Manuscript accepted on :May 25, 2017
Published online on: --
Plagiarism Check: Yes
karthick Sekar1, Prabhu Manickam Natarajan2 and Arva Kapasi3
1Saveetha dental college Saveetha university Chennai 600077 Tamilnadu, India.
2College of dentistry Gulf medical university UAE.
3Faculty of Dentistry, University Malaya 50603 Kuala Lumpur, Federal Territory of Kuala Lumpur.
Corresponding Author E-mail: drskarthick@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1136
Abstract
The application of tooth supported appliances of various types to the jaws and immobilization by intermaxillary fixation is the customary form of treatment in the management of fracture of the mandible and maxilla. Wire ligatures, arch bars and splints aide in the treatment of jaw fractures. They are applied to the teeth, alveolar processes and skeletal parts of the face or cranium. They function in the fixation of injured skeletal parts among one another and to the uninjured portions as well as the immobilization of fractured or loosened teeth. To Compare Arch Bar, Eyelets and Transmucosal Screws for Maxillomandibular Fixation in Jaw Fractures. Various modalities such as wire ligatures, arch bars and splints have been recommended but they have their associated morbidity including periodontal damage, decalcification under the splints and loosening and extrusion of the supporting teeth. 36 patients requiring maxillomandibular fixation who had jaw fractures are divided into three groups (arch bar, eyelets and transmucosal screws) the duration maxillomandibular fixation is 3-4 weeks. The plaque accumulation index (primary outcome) showed significant difference between all three groups. Mucosal damage time of fixation and time of removal (secondary outcome) showed significant between all three groups. For our study of maxillomandibular fixation comparing all three groups transmucosal screws has significantly less plaque accumulation less traumatic and less operating time.
Keywords
Application intermaxillary; treatment; fractures
Download this article as:| Copy the following to cite this article: Sekar K, Natarajan P. M, Kapasi A. Comparison of Arch Bar, Eyelets and Transmucosal Screws for Maxillo Mandibular Fixation in Jaw Fratcure. Biomed Pharmacol J 2017;10(2). |
| Copy the following to cite this URL: Sekar K, Natarajan P. M, Kapasi A. Comparison of Arch Bar, Eyelets and Transmucosal Screws for Maxillo Mandibular Fixation in Jaw Fratcure. Biomed Pharmacol J 2017;10(2). Available from: http://biomedpharmajournal.org/?p=15081 |
Introduction
The application of tooth supported appliances of various types to the jaws and immobilization by intermaxillary fixation is the customary form of treatment in the management of fracture of the mandible and maxilla. An ideal splint must provide stable attachment to the teeth or to the cranium- while doing minimal damage to the enamel, tooth-supporting structures, soft tissues and bones as well as affording good immobilization of the injured portions of the mandible and midface. The splint should be as inconspicuous as possible i.e. made of minimal amount of material and by allowing easy access to its elements, be amenable to easy care and maintenance 1. These requirements are satisfied to different degrees by the appliances to be discussed.
Wire ligatures, arch bars and splints aide in the treatment of jaw fractures. They are applied to the teeth, alveolar processes and skeletal parts of the face or cranium. They function in the fixation of injured skeletal parts among one another and to the uninjured portions as well as the immobilization of fractured or loosened teeth. For example, the injured mandible is attached to the uninjured maxilla and midface, the injured midface to the forehead, to the mandible and midface if both are involved to the cranium 1.
The oldest known devices for immobilization of fracture jaws are extra oral bandages also known as Craniofacial bandages. These have been known since the time of Hippocrates. The bandages and head supports recommended then were made of cloth or leather. Specific forms of these bandages are “Tunda Maxillae”, the “Capistrum Simplex” and “Duplex” 1.
The next step was the development of combined extra and intraoral appliances. With these, the teeth or the alveolar process of the fractured mandible were enveloped by a metal or rubber device and attached by means of bandages, screws, brackets or springs to the chin or a pressure pad located beneath the chin.
Today a good result of a mandibular fracture treatment should be considered nothing less than uneventful bony union with full recovery of function including a stable functional occlusion, as well as a full temporomandibular joint stabilization with a full range of motion. Other than fractures, various other definitive therapy include maxillomandbular fixation as an essential treatment plan.
The establishment of bone plating system as a treatment for fracture fixation has minimized the need of IMF, however short term IMF can be used intra operatively as a guide for alignment of fracture segments and to restore occlusion.
Dental circumferential wiring technique with or without IMF, has also been widely practiced to restore occlusion followed by fracture segment approximation, However these wires have some unfavorable effects on teeth and surrounding soft tissue and several workers have studied various aspects of this important issue.
Nevertheless these effects are reversible after removal of the splint. Occasionally progressive root resorption can be the most complex outcome after cementum injury in trauma fracture fixation.
Various complications of wire ligature, acrh bar and splints include compromised periodontal health, demineralisation of tooth beneath the splint and mobility and extrusion of supporting teeth. Along with being time consuming, tedious and painful, removal of these splints can turn out to be fatal when emergency removal of IMF is essential due airway obstruction
To bypass these disputes, the transmucosal screw has been advocated in the literature. The aim of this study is to compare arch bar,eyelets and transmucosal screws for maxillomandibular fixation in jaw fractures and to describe in detail the methodology and application of this system and to evaluate the merits and demerits of this system.
Materials and Methods
Arch Bars
Armamentarium
Erich Arch Bar
5- and 0.4-mm wire of stainless steel
Wire cutters and wiring forceps
Cheek and tongue retractors
Good light source and saliva ejector
Each arch bar is a flat stainless steel bar on which fleats or hooks are attached directed towards the gingival margin in each arch
Technique
If adequate number of teeth are available, it is recommended to place and secure the wire away from fracture site to avoid any unpredictable subluxation of the teeth adjacent to fracture site. In addition, provided there is sufficient fixation at the posterior segments, it is recommended to keep the inferior incisor portion unattached to arch bar to avoid their extrusion.
The arch bar initially is cut to a reasonable length and then is bent following the arch curvature. One-half of the arch is measured with the end of the loop, and then doubled the distance is cut off.
Stainless steel ligature wires of 0.4mm (some prefer 0-5mm specially for posterior region) are used for adapting the arch bar. The wires are inserted in the interproximal area around the neck of each available tooth (keep the wire below the greater circumference of the tooth by pressing the wire apically with the help of an assistant gripping the instrument like the Luniatschek while the wires are tightened closely with the tooth by twisting tightly to anchor the arch bar with the dental arch.
IMF is achieved using orthodontic elastic bands or wires inserted between the fleats of upper and lower arch bar. The wires are first pulled, tightened and then cut in a way so that the sharp ends of the wire are twisted and angled into the interdental area to avoid any soft tissue laceration. IMF is released by removing the elastic bands or wires.
Eyelets
Armamentarium
10 -20 prepacked autoclaved eyelet wires of 0.4-mm stainless steel wire lengthened 10% to a 5-cm length.
Cluster of 20 tie wires, 0.5-mm diameter and 15-cm long, of prestretched, soft stainless steel
Wire cutters and wiring forceps
Luniatschek
Cheek and tongue retractors
Good light source and saliva ejector
Eyelets wires are fabricated of 0.4mm diameter soft stainless steel wire which should be extended by 10% of the actual length for as to maintain the close fit of the wires after insertion. Overstretching hardens the wire, which then becomes brittle.
Eyelets wire are formed by making a loop at the center of each length of the wire around a shaft of 3mm diameter rod which is held in a vice. Three or four twist suffice, and the edges are trimmed off obliquely to create a sharp point with uniform lengths of the wire, so that the wire can be smoothly passed through the interproximal area. A sum of approximately 14 eyelet wires are collected and assembled by passing through a prefabricated wire loop through each eyelet followed by packing and autoclaving for instant use.
For general consideration, if short term immobility of the fracture segment is indicated ,relatively few eyelets are necessary, for example, one or two in each quadrant.
Technique
The wire ends are turned and clenched with the help of modified hemostat or special clip at around halfway to the curve so as to assist the wires through the interdental spaces without damaging the gingival papillae, lingual tissue or palatal tissue.
After selecting the tooth to be wired, both wire ends are introduced from the buccal side across the interdental region entering the lingual or palatal side from where they are grasped by a second pair of forceps which is operated by an assistant who after bending them, lodge the wire back through the adjacent mesial and distal inter dental spaces. The operator grips each wire as it appears out of the spaces and pulls it through.
Each wires is drawn around the mesial and distal tooth respectively; the distal wire entering into and out of the previously formed loop of the eyelets, both wire tail ends pulled, crossed and twisted tightly together while simultaneously the assistant retains the palatal or lingual portion of the wire beneath the maximum bulbosity of both the teeth with an appropriate instrument. Alternatively the wire can be brought out from underneath the loop allowing greater fixation for the eyelets. In the upper jaw, the eyelets should project above, and in the lower jaw, below the horizontal twist this averts the ends from disturbing each other.
The furthermost part of the wire are trimmed and angled interdentally to protect the lips and the cheeks from irritation, provided there are no secondary wires that are passed through. Vertical , anterioposterior and lateral motions of the jaw must supervised correctly throughout the duration of immobilization.
Insertion of wires is challenging in the lower incisors due to unsuitable shape for retention and crowded alignment, hence the wiring design can be refashioned avoiding the lower incisors teeth.
When some teeth are absent but not sufficient to necessitate an arch bar, or the fracture site is unsuitable, a wire can be connected to an isolated tooth by creating a clove hitch, and after tightening the wire loop, bringing about one end of the wire through the opposing jaw, anchoring it together with the other end.
Reduction of the fracture is mandatory prior to tightening the wires. Once the acceptable occlusion has been achieved, the posterior teeth should be secured to restrict excessive traction on the lower anterior teeth.
To withdraw the eyelets after the immobilization phase, it is recommended to remove the tie wires to permit a slight amount of jaw opening. Removal of eyelets can be postponed for one more week to control bony union by reconfirming the occlusion. Later eyelet wires are pulled out after releasing the wire untwining it in a counter clockwise rotations so that the buccal wire can be cut off.
Transmucosal Screws
Armamentarium
The armamentarium used in this study, namely the transmucosal screw was indigenously designed and fabricated in a cost effective way.
The armamentarium consisted of
Transmucosal screws
Instrument kit
Transmucosal Screws
The transmucosal screws are made up of stainless steel. These screws are 2 mm in diameter. They have a capstan head part and a thread part. The total length of the screw is 13mm, out of which the head measures 3 mm and the thread part measure 10 mm. The screws are self-tapping type.
Instrument Kit
The instrument kit consisted of
Screw driver; for tightening the screws
Screw holder; for driving them into the predrilled holes
Surgical bur; for drilling holes for the
Surgical Procedure
Maxillary Technique
The placement of three screws is recommended. Position of the screws can be anywhere in the dental arch but in practice we found that it is preferred ideally to position them, one in the midline, between the apices of central incisors and the other two between the canine and the first premolar, one in each arch. These self-tapping screws are implanted in the pre-drilled holes and the interface of the attached and reflected mucosa is the most favorable site.
First these areas are infiltrated with 2% lignocaine and 1:1,00,000 epinephrine. Tunnels/holes may be drilled transmucosally; there is no specific indication of a gingival incision. It is necessary to make certain that the drill passes in the midst of the roots of the teeth without causing any harm to the adjacent teeth. The bur is passed through the buccal and palatal/lingual cortices under copious irrigation. The screw is incoperated with the help of a screw holder. The screw is inserted and later tightened with a screwdriver till the flat portion of the head is well adapted against the buccal mucosa. It is mandatory not to perforate the palatal or lingual mucosa with the screw as it can lead to soft tissue irritation.
Mandibular Technique
As in the maxillary technique, three screws are recommended. These screws should be ideally placed opposite to the maxillary screws. The procedure is the same as that of the maxillary technique. In some patients with crowding of the dental arch, sometimes the screws cannot be placed exactly opposite to the maxillary screws, in the above-mentioned sites. In such cases it can be applied distally.
If the screws are placed in General anesthesia, it is easier to perform the surgical access and expose the fracture first. The screws are then placed while directly visualizing the teeth roots, nerves and fractures. When applied in this fashion, the screws do not interfere with the surgical access or placement of the reduction or fixation device. Temporary intermaxillary fixation is achieved using stainless steel wires (26 gauge) and occlusion is checked.
Table 6.4: Mean values
| Variables | N | Mean | Std. Dev | Minimum | Maximu m | |
| Erich Arc Bar | 12 | 38.5 | 12.681 | 20 | 60 | |
| Transmucosal Screws | 12 | 28.58 | 9.385 | 18 | 49 | |
| Age | Eyelets | 12 | 28.75 | 11.315 | 18 | 60 |
| Total | 36 | 31.94 | 11.856 | 18 | 60 | |
| Erich Arc Bar | 12 | 3.08 | 0.289 | 3 | 4 | |
| Plaque Accumulati on 1st week | Transmucosal Screws | 12 | 1 | 0 | 1 | 1 |
| Eyelets | 12 | 2 | 0 | 2 | 2 | |
| Total | 36 | 2.03 | 0.878 | 1 | 4 | |
| Erich Arc Bar | 12 | 3.5 | 0.522 | 3 | 4 | |
| Plaque Accumulati on 2nd week | Transmucosal Screws | 12 | 1 | 0 | 1 | 1 |
| Eyelets | 12 | 2 | 0 | 2 | 2 | |
| Total | 36 | 2.17 | 1.082 | 1 | 4 | |
| Erich Arc Bar | 12 | 3.92 | 0.289 | 3 | 4 | |
| Plaque Accumulati on 3rd week | Transmucosal Screws | 12 | 1 | 0 | 1 | 1 |
| Eyelets | 12 | 1.5 | 0.522 | 1 | 2 | |
| Total | 36 | 2.14 | 1.334 | 1 | 4 | |
| Erich Arc Bar | 12 | 4 | 0 | 4 | 4 | |
| Plaque Accumulati on 4th week | Transmucosal Screws | 12 | 1 | 0 | 1 | 1 |
| Eyelets | 12 | 1.33 | 0.492 | 1 | 2 | |
| Total | 36 | 2.11 | 1.389 | 1 | 4 | |
| Erich Arc Bar | 12 | 43.25 | 4.595 | 37 | 50 | |
| Transmucosal Screws | 12 | 10.17 | 2.918 | 5 | 16 | |
| Fixation time | Eyelets | 12 | 22.58 | 2.575 | 19 | 27 |
| Total | 36 | 25.33 | 14.245 | 5 | 50 | |
| Erich Arc Bar | 12 | 33.83 | 5.589 | 25 | 45 | |
| Transmucosal Screws | 12 | 6.58 | 1.165 | 5 | 8 | |
| Removal time | Eyelets | 12 | 16.17 | 1.697 | 14 | 20 |
| Total | 36 | 18.86 | 11.924 | 5 | 45 | |
Table 6.5: Kruskal-Wallis Test compare the mean values between groups
| Variables | P-Value |
| Age | 0.043 |
| Plaque Accumulation 1st week | 0.001 |
| Plaque Accumulation 2nd week | 0.001 |
| Plaque Accumulation 3rd week | 0.001 |
| Plaque Accumulation 4th week | 0.001 |
| Fixation time | 0.001 |
| Removal time | 0.001 |
Table 6.6: Mann-Whitney Test compare mean values between Erich Arc Bar and Transmucosal Screws
| Variables | P-Value |
| Age | 0.045 |
| Plaque Accumulation 1st week | 0.001 |
| Plaque Accumulation 2nd week | 0.001 |
| Plaque Accumulation 3rd week | 0.001 |
| Plaque Accumulation 4th week | 0.001 |
| Fixation time | 0.001 |
| Removal time | 0.001 |
Table 6.7: Mann-Whitney Test compare mean values between Erich Arc Bar and Eyelets
| Variables | P-Value |
| Age | 0.022 |
| Plaque Accumulation 1st week | 0.001 |
| Plaque Accumulation 2nd week | 0.001 |
| Plaque Accumulation 3rd week | 0.001 |
| Plaque Accumulation 4th week | 0.001 |
| Fixation time | 0.001 |
| Removal time | 0.001 |
Table 6.8: Mann-Whitney Test compare mean values between Transmucosal Screws and Eyelets
| Variables | P-Value |
| Age | 0.817 |
| Plaque Accumulation 1st week | 0.001 |
| Plaque Accumulation 2nd week | 0.001 |
| Plaque Accumulation 3rd week | 0.006 |
| Plaque Accumulation 4th week | 0.032 |
| Fixation time | 0.001 |
| Removal time | 0.001 |
Table 6.9: Friedman Test to compare the mean values of Plaque Accumulation between time points in each group separately
| Plaque Accumulation | P-Values |
| Erich Arc Bar | 0.001 |
| Transmucosal Screws | – |
| Eyelets | 0.001 |
Table 6.10: Wilcoxon Signed Ranks Test to compare the mean values of Plaque Accumulation between 1st and 2nd week in each group separately
| Plaque Accumulation | P-Values |
| Erich Arc Bar | 0.025 |
| Transmucosal Screws | 0.999 |
| Eyelets | 0.999 |
Table 6.11: Wilcoxon Signed Ranks Test to compare the mean values of Plaque Accumulation between 1st and 3rd week in each group separately
| Plaque Accumulation | P-Values |
| Erich Arc Bar | 0.002 |
| Transmucosal Screws | 0.999 |
| Eyelets | 0.014 |
Table 6.12: Wilcoxon Signed Ranks Test to compare the mean values of Plaque Accumulation between 1st and 4th week in each group separately
| Plaque Accumulation | P-Values |
| Erich Arc Bar | 0.001 |
| Transmucosal Screws | 0.999 |
| Eyelets | 0.005 |
Table 6.13: Wilcoxon Signed Ranks Test to compare the mean values of Plaque Accumulation between 2st and 3rd week in each group separately
| Plaque Accumulation | P-Values |
| Erich Arc Bar | 0.025 |
| Transmucosal Screws | 0.999 |
| Eyelets | 0.014 |
Table 6.14: Wilcoxon Signed Ranks Test to compare the mean values of Plaque Accumulation between 2st and 4th week in each group separately
| Plaque Accumulation | P-Values |
| Erich Arc Bar | 0.014 |
| Transmucosal Screws | 0.999 |
| Eyelets | 0.005 |
Table 6.15: Wilcoxon Signed Ranks Test to compare the mean values of Plaque Accumulation between 3rd and 4th week in each group separately
| Plaque Accumulation | P-Values |
| Erich Arc Bar | 0.317 |
| Transmucosal Screws | 0.999 |
| Eyelets | 0.157 |
Table 6.16: Fisher’s exact chi-Square Test to compare the propotions of Mucosal damage between groups
| Group |
Total |
P-Value |
||||||||
| Erich Arc Bar | Transmucos al Screws |
Eyelets |
||||||||
| N | % | N | % | N | % | N | % | |||
|
Gender |
Male | 12 | 100.0 | 11 | 91.7 | 9 | 75.0 | 32 | 88.9 |
0.294 |
| Female | 0 | 0.0 | 1 | 8.3 | 3 | 25.0 | 4 | 11.1 | ||
| Mucosal damage 1st week |
Present |
12 |
100.0 |
12 |
100.0 |
12 |
100.0 |
36 |
100.0 |
– |
| Mucosal damage 2nd week | Absent | 0 | 0.0 | 0 | 0.0 | 2 | 16.7 | 2 | 5.6 |
0.314 |
| Present | 12 | 100.0 | 12 | 100.0 | 10 | 83.3 | 34 | 94.4 | ||
| Mucosal damage 3rd week | Absent | 0 | 0.0 | 0 | 0.0 | 10 | 83.3 | 10 | 27.8 |
0.001 |
| Present | 12 | 100.0 | 12 | 100.0 | 2 | 16.7 | 26 | 72.2 | ||
| Mucosal damage 4th week | Absent | 0 | 0.0 | 12 | 100.0 | 12 | 100.0 | 24 | 66.7 |
0.001 |
| Present | 12 | 100.0 | 0 | 0.0 | 0 | 0.0 | 12 | 33.3 | ||
|
Traumatic |
No | 0 | 0.0 | 12 | 100.0 | 0 | 0.0 | 12 | 33.3 |
0.001 |
| Yes | 12 | 100.0 | 0 | 0.0 | 12 | 100.0 | 24 | 66.7 | ||
| Total | 12 | 100.0 | 12 | 100.0 | 12 | 100.0 | 36 | 100.0 | ||
Table 6.17: Fisher’s exact chi-Square Test to compare the propotions of Mucosal damage between Erich Arc Bar and Transmucosal Screws
| Group |
Total |
P-Value |
||||||
| Erich Arc Bar | Transmucos al Screws | |||||||
| N | % | N | % | N | % | |||
|
Gender |
Male | 12 | 100.0 | 11 | 91.7 | 23 | 95.8 |
0.994 |
| Female | 0 | 0.0 | 1 | 8.3 | 1 | 4.2 | ||
| Mucosal damage 1st week |
Present |
12 |
100.0 |
12 |
100.0 |
24 |
100.0 |
– |
| Mucosal damage 2nd week |
Present |
12 |
100.0 |
12 |
100.0 |
24 |
100.0 |
– |
| Mucosal damage 3rd week |
Present |
12 |
100.0 |
12 |
100.0 |
24 |
100.0 |
– |
| Mucosal damage 4th week | Absent | 0 | 0.0 | 12 | 100.0 | 12 | 50.0 |
0.001 |
| Present | 12 | 100.0 | 0 | 0.0 | 12 | 50.0 | ||
|
Traumatic |
No | 0 | 0.0 | 12 | 100.0 | 12 | 50.0 |
0.001 |
| Yes | 12 | 100.0 | 0 | 0.0 | 12 | 50.0 | ||
| Total | 12 | 100.0 | 12 | 100.0 | 24 | 100.0 | ||
Table 6.18: Fisher’s exact chi-Square Test to compare the propotions of Mucosal damage between Erich Arc Bar and Eyelets
| Group |
Total |
P-Value |
||||||
| Erich Arc Bar | Eyelets | |||||||
| N | % | N | % | N | % | |||
|
Gender |
Male | 12 | 100.0 | 9 | 75.0 | 21 | 87.5 |
0.217 |
| Female | 0 | 0.0 | 3 | 25.0 | 3 | 12.5 | ||
| Mucosal damage 1st week |
Present |
12 |
100.0 |
12 |
100.0 |
24 |
100.0 |
– |
| Mucosal damage 2nd week | Absent | 0 | 0.0 | 2 | 16.7 | 2 | 8.3 |
0.478 |
| Present | 12 | 100.0 | 10 | 83.3 | 22 | 91.7 | ||
| Mucosal damage 3rd week | Absent | 0 | 0.0 | 10 | 83.3 | 10 | 41.7 |
0.001 |
| Present | 12 | 100.0 | 2 | 16.7 | 14 | 58.3 | ||
| Mucosal damage 4th week | Absent | 0 | 0.0 | 12 | 100.0 | 12 | 50.0 |
0.001 |
| Present | 12 | 100.0 | 0 | 0.0 | 12 | 50.0 | ||
| Traumatic | Yes | 12 | 100.0 | 12 | 100.0 | 24 | 100.0 | – |
| Total | 12 | 100.0 | 12 | 100.0 | 24 | 100.0 | ||
Table 6.19: Fisher’s exact chi-Square Test to compare the propotions of Mucosal damage between Transmucosal Screws and Eyelets
| Group |
Total |
P-Value |
||||||
| Transmucosal Screws |
Eyelets |
|||||||
| N | % | N | % | N | % | |||
|
Gender |
Male | 11 | 91.7 | 9 | 75.0 | 20 | 83.3 |
0.590 |
| Female | 1 | 8.3 | 3 | 25.0 | 4 | 16.7 | ||
| Mucosal damage 1st week |
Present |
12 |
100.0 |
12 |
100.0 |
24 |
100.0 |
– |
| Mucosal damage 2nd week | Absent | 0 | 0.0 | 2 | 16.7 | 2 | 8.3 |
0.478 |
| Present | 12 | 100.0 | 10 | 83.3 | 22 | 91.7 | ||
| Mucosal damage 3rd week | Absent | 0 | 0.0 | 10 | 83.3 | 10 | 41.7 |
0.001 |
| Present | 12 | 100.0 | 2 | 16.7 | 14 | 58.3 | ||
| Mucosal damage 4th week |
Absent |
12 |
100.0 |
12 |
100.0 |
24 |
100.0 |
– |
|
Traumatic |
No | 12 | 100.0 | 0 | 0.0 | 12 | 50.0 |
0.001 |
| Yes | 0 | 0.0 | 12 | 100.0 | 12 | 50.0 | ||
| Total | 12 | 100.0 | 12 | 100.0 | 24 | 100.0 | ||
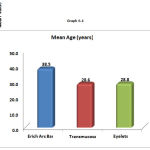 |
Graph 6.1
|
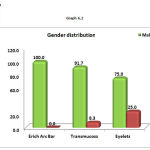 |
Graph 6.2
|
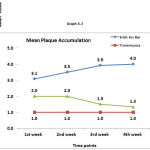 |
Graph 6.3
|
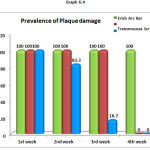 |
Graph 6.4
|
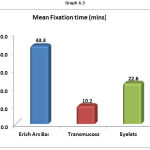 |
Graph 6.5
|
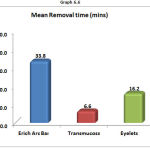 |
Graph 6.6
|
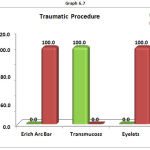 |
Graph 6.7
|
 |
Figure 1
|
 |
Figure 2
|
 |
Figure 3
|
 |
Figure 4
|
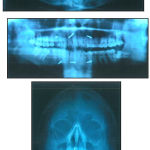 |
Figure 5
|
Results
The plaque accumulation index (primary outcome) showed significant difference between all three groups. Mucosal damage time of fixation and time of removal (secondary outcome) showed significant between all three groups.
Discussion
Re-establishing the dental occlusion to the pre-trauma status has been the main stray of successful treatment of fracture of the jaws 4. Intermaxillary fixation with the use of arch bars has been the standard treatment for most mandibular and maxillary fractures with or without open reduction. Arch bars have been applied to respective arches with circumdental stainless steel wires. Stabilization of the fractures has been achieved using intermaxillary fixation wires or elastics 5.
An adverse sequalae of usage of arch bars or wire loops for splinting causes marginal conditions to be comprimsed causing gingivitis and increased tooth mobility. These conditions however, are reversible after the removal of splints3. in their article on effects of interdental wiring in jaw fractures, state that wiring of teeth to splint jaw fractures leads to alterations in the periodontium. These changes may regress once the wiring is removed.
Tooth mobility after maxillo-mandibular fixation has been surveyed in some researches. 3, 6 and show a slow return to ideal values after cessation of maxillo-mandibular fixation. These may be the aftermath of the orthodontic forces that are originated by tightening of the wires on the teeth.
The wire encompassing the cervical region of the tooth theoretically accomplishes the conditions that may lead to start an external root resorption. The ligature may well be traumatizing element in itself that causing damage to the protective layer of cementoblasts and cementoid on the surface of the root. The wiring may aswell induce inflammation in the marginal tissues 7.
With the upcoming quantity of people infected with human immuno-deficiency virus, oral and maxillofacial surgeons need to take precautions to avoid inadvertent skin puncture. Scully and Porter has analysed the possibility of transmission of human immuno-deficiency virus infection amongst the patients and the dental staff 8. They verified that the primary occupational risk for the dental health care worker is from sharps injury. With the approach of using arch bars, usually 16 to 22 interdental wires are passed. Each wire passed has the plausibility for unintentional skin puncture. For the patients with a high probability of having HIV infection (i.e., intravenous drug abusers or homosexuals) who need maxillo-mandibular fixation, an alternative technique of transmucosal screws is best suited 9.
As surgical approach of rigid skeletal fixation by the method of open reduction have developed into a more sophisticated and widely used procedure hence, long-term maxillo-mandibular fixation no more seems to be needed. Consequently today the use of maxillo-mandibular fixation is generally narrowed down to a short ranged duration intra operatively and post operatively.
To circumvent the above-mentioned dilemma the use of transmucosal screws as an alternative method has been tried and analysed.
Intraoral cortical bone screw technique has concluded to be greatly advantageous. Primarily the jeopardy of percutaneous contamination to both, surgeon and patient has been scaled down. Learning the technique is straightforward and easy to practice. The operating time has been reduced from over one hour to nearly fifteen minutes. The fixation attained is comparable to that with arch bars. They are also absolutely compatible with bone plates. Increased compliance, enanced oral hygiene and a reduced rate of infection have been realized.
The technique is not dependent on the number of teeth present and is suitable to be done under local anesthesia. In addition, undisplaced fractures in edentulous mandibular segments may be successfully treated as well, provided that dentures are available. They are peculiarly satisfactory for patients with extensive crown and bridgework.
There are of course a few disadvantages or limitations to these procedures. It demands the availability of specially made self-tapping bone screws, which must be subsequently removed. It is a advanced technique that requires a course of acclimation, and it is not convenient for all fractures.
The most suitable fractures are those that are relatively undisplaced. The technique is useful for both symphysis and para-symphysis fractures with or without intraoral bone plates.
The intraoral cortical bone screw technique is not generally preferred for severely comminuted fractures, extensive dentoalveolar bone fractures, missile injuries to the jaws and paediatric fractures.
Reports have been published cautioning the use of bicortical intermaxillary fixation screws 11-14. Careful handling is advised in the course of insertion of the screws with regards to both positioning and insertion torque. While the complications have been minor and comfortably managed, they have resulted in the need for further treatment. A cautious manipulation throughout the drilling of the bur hole is crucial, with passive drill speed and copious irrigation with sterile saline. The screw should be passively implanted at constant speed and should not be forced if resistance is perceived (Likely to be engaging the roots of the teeth).
Conclusion
From our study of maxillomandibular fixation with intraoral cortical bone screws, we found that it provides a comparable fixation, significantly decreased operating time and less plaque accumulation. Transmucosal screws include ease of use, quickness, shortened operating time.
Furthermore, compared with arch bars and eyelets there is nil injury to the gingival margin and gingival health in easier to maintain. So transmucosal screws is identified to better method in comparison with arch bar and eyelets for comparing the plaque index of each method. But the technique is acceptable for interim intraoperative fixation and elastic traction. Wound healing of the periodontium after the surgery should also be taken into consideration.
References
- Andreason O. Textbook and colour atlas of traumatic injuries to the teeth. 1994; 449 – 450.
- Arthur , Berardo N. A simplified technique of maxillo – mandibular f ixation. J. Oral Maxillofacial Surgery. 1989; 47:1234.
CrossRef - Avery M.E., Johnson P. A. Surgical glove perforation and maxillofacial trauma; to plate or to wire. Br. J. Maxillofacial Surg. 1992; 30: 31 – 35 .
CrossRef - Benninger S., Gupta N., Gilmore K. Intraoperative infectious disease exposure to otolaryngology operating room personnel. Laryngoscope. 1991; 101 : 1276 – 1279.
CrossRef - Busch F. Maxillo – mandibular f ixation with intraoral cortical bone screws. Laryngoscope. 1994; 104:1048.
CrossRef - Carljones C. Trans alveolar screws. O.O.O. 1997; 84:458.
- Champey , Harle. Atlas of craniomaxillofacial osteosynthesis. Miniplates, microplates and screws. Chapter
- Stabilization of the occlusion. Atlas of the Oral Maxillofacial surgery. Clinics of North America. 1997;5:1.
- Coburn C., Kennedy D. W.G. Complications with intermaxillary f ixation screws in the management of fractured mandible. Br. J. Oral Maxillofacial Surg. 2002; 40:241 -243.
CrossRef - Davidson , Stabile B. Acquired immuno- deficiency syndrome, precautions for oto – laryngology-head and neck surgery. Arch. Otolaryn. Head and Neck Surg. 1991; 117: 1343 – 1344 .
CrossRef - Farr D.R., Whear M. Intermaxillary fixation screws and tooth damaged. Br. J. Oral Maxillofacial Surg. 2002; 40:84 – 85.
CrossRef - Homes, Ia Rowe and Williams maxillofacial injuries. 1994; 283 -327.
- Issacs S., Sykes J.M . Maxillo –mandibular fixation with intraoral cortical bone screws. Laryngoscope. 1995; 105: 109 -113.
CrossRef - Caution in the use of bicortical intermaxillary f ixation screws. Br. J. Oral Ma xillofacial Surg. 2000; 38:5
- Prabhu MN, et al.Osteoporosis and Periodontal Disease – A Review”. International Journal of innovations in Dental Sciences, December 2016, Vol. 1(1), 27-37.
- Prabhu MN et al. Analgesics Used In Periodontal Surgery” International Journal of innovations in Dental Sciences, December 2016, Vol. 1(1), 1-9.
- Prabhu MN, et al. The role of antibiotics in treatment of chronic Periodontitis”. International Journal of Dental Sciences and Research , 2014, 2 (1), 16-18.
- Prabhu MN, Priyavadhana Prabhu. Wound Healing in Periodontics,Biosciences Biotechnology Research Asia, August 2014. 11(2), 791-796.
CrossRef







