Manuscript accepted on :March 07, 2017
Published online on: --
Plagiarism Check: Yes
Marzya Abdramanovna Mamyrbayeva and Galina Dautovna Zhumagaliyeva
West Kazakhstan State Medical University named after Marat Ospanov, 030019, Kazakhstan, Aktobe region, Aktobe, Maresyev street, 68.
DOI : https://dx.doi.org/10.13005/bpj/1095
Abstract
Our studies showed that prolonged jaundice hyperbilirubinemia is not always evaluated by pediatricians as a factor in the debut of heavy damage of the hepatobiliary tract. The lack of competence of the physician in the interpretation of the obtained results of serological studies leads to erroneous diagnosis. The main difficulty in the management of jaundice of the newborn is, on the one hand, the high frequency of uncomplicated forms (56%). On the other hand, the risk of complications in a case of missed pathological hyperbilirubinemia is very high. And it imposes huge responsibility on the physician in the diagnosis and choice of treatment.
Keywords
Neonatal hyperbilirubinemia; newborn; intrauterine infectious
Download this article as:| Copy the following to cite this article: Mamyrbayeva M. A, Zhumagaliyeva G. D. Keeping Babies With Jaundice Syndrome in Primary Health Care. Biomed Pharmacol J 2017;10(1). |
| Copy the following to cite this URL: Mamyrbayeva M. A, Zhumagaliyeva G. D. Keeping Babies With Jaundice Syndrome in Primary Health Care. Biomed Pharmacol J 2017;10(1). Available from: http://biomedpharmajournal.org/?p=13856 |
Introduction
Primary health care physicians in their practice are experiencing difficulties in differential diagnostics of jaundice syndrome in newborns, occurring with protracted course. Neonatal jaundice is a common problem encountered in newborns. More than 50% of all full-term babies and 85% of premature babies are visibly jaundiced during the first week of life [1]. Over the past decade, views on the tactics of management of children with neonatal jaundice were significantly changed, so you can often find divergent views on this issue among practical neonatologists. The main difficulty in the management of jaundice of the newborn is, on the one hand, a high frequency (56%) of uncomplicated forms [2]. On the other hand, the risk of complications in a case of missed pathological hyperbilirubinemia is very high. And it imposes a huge responsibility on the physician in the diagnosis and choice of treatment. The probability of occurrence of problems becomes high in the case when the newborn baby’s jaundice lasts longer than three weeks. In view of the heterogeneity of jaundice, the aim of our study was to investigate the prevalence of neonatal jaundice, and its associations with viral infections, bacterial and protozoal microorganisms [3,4].
Materials and Methods
We have analyzed 645 case histories of children (form 112/y) with neonatal jaundice due to infection. Children were under the observation in hospitals in Aktobe in 2012-2014 years. Were selected 2 groups of children: a) 285 infants with neonatal jaundice with clinical and laboratory parameters of lesions of the liver parenchyma with signs of cytolysis and cholestasis; b) 360 newborns with hyperbilirubinemia due to indirect fractions without a syndrome of cytolysis and cholestasis. According to the Clinical Protocol of diagnosis and treatment of neonatal jaundice [5], the pediatrician who is treating the child must be able to assess an individual “safe” level of bilirubin in a newborn with jaundice and predict its potential growth using a modified scale of Cramer and a physical examination.
The Results of the Study
Was revealed the frequency of neonatal jaundice and infectious viral hepatitis among children in the first year of life by evaluating case histories of a child development (form #112/y) for the last three years (2013 -2015) in urban hospitals (table 1).
Table 1: The prevalence of neonatal jaundice (NJ) and infectious viral hepatitis (IVG) at the medical-preventive institutions of Aktobe
| Medical institutions | 2012 year | 2013 year | 2014 year | ||||||
| The number of children under one year | Children with NJ | Children with IVG | The number of children under one year | Children with NJ | Children with IVG | The number of children under one year | Children with NJ | Children with IVG | |
| Polyclinic №1 | 1651 | 75 | 1589 | 67 | 1678 | 43 | |||
| Polyclinic №2 | 2880 | 178 | 2287 | 147 | 2584 | 148 | |||
| Polyclinic №3 | 860 | 32 | 10 | 841 | 48 | 13 | 942 | 43 | 17 |
| Polyclinic «Bolashuck» | 201 | 23 | 219 | 45 | 228 | 14 | |||
| Polyclinic №4
without affiliation |
1258 | 28 | 1646 | 57 | 1663 | 77 | |||
| Polyclinic №5+ Polyclinic №6 | 903 | 83 | 880 | 86 | 1032 | 67 | |||
| Clinical-diagnostic centre | – | 21 | – | 2 | – | 6 | |||
| КСМ | 308 | 22 | 300 | 24 | 379 | 31 | |||
| Railway- Polyclinic | 502 | 10 | 590 | 17 | 548 | 12 | |||
| Total | 8563 | 472 | 116 | 8352 | 631 | 183 | 9054 | 441 | 104
|
| % | 5,5 | 1,35 | 7,5 | 2,2 | 4,9 | 1,15 | |||
| The rate per 1,000 | 55,1 | 13,5 | 75,5 | 21,9 | 48,7 | 11,5 | |||
The frequency of neonatal jaundice among newborns in Aktobe in different years varies without trends within 4.9 to 7.5% (the rate per 1000 children in the first year of life is 48,7 – 75,5). There further testing by ELISA and PCR have detected persistence of the virus in the peripheral blood. Intrauterine infectious viral hepatitis among newborns occurs with a frequency of 1.15-2.2%, which is consistent with the literature data. And the incidence rate of hepatitis per 1000 babies is multidirectional: 13,5 – 21,9 – 11,5.
Statistical data of morbidity on individual diseases does not give a clear picture of the prevalence of congenital infections of TORCH–complex in children of the first year of life, in particular causing damage to the liver. In herpes virus infection we should distinguish between the “infection” and “morbidity” as in the case of infection it does not always develop pathology or its formation is deferred.
To identify the prevalence of infection and morbidity were analyzed the research results of the presence of antibodies to antigens of major pathogens of TORCH-complex in the peripheral blood of children in the first year of life in combination with clinical manifestations (table 2).
Table 2: The incidence of antibodies IgG and IgM to antigens of the causative agents of intrauterine infections among children in the first year of life
|
CMVI |
Herpes virus infection | Toxoplasmosis |
Chlamydia |
|
| The number of patients with positive IgM and IgG antibodies to the antigens of the pathogen | 40 (8,0,%) | 3 (1,5%) | 1(0,8%) | 1 (0,89%) |
| The number of patients with a positive IgG to antigens of the pathogen | 456 (91,0%) | 182 (91%) | 7 (5,6%) | 4 (3,57%) |
| The number of patients with negative results | 5 (1,0%) | 15 (7,5%) | 117 (93,6%) | 107 (95,5%) |
| Were examined in total | 501 | 200 | 125 | 112 |
Was conducted a survey of 938 sera of sick children aged from 3 days to 12 month of life on markers of intrauterine infections: among them for the markers of CMV – 501, for the markers of HSV – 200 children, for the markers of toxoplasmosis – 125, for the markers of chlamydia – 112. All of them were hospitalized in municipal and regional children’s clinical hospitals in Aktobe in 2012 year. Antibodies IgM and IgG to CMV and HSV antigens were determined by ELISA [6, 7].
The ELISA showed a high detection rate of antibodies to CMV (99,0%) and to HSV (92,5%) among the examined children in the first year of life, comparing to a slight detection of ТОХО antibodies (17,6% to 10.2%) and chlamydia (5%). Prevalent was the detection of CMV IgG (91,7%), and CMV IgM was determined only in 8.0% of cases. CMV IgM, indicating an acute phase of the disease, was identified in the majority of the surveyed (29 infants) without clinical manifestations of the disease. In a small number of patients a positive result of CMV IgM was combined with the clinic of conjugational jaundice (5), fetal hepatitis (3 patients), intrauterine infection (2 patients) and intrauterine pneumonia (in 2 patients). Conversely, antibodies to CMV IgG showing the absence of activation of the virus and reparation, were observed together with the clinic of the manifest diseases.
It should be noted that the diagnoses of the sending organization at the admission were not intrauterine infection, but the conjugation and/or neonatal jaundice. With the diagnosis “Neonatal jaundice” from the polyclinics №2 and №4 of Aktobe in 2010 year were sent 199 (5.6% of the total number of births of newborns, geographically fixed to the polyclinics), 2011 year – 304 (8,1%), 2012 year – 407 (9,8%), 2013 year – 433 (9,8%) newborns. The number of hospitalizations of newborns with a diagnosis of “neonatal jaundice” and babies over 1 month of living with a diagnosis of “conjugational jaundice” has increased. Among them in 2011 year 5.59% were hospitalized with a final confirmed diagnosis of “fetal hepatitis” – 5,59%, in 2012 year – 1,47%. Only in a regional clinical hospital the annual number of patients with infectious viral hepatitis ranges from 4% to 4.8% of the total treated number. This indicates inconsistent trends in the prevalence of liver damage. And with unpredictable course of the neonatal jaundice doctors of the outpatient segment according to the strategy of integrated management of childhood illness in the identification of “severe jaundice” immediately sent the newborn to the hospital.
Analysis of case histories of children identified the following shortcomings observation by the physicians of primary care:
not all doctors remember the terrible symptoms of complicated hyperbilirubinemia;
infants that are urgently hospitalized are usually already have the complications in the form of hemorrhagic syndrome; and sometimes even death.
Typical omissions of the physician in primary care of the newborn from the hospital:
in 75% a template description of jaundice. Is not determined the localization of jaundice according to the modified scale of Kramer.
in 80% of cases is not fixed and is not detected a saturated color of urine.
in 98% is not fixed an attention on flatulence and abdominal distension in a newborn with jaundice.
a template record in the history of the development of the child: “The liver and spleen are not increased.” In 62% were not determined the size of the liver and spleen.
In the presence of jaundice the primary care doctors are usually making the following mistakes:
45% of primary care doctors remember about the symptoms.
55% do not know the terrible symptoms of dangerous hyperbilirubinemia.
According to the Protocol of “Neonatal jaundice” is required the inspection of infectious disease specialist. Only in 1% of newborns they were examined by an infectious disease specialist. In 100% they were examined by the surgeon and the neurologist.
Typical omissions by physicians in the supervision of children on an outpatient basis:
in 63% are not recorded the early detection of signs of “dangerous jaundice” and thus there is no regular clinical assessment of the newborn (every 8-12 hours) according to the Protocol; – in 100% fails the implementation of Protocol (“Physical examination”), especially is not estimated a color of the skin after lightly pressing with a finger down to the level of the subcutaneous fat;
ultrasound of the abdomen and liver was performed only in 35% of cases when it was recommended by the leading experts and according to the testimony in hospital;
is not taken into account the level of alkaline phosphatase and gammaglutamyltranspeptidase for exclusion of neonatal cholestasis in the pathology of the hepatobiliary system, which are not included in the guaranteed volume of research for population in an outpatient setting;
infants that are urgently hospitalized are usually already have the complications in the form of hemorrhagic syndrome; and sometimes even death.
Discussion of the obtained Date
Our studies showed that jaundice with prolonged hyperbilirubinemia is not always evaluated by pediatricians as a factor as the debut of heavy damage to the hepatobiliary tract and the lack of competence of the physician in the interpretation of the obtained serological results by ELISA lead to erroneous diagnosis. The examination of the patient, not matching the protocols and methodological requirements, leads to the fact that the doctors of practical health care with favorable clinical outcome are discharging patients with a diagnosis of “Neonatal or conjugational jaundice”, without taking into account the presence of CMV IgG antibodies. The increasing of jaundice intensity after its physiological decline, or a prolonged duration of hyperbilirubinemia, the gradual increase in size of the liver with the change in its density, the appearance of aholic stool and dark color of urine may be the main clinical markers of neonatal cholestasis [8, 9, 10].
Were identified common misconceptions:
the false confidence in the diagnosis of “conjugational jaundice” when there is a trend to decrease in the concentration of total bilirubin in the absence of initial signs of cytolysis or aholic stool;
wrong interpretation by a doctor of conjugated hyperbilirubinemia as “breastfeeding jaundice” or neonatal jaundice;
underestimation of the degree of lesions of the hepatobiliary system in identifying of hepatolienal syndrome and cholestatic jaundice;
lack of biochemical blood analysis monitoring of liver function tests in neonates among the primary health care specialists.
the late referral of children to specialist services, especially to children’s infectious disease doctor and to surgeon with the diseases of the liver and biliary tract;
If the jaundice continues after the child reaches the age of three weeks or it wavelike increases after its initial extinction, if there is a syndrome of cytolysis or cholestasis, it is necessary to conduct a more thorough examination of the child in a specialized hepatological reception. In order not to miss the formidable symptoms and to avoid possible errors, it is impractical to rely only on the experience and intuition, and it is necessary to use a clear algorithm of actions, which is adopted in the Protocol. The pediatrician must be able to assess an individual “safe” level of bilirubin in a newborn with jaundice and predict its potential growth using a modified scale of Kramer. For this, a physician should do the following:
to estimate the color of the skin;
to examine a fully naked child in good light (preferably daylight);
to provide the child with good thermal condition during the inspection;
to estimate the color of the skin after lightly pressing with a finger down to the level of the subcutaneous fat;
to determine the localization of jaundice according to the modified scale of Kramer.
Kramer modified scale is presented in figure 1.
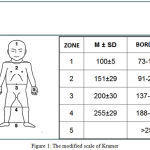 |
Figure 1: The modified scale of Kramer
|
Table 3: Assessment of the severity of detectable jaundice:
| Age (days) | Localization of jaundice | Conclusion |
| 1 | Any location | Dangerous jaundice |
| 2 | Limbs | |
| ≥3 | Foot, hands |
Conclusions
The implementation of a diagnostic algorithm in primary health care gives us an opportunity to discover the cause of the hyperbilirubinemia, the debut of hepatitis or biliary atresia. This helps to prevent bilirubin encephalopathy, make a diagnosis without a delay and to plan the further treatment and observation.
Reference
- Ushakova, R. A. Modern aspects of the development of prolonged jaundice in newborn infants. Bulletin of the modern medical academia 2010; 2: 33-36.
- Mamyrbaeva, M. A. To the monitoring of neonatal jaundice. Materials of the 1st national Congress of doctors of primary health care of the Republic of Kazakhstan within the framework 111 of the International Congress “Health for all. Equality, solidarity and social justice – the modern challenges of PHC”, 2014, pp. 73-76.
- Akhmedova, D. I. Clinical and diagnostic features of the major syndromes in children with in utero infection TORCH. Childhood infections 2009; 1: 29-31.
- Averyanova N.I. and Mekhryakova I. A. Communication conjugation of hyperbilirubinemia of newborns with perinatal risk factors. Issues of modern Pediatrics 2006; 1-5: 9.
- The clinical Protocol of diagnosis and treatment of neonatal jaundice. The Ministry of health of the Republic of Kazakhstan, minutes No. 1 of January 21, 2014.
- Zhumaaliyeva, G.D. and Mamyrbayeva, M.A. Infection and Incidence of Herpes Viruses in Neonates in Aktobe Region of Kazakhstan. Biol Med (Aligarh) 2016; 8: 333
- Mamyrbayeva, M., Igissinov, N., Zhumaaliyeva, G. and Shilmanova, A. Epidemiological aspects of neonatal mortality due to intra-terine infection in Kazakhstan. Iran J Publ health 2015; 44(10): 1322-1329
- Uchaikin, V.F., Cherednichenko, T. V. and Smirnov, A. V. The Infectious Hepatology:a guide for physicians. Moscow: GEOTAR – Media, 2012, pp.640.
- Degtyareva, A. V. Syndrome of cholestasis in newborns. Manual for doctors. Scientific center of obstetrics, gynecology and Perinatology V. I. Kulakov. Russian medical University. N. And. Pirogov, 2011, pp. 36.
- Amon, R. Neonatal Cholestasis: Textbook of Clinical Pediatrics. Berlin Heidelberg: Springer-Verlag, 2012, pp. 1987-2001.







