Manuscript accepted on :August 03, 2017
Published online on: --
Plagiarism Check: Yes
R. Vedamanickam1, B. Harri Prasad2, R. Vinothkumar3 and Nagendram Dinakaran4
1Department of Medicine. Sree Balaji Medical College and Hospital, Chrompet, Chennai.
2Department of Medical Gastroenterology and Hepalology, Sree Balaji Medical College and Hospital, Chrompet, Chennai.
3Sree Balaji Medical College and Hospital, Chrompet, Chennai.
4Senior Gastroenterologist, Chennai.
DOI : https://dx.doi.org/10.13005/bpj/1259
Abstract
Long term intermittent management of symptomatic erosive and non - erosive gastro esophageal reflux (GERD) disease needs elucidation and evaluation. To evaluate the clinical value of maintenance intermittent with oral rabeprazole 20mg once a day versus omeprazole 20mg once a day in patients with symptomatic. This prospective study included 60 adults patients of either sex aged 21-65 years with mean age of 31.4 + 1.2 years with symptomatic history of GERD more than 3 months duration consist of both erosive and non - erosive esophagitis. They were divided into two groups one group enrolled with oral rabepazole 20mg once a day initial 4 weeks followed by intermittent maintenance therapy of same dose 4 days a week for 6 months, another group enrolled with oral omeprazole 20mg once a day for initial 4 weeks followed by intermittent maintenance therapy 4 days a week for 6 months. When symptoms recurs, on demand liquid antacid 15 ml given when heart burn occurs either day time or night time. The outcome was elicited on clinical score severity of symptoms. Patients rated symptoms severity on a 5 point scale. 0= no symptoms and 4= very severe symptoms that interfere considerable with daytime or sleep. The primary efficacy end point mean percentage of heart burn free days was significantly greater with rabeprazole when compared to omeprazole. Rabeprazole experienced a significantly higher percentage of symptoms free daytime 75.9% versus 62.7% in omeprazole group and night time 82.6% in rabeprazole compared to 61.4% in omeprazole group. Intermittent use of rabeprazole may be an effective maintenance treatment strategy in patients with GERD.
Keywords
GERD; erosive and non-erosive; gastritis; rabeprazole omeprazole
Download this article as:| Copy the following to cite this article: Vedamanickam R, Prasad B. H, Vinothkumar R, Dinakaran N. Effect of Intermittent Therapy With Rabeprazole 20mg in Patients With Symptomatic Gastroesophageal Reflux Disease-A Double Blind Omeprazole-Controlled Study. Biomed Pharmacol J 2017;10(3). |
| Copy the following to cite this URL: Vedamanickam R, Prasad B. H, Vinothkumar R, Dinakaran N. Effect of Intermittent Therapy With Rabeprazole 20mg in Patients With Symptomatic Gastroesophageal Reflux Disease-A Double Blind Omeprazole-Controlled Study. Biomed Pharmacol J 2017;10(3). Available from: http://biomedpharmajournal.org/?p=16325 |
Introduction
Proton pump inhibitors (PPI) are highly efficacious in providing symptomatic relief, healing erosions and improving quality of life in patients with symptomatic gastro esophageal reflux disease. (GERD)1 Worldwide Proton pump inhibitors (PPI) are being used in the treatment of GERD.2 Anti secretary agents such as esomeprazole, pantoprazole, ilaprazole, rabeprazole causes decrease in acid production and have high healing rates and rates of resolution of reflux symptoms at 4 weeks but do not help in long term maintenance intermittent therapy.3 In our randomized control trail long term intermittent rabeprazole therapy has proved efficacious than omeprazole.
Materials and Methods
Study Design
This prospective study concluded in 60 patients in department of Medicine Sree Balaji Medical College and Hospital, Chennai, India with GERD symptoms heat burn, regurgitation, epigastric pain, abdominal bloating, loss of appetite. This double blind rabeprazole, omeprazole study comprised of two phases. First phase symptomatic GERD patients either erosive or non-erosive esophagitis received 4 weeks course of either rabeprazole or omeprazole 20mg orally once a day and second phase received 4 days a week intermittently for 6 months of rabeprazole or omeprazole. If heart burn occurs during this period they were supplemented with on demand liquid antacid 20ml orally. Prior to entering the screening period written informed consent was obtained from each patients.
Patients
Male and Female patients aged 21-65 years of either sex with a minimum 3 months history of GERD symptoms. Patients were excluded if they had evidence of clinically significant cardiovascular, hepatic, renal, endocrinal, neurological, haematological abnormalities, known case of gastric or duodenal ulcer on long term PPI medication, patients who were on long term aspirin, non steroidal anti-inflammatory drugs, feeding or pregnant women, and those not willing for endoscopy. Efficacy and safety assessments patients were assessed at beginning of initial phase, during maintenance and after end of 6 months. Physical examination, vital signs and reflux clinical scoring system performed. Heart burn frequency was assessed as the number of days in a week in which symptoms occurred as 4 point scale 0=no symptoms 1= mild occasional symptoms 2= moderate symptoms 3= severe disturbing symptoms.
Results
Results of the study revealed that symptomatic response to therapy was over all in non-erosive esophasitis compared to erosive esophasitis 83.5% vs 59%. Maintenance group rabeprazole was superior when compared to omeprazole non-erosive group (88.5% to 66%) and in erosive group (79.2% to 52.8%) Fig.1. On demand antacid therapy requirement is less in rabeprazole 19.8% compared to omeprazole 29.7%. Both drugs were well tolerated and no major adverse side effect observed except headache in 13.2% in rabeprazole versus 6.6% in omeprazole.
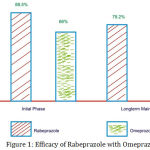 |
Figure 1: Efficacy of Rabeprazole with Omeprazole
|
Discussion
GERD is a common recurrent usually life long disorder resulting in disturbing health related quality of life in an individual4. Mono therapy for optimal management is insufficient. There are more studies indicate prokinetic with PPI combination is a better option. There are some studies indicate the demerits of prokinetics on long term.5,6 This study focus on using mean percentage of heart burn free days as the primary outcome measure. We demonstrated that a 6 months intermittent regimen of rabeprazole 20mg in symptomatic GERD patients provide adequate efficacy in 82.5% compared to 66% in omeprazole group. The percentage of heart burn free day time and night time periods were significantly better for rabeprazole group. Further more daily use of risk antacid on demand therapy for relief of heart burn was lower in rabeprazole group than omeprazole.7
Conclusion
Based on the symptomatic relief of intermittent rabeprazole for long term (6 months ) treatment with 20mg of rabeprazole was significantly more effective than 20mg of omeprazole. The overall efficacy and safety profile demonstrate in this study suggest that intermittent use of rabeprazole may be effective maintenance treatment strategy for patients with symptomatic GERD.
Reference
- Moayyedi P., Tolley N. J. gastro–esophageal reflux disease. Lancet. 2006:367;2086-100.
CrossRef - Bate C. M., Griffin S. M., Keeling P. W et al., Reflex Symptom relief with omeprozole in patients without unequivocal oesophatis aliment. pharmacol Ther . 1996;10:547-55.
- Carlson R., Dent J., Watts R. et al GERD in primary care an international study of different treatment strategies with omeprazole international GERD study group. EUR J Gastro enterol Hepatol. 1998;10;119-24.
CrossRef - KAJI M., FUJIWARA Y., SUGUSHIBA M. et al., prevalence of GERD on health –related quality of life. Journal of gastro enterology and Hepatology. 2010;25(6):1151-56.
CrossRef - Stanely M., Rotrosen J. The Benzamides pharmacology neurobiology and clinical aspects in: Advances in biochemical, psychopharmacology, 35. Raven press, NEW York. 1982:7-15.
- Rossi F., Forgione A. Pharmaco toxicological aspects of levosulpiride. Pharmacol Res. 1995;31:81-94.
CrossRef - Hungin A. P., Rubin G. P., O’Flanagon H. Long term prescribing of proton pump inhibitors on general practice. Br. J. Gen. Pract. 1999;49:451-453.







