Vian Sabah Abdulhameed1, Saif S. Saliem2 and Thair A.L. Hassan3
1Department of Periodontics, Dental Teaching Hospital, College of Dentistry, University of Baghdad, Bab-Almoadham, P.O.Box 1417, Baghdad, Iraq.
2Department of Periodontics, Dental Teaching Hospital, College of Dentistry, University of Baghdad, Baghdad, Iraq.
3Department of Oral and Maxillofacial Surgery, Dental Teaching Hospital, College of Dentistry, University of Baghdad, Baghdad, Iraq.
Corresponding Author E-mail: v.sabah@yahoo.com
DOI : https://dx.doi.org/10.13005/bpj/1305
Abstract
Preservation of interdental papilla and the need for esthetics are being progressively considered an essential criteria since crestal bone loss before loading may compromise implant success. Extensive and conserved flap designs frequently used in implant surgery. Salivary Alkaline phosphatase could be used to detect possible turnover process in the bone. This study evaluated crestal bone loss interproximally and to assess Alkaline phosphatase level occurring after implantation of single-tooth using two different flap designs. A total of 24 patients aged in range between 20-40 years underwent implant installation. Participants were divided in 2 groups: group A (12 patients) treated with extensive type, and group B (12 patients) with conserved one. Saliva was sampled from each patient five times (before, 2, 4, 12 and 24 weeks after surgery). An intraoral paralleling radiograph was taken as a baseline to evaluate the relation between the crestal bone and the dental fixture, one day and 24 weeks after surgery. The maximum amount of crestal bone loss on both mesial and distal sides for extensive was 0.6 mm while for conserved was 0.3 mm. The highest mean of Alkaline phosphatase in conserved type was seen in 2 weeks following surgery (7.04), while for extensive one was 6.95. The study results indicated that loss in the crestal bone interproximally was of practical importance and statistically significant less subsequent to the use of a conserved flap design when compared with the extensive type, also Alkaline phosphatase could be useful as a potential marker for bone turnover.
Keywords
Crestal bone loss alkaline phosphatase; Flap design;
Download this article as:| Copy the following to cite this article: Abdulhameed V. S, Saliem S. S, Hassan T. A. L. Evaluation of Crestal Bone Loss and Alkaline Phosphatase Level in Saliva According To Different Flap Designs in Single-Tooth Dental Implant Surgery (A Clinical Comparative Study). Biomed Pharmacol J 2017;10(4) |
| Copy the following to cite this URL: Abdulhameed V. S, Saliem S. S, Hassan T. A. L. Evaluation of Crestal Bone Loss and Alkaline Phosphatase Level in Saliva According To Different Flap Designs in Single-Tooth Dental Implant Surgery (A Clinical Comparative Study). Biomed Pharmacol J 2017;10(4). Available from: http://biomedpharmajournal.org/?p=17894 |
Introduction
One of the most significant advances in modern dentistry is the replacement of lost natural teeth with Osseo integrated dental implant. Implant dentistry considered as a progressive development compare to all other dental disciplines especially in the introduction of novel surgical techniques.1 The success of outstanding esthetic results with implant-supported single-tooth replacements has been obviously proved in several longitudinal studies.2,3 At this time, with better esthetic demands, Specialist must create a gingival contour that is harmonious with the gingival outline of the neighboring tooth and with an integral papilla, especially in esthetic zone.
To extent these aims, dental implants must be sited in adequate position and inclination.4,5Accomplishment of patient satisfaction involves not only the success of restorative requirements and remaining laboratory fabrication parameters, but as well the need of soft tissue in harmony with the neighboring teeth for reaching of successful esthetic results.6 Gingival esthetics has become a critical factor in the global success of an implant-supported tooth.7,8,9 Reconstruction or regeneration of peri-implant dental papillae is the most difficult and challenging feature of implant dentistry.10 Some efforts have been completed to correct the absence of papilla by surgical techniques; though, regeneration of papillae adjacent to dental implants is still challenging and is frequently unpredictable.11,12,13
The papilla shows a protective role on the neighboring periodontium, together with the alveolar bone crest, acting as a biological barrier against external invaders and inhibiting food impaction. Moreover, its loss can lead to cosmetic abnormalities and phonetic difficulties.14 The interdental papilla, present or absence, around dental implant depends on from the contact point to the crestal bone. Several probable etiologies of early crestal bone loss around dental implants including surgical trauma, flap designs, occlusal overload, periimplantitis, and others have been suggested.15
Extensive and conserved flaps design usually used in dental implant surgery depending on including or excluding of interdental papilla of the teeth adjacent to the edentulous site and this may have an effect on the crestal bone.16,17 To ensure of crestal bone loss depending on flaps design; two methods were used:
First one was the radiographic examination by using standardized paralleling radiographic technique.18
Second one was the biochemical test by using Alkaline phosphatase (ALP) in saliva as a marker in which it may be useful as a possible bone turnover marker to establish the diagnosis and prognosis of periodontal disease.19
Clinical periodontal parameters (PI, GI, PPD, BOP, CAL) for the teeth bounded the edentulous site were done for all patients at different intervals.
Materials and Methods
This clinical prospective study was conducted from October 2015 to October 2016. The sample included patients who attended the Department of Oral & Maxillofacial Surgery in the Teaching Hospital of College of Dentistry-Baghdad University for the purpose of implant placement. The whole study was approved by Ethical Committee of the College of Dentistry, University of Baghdad. According to SAC classification,20 only straightforward cases with bounded-single tooth replacement in anterior and premolar region were enrolled in this research with delayed implant placement protocol. An orthopantomograph (OPG), sample of whole unstimulated saliva, and clinical periodontal parameters for the teeth bounded the edentulous site, were done for all participants in this study pre-operatively.
A proper three sided full thickness mucoperiosteal flap design was planned, the participants were divided in 2 groups depends on flap design: group A with extensive flap design by including interdental papilla of the teeth bounded the edentulous site in the flap design, Figure 1, while group B with conserved flap design by excluding the interdental papilla of the adjacent teeth, Figure 2, then according to manufacturer instructions of the dental implant (DI) system (Easy Co. Ltd., chavanod, France), self-threaded titanium implant was inserted and tightened until acceptable primary stability was achieved. Prescription of proper antibiotics to the patients for 5 days [Augmentin tablet 625 mg / 8 hourly, Metronidazole tablet 250 mg / 8 hourly] with analgesia [ponstan tablet 500mg 1 tablet on need].
The patients were strictly informed to maintain biting on sterile gauze for 30 minutes postoperatively. They were properly instructed to put ice pack externally on the skin over the surgical site for the first 8 hours after surgery intermittently and to maintain good oral hygiene. All patients in both groups were informed to attend for taking the first paralleling radiographic technique, Figure 3, to evaluate the level of DI in relation to the crest as a baseline record and 24 weeks after surgery to evaluate this relation. The patients were seated on dental chair in upright position, then the sensor positioned in the holder that attached to the positioning ring (Figure 4). To ensure standardization in radiographic technique for the same patient after 24 weeks, the mesial side of the sensor was placed around 3 mm on the tooth adjacent to implanted area by using marker pen to identify the accurate position, this measured by using endodontic reamer size 55 with stopper and endodontic ruler.
 |
Figure 1: Extensive flap design |
 |
Figure 2: Conserved flap design |
 |
Figure 3: Paralleling radiographic technique for tooth site No. 12. |
 |
Figure 4: Digital sensor within sleeve and attached to the holder. |
Biochemical assays of alkaline phosphatase
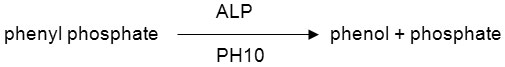
For enzyme analysis kit manufactured by BIOMARE (Angouleme, France) was used, the kit subjected to modification by a specialist (biochemist) to measure the activity of this enzyme in saliva. Colorimetric determination of alkaline phosphatase activity according to the following reaction:
Follow up and data collection
Each patient of both groups were informed to be seen 2, 4, 12, 24 weeks following surgery for saliva sampling, 12 weeks postoperatively for measurement of clinical periodontal parameters for the teeth adjacent to edentulous site, also 24 weeks postoperatively for measurement of clinical periodontal parameters and paralleling radiographic technique for the edentulous area. After that a second OPG was requested from the patient for overall examination of the implanted site and to ensure the precise position of the implant to prepare the patient for second stage surgery.
Statistical analysis
Data were analyzed using SPSS (statistical package of social science) version 19 software. Mean and standard deviation (SD) were calculated for quantitative variables. The independent sample t-test was used to compare the measured variables between two groups. Bonferron test for comparison between each two durations. In all of the tests, the result was considered statistically significant at p-value ≤ 0.05.
Results
A total of 24 patients were enrolled in this study; 5 males and 19 females; Age range from 20-40 years, mean age was 30.50 years (± 4.64). There was non-significant differences between extensive and conserved flap designs in ALP before, 2, 4, 12 and 24 weeks after surgery, The mean in crestal bone loss in group A on the mesial side was 0.46 mm (± 0.07), and on the distal side the mean was 0.45mm (± 0.07), in the group B was 0.17 mm (± 0.11) on the mesial side, while distally 0.12mm (± 0.10), resulting in highly significant difference between both groups (p < 0.000), Table 1. In the same group There was highly significant differences between ALP before surgery and 2, 4, 12 weeks after surgery and non-significant differences between before surgery and 24 weeks after surgery also there was highly significant differences between 2 weeks and 4, 12, 24 weeks after surgery and there was highly significant differences between 4 weeks and 12, 24 weeks after surgery also there was highly significant differences between 12 weeks and 24 weeks after surgery this all were for group A&B, Table 2. After a healing period of 24 weeks, all the implants were stable and successfully osseointegrated with 100% survival rate.
Table 1: Descriptive statistics and flap designs difference
| Variables | Durations | Descriptive statistics | Flap design difference
(d.f. =22) |
|||||
| Extensive flap | Conservative flap | |||||||
| Mean | S.D. | Mean | S.D. | Mean
Difference |
t-test | p-value | ||
| ALP
(IU/L) |
Before | 5.30 | 0.63 | 5.15 | 0.67 | 0.15 | 0.563 | 0.579 (NS) |
| After 2 weeks | 7.04 | 0.52 | 6.95 | 0.77 | 0.09 | 0.346 | 0.733 (NS) | |
| After 4 weeks | 6.55 | 0.44 | 6.38 | 0.69 | 0.17 | 0.727 | 0.475 (NS) | |
| After 12 weeks | 6.19 | 0.60 | 5.95 | 0.69 | 0.24 | 0.925 | 0.365 (NS) | |
| After 24 weeks | 5.40 | 0.66 | 5.28 | 0.69 | 0.12 | 0.422 | 0.677 (NS) | |
| Bone Loss
Difference (mm.) |
Mesially | 0.46 | 0.07 | 0.17 | 0.11 | 0.29 | 7.991 | 0.000 (HS) |
| Distally | 0.45 | 0.07 | 0.15 | 0.10 | 0.30 | 8.617 | 0.000 (HS) | |
Table 2: Bonferroni test for comparison between each two durations
| Duration | Extensive flap | Conservative flap | |||
| Mean
Difference |
p-value | Mean
Difference |
p-value | ||
| Before | After 2 weeks | -1.75 | 0.000 (HS) | -1.81 | 0.000 (HS) |
| After 4 weeks | -1.26 | 0.000 (HS) | -1.23 | 0.000 (HS) | |
| After 12 weeks | -0.89 | 0.000 (HS) | -0.80 | 0.000 (HS) | |
| After 24 weeks | -0.11 | 0.523 (NS) | -0.14 | 0.133 (NS) | |
| After 2 weeks | After 4 weeks | 0.49 | 0.003 (HS) | 0.57 | 0.000 (HS) |
| After 12 weeks | 0.85 | 0.000 (HS) | 1.01 | 0.000 (HS) | |
| After 24 weeks | 1.64 | 0.000 (HS) | 1.67 | 0.000 (HS) | |
| After 4 weeks | After 12 weeks | 0.36 | 0.010 (HS) | 0.43 | 0.005 (HS) |
| After 24 weeks | 1.15 | 0.000 (HS) | 1.09 | 0.000 (HS) | |
| After 12 weeks | After 24 weeks | 0.79 | 0.000 (HS) | 0.66 | 0.000 (HS) |
Discussion
To best of the authors´ knowledge, it is worthy to say that this was one of the few study in the literature that evaluated the crestal bone loss according to different flap designs in relation with ALP level in saliva for different intervals. The most critical factor for esthetically, and functionally success of single tooth supported DI is creation of soft tissue with intact papilla and gingival contour that is in harmony with the gingival drawing of the adjacent tooth. Widespread literature has complete that whether it is natural teeth or osseointegrated implants, the absence or presence of interdental papillae relied on the interproximal crestal bone, also suggested that the absence or presence of an intact interdental papilla depend directly on the underlying crestal bone.14 21
It has countered the interproximal crestal bone loss as one standard for DI success.22 23 According to this measure, bone loss of less than 0.2 mm per year following the implant’s first year of function is essential for long-term success. Salama et al 24 and Hermann et al 23 considered the interproximal bone height as a factor in completing optimal esthetic outcomes. Adell et al 25 who suggested that an average of 1.2 mm of crestal bone loss from the implantation during the healing period and first year after loading and 0.1 mm annually therefore, maintaining the interdental tissue for preserving the blood supply of the underlying bone diminishes the crestal bone loss around DIs, subsequent to ideal esthetic and functional consequences. Sunitha et al17 and Gomez-Roman16 suggested that the use of conserved flap design result in less crestal bone loss in comparison with extensive flap design. The results of this study was in agreement with Sunitha et al17 and Gomez-Roman16 in which there was highly significant difference in crestal bone loss between extensive and conserved flap designs.
The flap design proposed in this study (conserved flap design) preserved the interdental tissue, the aim of which was less traumatic preparation of the soft tissue. The interdental tissue was not comprised in the mucoperiosteal flap but was preserved at a width of 1 to 2 mm attached to alveolar bone, so more preservation for the crestal bone. While in extensive flap design, the bone loss increased, Moreover, adequate interdental bone height is fundamental key for the morphology and nutrition of an intact interdental papilla. The use of a conserved flap design to diminish interproximal crestal bone loss and possible loss of papillae around dental implants. This loss of crestal bone could be related to the fact that at whatever time bone is stripped of its periosteum, its nutrition is affected, which could result in resorption of the crestal bone.
Bone biomarkers play an important role in life disciplines and have begun to take on a better role in diagnosis, monitoring the outcomes and drug discovery.26 Numerous bio- markers in saliva were suggested as a diagnostic tests for periodontal destruction such as intracellular enzyme ALP. In healthy persons, its activities are within normal level. During diseases or destructions of periodontal ligaments, the cells become damaged, due to oedema or destruction of a cellular membrane, as a result of which there is an increased release into the gingival crevicular fluid (GCF) and saliva where its activity can be measured. Due to this, this enzyme can be biochemical markers of the functional condition of periodontal tissues.27
In this study, there was highly significant differences in ALP level before, 2, 4, 12 and 24 weeks postoperatively in both extensive and conserved flap designs as a result of destructive process during surgical procedures. In which ALP level in saliva elevated in comparison with healthy status, when there is breakdown in the periodontal tissues and this study agree with Kumar and Geeta28 that showed the potential value of salivary ALP level as indicator for periodontal tissue status it also agree with Deepika et al29 who suggested that intracellular enzymes including ALP are increasingly released from the damaged cells of periodontal tissues into the GCF and saliva.
In this study, there were highly significant differences in ALP between before, 2, 4 and 12 weeks after surgery in both groups. In which, the 2nd week after surgery recorded the highest elevation in the level of ALP in comparison with normal value of ALP, this result from the destructive process in the periodontal tissue as a result from flap design and drilling procedures. After the 2nd weeks there was dropping in the ALP result from the healing process in the periodontium. In the 24th weeks after surgery, ALP level returned to the normal value before surgery. In comparison between both groups, there was non-significant differences in the level of ALP; but the mean in group A is higher than in group B in all periods (2, 4, 12 and 24 weeks after surgery); it may be due to the small sample size that may consider a limitation for this study.
The results of this study indicate that the conserved flap design in dental implant is more savable for crestal bone in comparison with extensive flap, also ALP considered as an effective biomarker for bone remodeling process around dental implants and it is level was not a significant indicator between the two groups.
References
- Guruprasada A.M, Gen G.K, Thapliyal B, Pawar V.R. A comparative analysis of periimplant bone levels of immediate and conventionally loaded implants. Medical J Armed Forces India. 2013;69:41-47.
CrossRef - Hass R, Mensdorff-Pouilly N, Mailath G, et al. Single tooth implants: a preliminary report of 76 implants. J. Prosthet Dent. 1995;73:274-279.
CrossRef - Askary E.l A.S. Esthetic considerations in anterior single tooth replacement. Implant Dent. 1999;8:61–67.
CrossRef - De L.G.L. Aesthetic and prosthetic principles for single tooth implant procedures: an overview. Pract Periodontics Aesthet Dent. 1995;7:51–62.
- Phillips K, Kois J.C. Aesthetic peri-implant site development. The restorative connection. Dent Clin North Am. 1998;42:57–70.
- Smith D.E and Zarb G.A. Criteria for success of osseointegrated endosseus implant. J. prosthet Dent. 1989;62(5):567-72.
CrossRef - Reikie D.F. Esthetic and functional considerations for implant restoration of the partially edentulous patient. J. Prosth .Dent. 1993;70: 443–437.
CrossRef - Reikie D.F. Restoring gingival harmony around single tooth implants. J. Prosth Dent. 1995;74:47–50.
CrossRef - Chang M, Wennstrom J.L, Odman P. et al. Implant supported single-tooth replacements compared to contralateral natural tooth. Crown and soft tissue dimensions. Clin Oral Implants Res. 1999;10:185–194.
CrossRef - Lekovic V, Kenney E.B, Weinlaender M, et al. A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. J. Periodontol. 1999;68:563–570.
CrossRef - Beagle J.R. Surgical reconstruction of the interdental papilla: case report. Int J Periodontics Restorative Dent. 1992;12:145–151.
- Jemt T. Regeneration of the gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997;17:326–333.
- Newcovsky C.E, Moses O and Artzi Z. Interproximal papillae reconstruction in maxillary implants. J. Periodontol. 2000;71:308–314.
CrossRef - Tarnow D.P, Magner A.W, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J. Periodontol. 1992;63:995–996.
CrossRef - Dannan A. Crestal Bone Loss Around Dental Implants; A Short Communication. The Internet J Dent Sci. 2012;10(2):1-4.
- Gomez-Roman G. Influence of Flap Design on Peri-implant Interproximal Crestal Bone Loss around Single-tooth Implants. Int J Oral Maxillofac Implants. 2001;16:61–67.
- Raja S.V, MDS M.P.H, Ramakrishnan T, M.D.S, Kumar S.S, Pamela M.D.S, Emmadi M.D.S. Soft tissue preservation andcrestal bone loss around single-tooth implants. Journal of Oral Implantology. 2008;34 (4):223-229.
CrossRef - Nemli S.N, Bankoglu M, ngo G.r, Aydın C et al. Clinical and radiographic evaluation of new dental implant system: Results of a 3-year prospective study. J. Dent Sci. 2016;11:29-34.
CrossRef - Desai S, Shinde H, Mudda J et al. Levels of Alkaline Phosphatase (ALP) In Saliva of Patients with Chronic Periodontitis; a Clinical and Biochemical Study. Internet J Dent Sci. 2008;8(1):1937-8238.
- Antony D and Chen S. The SAC classification in implant dentistry. Eur J Orthod. 2009;31(564):1-13.
- Dardir M, Ul-Dahab O.A, Abuo-Elfadl K et al. A Comparative Clinical Study Between Bone Onlay Graft And Connective Tissue Graft In Reconstruction Of Interdental Papillae Between Two Implants. J. Am sci. 2011;7(9).
- Albrektsson T, Zarb G.A, Worhtington P, et al. The long-term efficacy of currently used dental implants: a review and proposed criteria for success. Int J Oral Maxillofac Implants. 1986;1:11–12.
- Hermann F, Henriette L, Palti A. Factors influencing the preservation of the peri-implant marginal bone. Implant Dent. 2007;11:162–9.
- Salama H, Salama M.A, Garber D, et al. The interproximal height of bone—a guide post to predictable esthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodont Aesthet Dent. 1998;10:1131–1141.
- Adell R, Lekholm U, Rockler B, et al. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. J. Oral Surg. 1981;10(6):387-416.
CrossRef - Sheetal S, patel S, agarwal P. Gingival crevicular fluid alkaline phosphatase as a potential diagnostic marker of periodontal. J. Indian Soc Periodontol. 2012;16(4):513-88.
CrossRef - Kaufman E and Lamster I.B. Analysis of saliva for periodontal diagnosis. J. Clin Periodontal. 2000;27(7):453-65.
CrossRef - Randhir K, Sharma G. October. Salivary Alkaline Phosphatase level as Diagnostic marker for periodontal disease. J. o Int Oral Health. 2011;3(5):81-86.
- Deepika V,Priya V.V, Bedre A et al. Salivary AST, ALP and CK Levels in Patients with Periodontitis. J. Pharm Sci & Res. 2015;7(6):341-343.








