flexural strength and elastic modulus
Descriptive statistics, One-way ANOVA and the LSD analysis were presented in tables 1-3.
Regarding the impact strength test results, there was a highly significant difference (p<0.01) between all the experimental groups. The polycarbonate (A) showed the highest mean values (233.43 KJ/M2) followed by the injectable acrylic (B) with (29.89 KJ/M2) while the lowest mean value was for the heat cure acrylic (C) with only (7.53 KJ/M2) (Table 1).
Table 1: Descriptive statistics, one-way ANOVA and LSD of Impact strength test
| (A) | (B) | (C) | ANOVA F- test | P- value | Compared groups | P. values | LSD | ||
| N | 10 | 10 | 10 | A | B | 0 | Sig. | ||
| Mean | 233.43 | 29.89 | 7.53 | B | C | 0 | HS | ||
| SD | 8.94 | 2.28 | 1.005 | C | 0 | HS | |||
| Min. | 227.03 | 28.25 | 6.81 | 5392.714 | 0.000 HS | HS | |||
| Max. | 239.82 | 31.53 | 8.25 |
On the other hand, a highly significant difference (p<0.01) were also noticed between all the experimental groups of the transverse flexural strength test. The experimental group (C) showed highest mean values (77.03 MPa) followed by group (A) with (69.12 MPa) while the lowest mean value was for group (B) (60 MPa) (Table 2).
Table 2: Descriptive statistics, one-way ANOVA and LSD of transverse flexural strength test
| (A) | (B) | (C) | ANOVA F- test | P- value | Compared groups | P. values | LSD | ||
| N | 10 | 10 | 10 | B | 0 | Sig. | |||
| Mean | 69.12 | 60 | 77.03 | C | 0 | HS | |||
| SD | 2.54 | 2.03 | 2.68 | A | C | 0 | HS | ||
| Min. | 66 | 56.4 | 73.2 | 122.27 | 0 | B | HS | ||
| Max. | 74.4 | 63.6 | 81.5 | HS |
Finally, the results of the elastic modulus test also indicate a highly significant difference (p<0.01) between all the experimental groups. The experimental group (C) showed the highest mean values (4.541 N/M2) followed by group (A) with (2.684 N/M2) while the lowest mean value was for group (B) with (2.366 N/M2) (Table 3).
Table 3: Descriptive statistics, one-way ANOVA and LSD of elastic modulus test
| (A) | (B) | (C) | ANOVA F- test | P- value | Compared groups | P. values | LSD | ||
| N | 10 | 10 | 10 | 1570.572 | B | 0 | Sig. | ||
| Mean | 2.68 | 2.36 | 4.54 | A | C | 0 | HS | ||
| SD | 0.004 | 0.14 | 0.07 | B | C | 0 | HS | ||
| Min. | 2.67 | 2.12 | 4.41 | 0 | HS | ||||
| Max. | 2.69 | 2.58 | 4.69 | HS |
Discussion
SEM result of fracture line of specimens after impact test
Heat cured specimen showed granular fracture line which indicate a brittle fracture, while injectable acrylic shows a river like line with straight cuts which indicate a ductile fracture, the polycarbonate deformed at impact test and the area of bend was cut and the area shows river wave configuration which is an indicator of ductile fracture.21
Impact strength test
The experimental group (polycarbonate) showed highest mean values followed by the (injectable acrylic) while the lowest mean values were for the (heat cure acrylic). This is due to the differences in the chemical structure between Polycarbonate and PMMA in general including (heat cured and injectable type), concerning with the polycarbonate’s high impact strength was a result of many factor related to its structure as it had a large aromatic content of phenyl groups (benzene ring) in its backbone, and moderately large pendent oxygen and hydrogen groups. These oxygen and hydrogen groups allow the tangle with the nearby polymer chains, and the formation of hydrogen bond. All these factors will lead to increase the resistance to intermolecular movements.22 Regarding the difference between PMMA types (heat cured and injectable type) is may be due to different processing technique, higher impact strength of injectable PMMA was related to the dual polymerization and the end polymer will contain less or none free monomer, while in heat cured more residual monomer and under polymerized polymer this will decrease its impact strength.3
The PMMA samples were fractured while polycarbonate samples did not fracture but bended after impact test, this is because the PMMA is thermoplastic amorphous polymer and its mechanical properties affected by the testing temperature and PMMA behavior will change from brittle to ductile as it became close to its glass transition temperature which is as average (104oC) and limited working range of working temperature , so it will undergo brittle fracture at room temperature which is not same as, Polycarbonate glass transition temperature (145oC) and, have a unique property that its less affected by temperature change and able to maintain its mechanical properties under a wide range of temperature change.16 Another explanation that polycarbonate has a large plastic deformation without crack or break, not same as that for PMMA.15 polycarbonate sample at room temperature is ductile and can be bended when force applied without being fractured.23
Transverse Flexure Test and Elastic Modulus
Transverse Flexural Strength
The transvers flexure test results showed that the experimental group (heat cure acrylic) had the highest mean value of flexural strength followed by the (polycarbonate), while the lowest mean value was for the (injectable acrylic) when measured at the maximum load applied.
This may be due to the polymers processed by injected molded technique are more flexible and ductile as expressed by Ippei H., that explain the higher results of flexure strength for heat cured acrylic in regarding to other experiment materials and why injected molded specimen didn’t fracture under the test.23 The polycarbonate and injectable acrylic differences related to each polymer unique chemical structure which influence its mechanical properties. Polycarbonate is produced by the linear polymerization reaction of bisphenol A (BPA) and phosgene COCl2 which reacted in more than one molecular space to form three dimension cross linked network and build up by condensation reaction this structure gives polycarbonate superior flexibility and elasticity at room temperature, while PMMA is formed by free radical polymerization reaction of the monomer with catalyst which reacted in one molecular space to form two dimension network and increase in size by addition reaction this make it brittle at room temperature.24
Another possible explanation of the differences between heat cured and injectable acrylic is within the same polymer family, the decrease in impact will cause increase of rigidity and vice versa, and the modification of the polymer to be suitable for the processing technique requirement.25
Elastic Modulus
A significant difference between all 3 experimental groups were found. The (heat cure acrylic) had the highest elastic modulus followed by the (polycarbonate), while the lowest elastic modulus was for the (injectable acrylic). The result was calculated from stress/strain curve at maximum load as shown in (fig 5), and showed a rigid behavior of the heat cured acrylic which can be explained as the under polymerization and the presence of residual monomer can affect the elasticity of the material make it brittle and fractured underload, while as for injected acrylic the dual polymerization and the trace to none residual and proceeding technique will lead to higher elasticity in comparison with heat cured acrylic.3 Another possible explanation of the differences within the same polymer family, Crompton T. describe the relationship between impact strength and rigidity as the decrease in impact strength will cause increase of rigidity (increase of elastic modulus) and vice versa.25
As for polycarbonate, the injected molded technique in addition to its chemical structure makes it more elastic than heat cured acrylic but less than injectable acrylic.24 Another possible explanation for the differences between injectable polycarbonate and injectable acrylic is the degree of crystallization.13
Ippei H., explained in his study, that all injected molded thermoplastic material had a lower elastic modulus and higher flexibility than heat cured acrylic.23
Conclusions
The following conclusions were reached after taking into consideration the limitations of this study
Samples made of heat cured acrylic showed higher flexure strength and elastic modulus with lower impact resistance in comparison with the samples of two other test materials.
Polycarbonate samples had higher impact resistance, moderate flexure strength and elastic modulus, in comparing with samples made of two other test materials.
Injectable acrylic samples exhibit moderate impact resistance, lowest flexure strength and elastic modulus in comparing with the other tested materials.
All thermoplastic materials in this study showed higher flexibility and ductility.
Acknowledgments
Authors wish to thank the dean as well as the assistant dean for scientific affairs of the college of dentistry, university of Baghdad for their kind support in facilitating using the available resources and materials to accomplish this work.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Funding Source
The authors have no funding to report.
References
- Diwan R. Materials Prescribed in the Management of Edentulous Patients. In: Zarb G, Bolander CL. Prosthodontic Treatment for Edentulous Patients. Ed 12. St. Louis, C.V. Mosby. 2004;190-207.
- Jagger D. C., Harrison A and J and t K. D. The reinforcement of dentures. Oral Rehabil. 1999;26:185–194.
CrossRef - Jafar G., Nafiseh A., Foad S. et al. Flexure strength of acrylic resin denture base processed by two different methods. 2014;8(3):148-152.
- Craig R. G and Powers J. M. Restorative dental materials. 11th St. Louis, Missouri.Elsevier. 2002; 640-4.
- Parvizi A., Lindquist T., Schneider R., Williamson D., Boyer D and Dawson D. V. Comparison of the dimensional accuracy of injection-molded denture basematerials to that of conventional pressure-pack acrylic resin. J Prosthodont. 2004;13:83–9.
CrossRef - Touraj N., Farshid S and Tony J. Impact of Packing and Processing Technique on Mechanical Properties of Acrylic Denture Base Materials. Materials. 2015;8(5):2093-2109.
CrossRef - Zbigniew R and Danuta N. Mechanical properties of hot curing acrylic resin after reinforced with different kinds of fibers. IJBMR. 2013;1(1):9-13.
CrossRef - Ahmed A., Medhat A and Abdelrahman M. A. Evaluation of a Newly Formulated Thermoplastic Monomer Free Complete Denture Base Material (Microbiological Study). IJSR. 2016;5(2):656.
CrossRef - Susanna S. Carbon-Graphite fiber reinforced polymers for implant superstructures. Dent Mater. 2007;23:1150-1156.
CrossRef - Alla R. K. Dental Materials Science 1st edition, Jaypee Brothers Medical Publishers (Pvt) Ltd., New Delhi: India. 2013;248-284.
CrossRef - Shikha N., Pankaj G., Himanshu S and Manmeet S. N G. NEW ERA IN DENTURE BASE RESINS A REVIEW. DJAS 1(III). 2013;136-143.
- Prashanti E., Jain N., Shenoy V. K., Reddy J. M and Shetty B. T. Flexible dentures A flexible option to treat edentulous patients. J Nepal Dent Assoc. 2010;11(1):85–7.
- Ken’ichiro H., Masaru N. Which of the material properties dominates surface roughness of diamond turned plastics, Shimo-okubo, Urawa, Saitama .JAPAN. 2000.
- Giulia B., Mario D and Del R. R. Poly(bisphenol A carbonate) Recycling High Pressure Hydrolysis Can Be a Convenient Way. Politecnico di Milano Italy.
- E. M. Physical properties of polymer. Hand book 2nd ed. New York, USA springer science +business media LLC. 2007.
- Nicholson J. W. The chemistry of polymer Cambridge UK RSC publishing. 2012.
- ISO 179-1, Plastics—Determination of Charpy impact properties. Part 1 Non-instrumented impact test. Geneva Switzerland: International Organization for Standardization. 2000.
- American dental association specification No. 12 for denture base polymer guide to dental materials and devices,7th edition, Chicago: Illiniois. 1999.
- Anusavice K. J. Philips science of dental materials. 11th Saunders Co. Philadelphia. 2008;162-169:190-195.
- Robert G. F., Richard M. F and Harold Q. F. Physics including human application, Harper and raw publisher, INT New York: USA. 1978.
- Jun C & Guangchun Y. Impact toughness and fractography in Mg-Y alloy. Mater Des. 2017;123: 64-68.
CrossRef - Brydson J. A. Plastics Materials,7th Butterworth-Heinemann. 1999.
- Ippei H., Yutaka T & Hiroshi S. The mechanical properties of injected molded thermoplastic denture base resins. Acta Odontal. 2011;69:75-79.
CrossRef - Joshua S. S. Impact mechanics of PMMA/PC multi- laminate with soft polymer interlayers, NA: Blacksburg. 2002.
- Crompton T. R. Physical testing of plastics. Rapra technology LTD Shrewsbury united kingdom. 2012








